Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Sebastian Słomka1* and Piotr Lipiec2
Received: April 05, 2023; Published: April 18, 2023
*Corresponding author: Sebastian Słomka, Department of Internal Medicine and Geriatry, Bieganski Hospital, Medical University of Łódź , Kniaziewicza 1/5, 91-347 Łódź, Poland
DOI: 10.26717/BJSTR.2023.49.007863
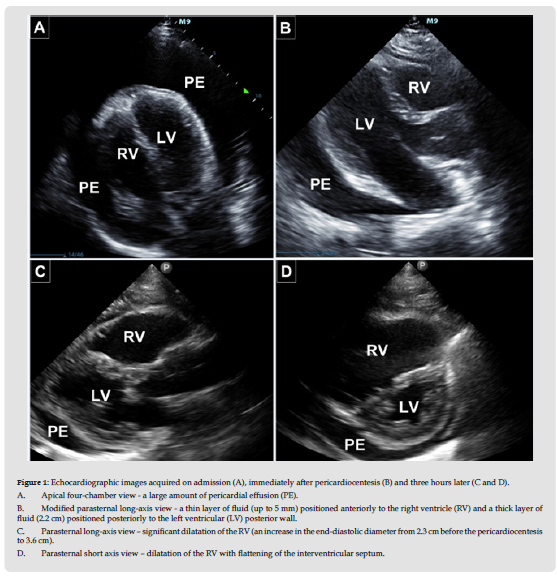
A 47-year-old patient with a history of alcoholism and smoking was referred to the department complaining of severe dyspnea at rest, progressing over the preceding week. On admission, tachycardia with respiratory variability of the pulse, decreased arterial pressure (90/55 mmHg) and respiratory variability of the ECG voltage were found. Cardiac tamponade was suspected, which was confirmed by bedside echocardiography - a significant amount of pericardial effusion (layer up to 3.6 cm), collapsing right atrial and right ventricular free wall, increased respiratory variability of the tricuspid and mitral inflows and the «swinging heart» sign were observed (Figure 1A). The patient underwent urgent pericardiocentesis, which resulted on obtaining about 800 ml of bloody fluid. Dyspnea at rest subsided, a decrease in heart rate to 85/min and an increase in blood pressure to 110/70 mmHg were observed. In the follow-up echocardiography after the procedure, a significant reduction in the amount of pericardial effusion was found (Figure 1B). The echocardiographic signs of tamponade were no longer present.
However, three hours later the patient reported a recurrence of severe dyspnea. Bedside echocardiography showed no increase in the amount of pericardial effusion. Nevertheless, signs of significant right-ventricular overload were noticeable (Figures 1C &1 D). In laboratory tests, an increase in troponin I from 6 ng/l to 881 ng/l and a significantly increased D-dimers level (12944 ng/ml) were observed. Pulmonary embolism was suspected, which was confirmed by pulmonary CT angiography, which revealed thrombi in the lower lobe branches of both pulmonary arteries. Ultrasonography of the veins of the lower limbs revealed thrombosis of the right femoral vein. The anticoagulative treatment was administered. The association between the pulmonary embolism and the cardiac tamponade was deemed not be direct causal, but we rather decided to look for a pathology that increases the risk of both of these complications. Therefore, the malignant tumor was suspected [1,2]. In the panel of biochemical markers, a significant increase in CA 125 (> 600.0 U/ml), CA 15-3 (> 200.0 IU/ml) and, to a lesser extent, elevated carcinoembryonic antigen (CEA) (4.9 ng/ml) were noted. In chest computed tomography, a nodular lesion up to 34mm in diameter was found in the left lung with an involvement of the pleura. In addition, there was a significant amount of fluid in the left pleural cavity. Pleurocentesis was performed and 2100 ml of bloody fluid was drained. All these findings were suggestive of non-small cell lung cancer. In the following days, the patient developed multiple organ failure and, despite treatment, died after 12 days of hospitalization. The post-mortem examination confirmed adenocarcinoma of the left lung involving the pleura and the pericardium.
Figure 1 Echocardiographic images acquired on admission (A), immediately after pericardiocentesis (B) and three hours later (C and D). A. Apical four-chamber view - a large amount of pericardial effusion (PE). B. Modified parasternal long-axis view - a thin layer of fluid (up to 5 mm) positioned anteriorly to the right ventricle (RV) and a thick layer of fluid (2.2 cm) positioned posteriorly to the left ventricular (LV) posterior wall. C. Parasternal long-axis view – significant dilatation of the RV (an increase in the end-diastolic diameter from 2.3 cm before the pericardiocentesis to 3.6 cm). D. Parasternal short axis view – dilatation of the RV with flattening of the interventricular septum.
None declared.


