Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Maria Fernanda Ortiz Jaramillo1*, Mary of the Sea Sáez of Ocariz1, John Charles Bustamante Ogando2, Robert Olives Roman3, Rodolfo Rodriguez Jurado3 and Carola Duran Mc Kinster1
Received: March 24, 2023; Published: April 13, 2023
*Corresponding author: Maria Fernanda Ortiz Jaramillo, Dermatology Service, National Institute of Pediatrics, Ecuador
DOI: 10.26717/BJSTR.2023.49.007848
Abbreviations: CTB: Cutaneous Tuberculosis; PPD: Purified Protein Derivative of Tuberculin; PIDs: Primary Immunodeficiencies; PCR: Polymerase Chain Reaction; CGD: Chronic Granulomatous Disease; ZN: Ziehl Neelsen; HIV: Human Immunodeficiency Virus; BCG: Bacillus Calmette-Guérin; ABAR: Acid-Bacilli Resistant Alcohol
Cutaneous tuberculosis (cTB) represents 1-2% of extrapulmonary tuberculosis [1] and is caused by the Mycobacterium tuberculosis complex (M. tuberculosis, M. bovis, M. africanum, M. microti, M. canetti, M. caprae, and M. pinnipedii). [2] The diagnosis of cTB is established by clinical signs, the presence of active TB in other organs, as well as the positivity of the purified protein derivative of tuberculin (PPD), the capacity to respond to antifungal drugs, the finding of tuberculous granuloma in the histopathological examination, the finding of some microorganism of the M. tuberculosis complex in a culture and/or the positive result in the polymerase chain reaction (PCR). Histopathological findings can be well-defined granulomas with or without caseous necrosis and ill-defined granulomas with intense caseous necrosis. [3] Primary immunodeficiencies (PIDs) have an approximate prevalence of 1 in 2,000 live births. [4] The most related to TB are severe combined immunodeficiency (CIDG) by the BCG vaccine, idiopathic CD4+ lymphopenia, chronic granulomatous disease (CGD), susceptibility mendeliana to mycobacteria, Di George syndrome, IL-12/23 axis defects, - IFN gamma, among others. [5,6] The relationship between immunological changes and tuberculosis lies in a reduction of CD3, CD4 and CD8. Cellular immunity plays a fundamental role in protection against tuberculosis infection. These modifications are related not only to the systemic deterioration caused by comorbidities or severity of the disease, but also by the infection itself.
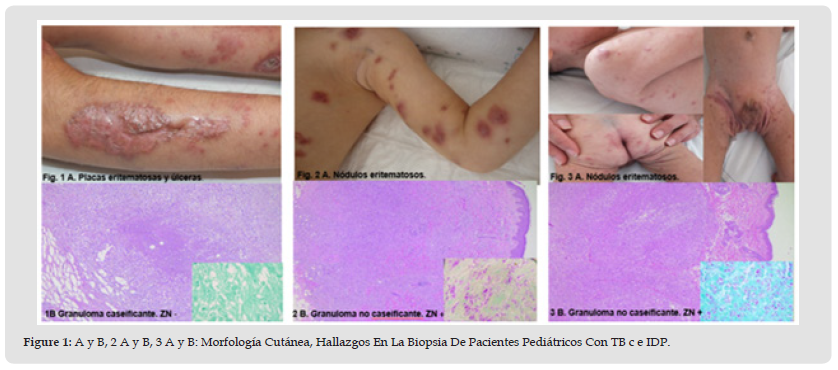
[7] TBc acquires several clinical aspects, which are generally related to the immune status of the host and the route of infection. In patients with immune deficiency, multibacillary forms can be seen, such as miliary TB and metastatic gummas; while immunocompetent patients present paucibacillary forms, such as verrucosa cTB and lupus vulgaris. Scrofuloderma, which is the most frequent cutaneous form, is observed in patients with intermediate resistance to the disease. [8] The purpose of this case report is to show that the histological finding of cutaneous tuberculosis with non-caseating granulomas presented a large number of acid-fast bacilli, unlike the caseating granulomas in which BARR staining was negative. Therefore, it must be taken into account that the presence of these bacilli may be much more predominant in non-caseating granulomas.
First Case: Female who at 5 years of age presented multiple episodes of airway infection and a disseminated dermatosis with infiltrated erythematous-scaly plaques and ulcers. SCID (RAG deficiency) and lupus TB were diagnosed. Skin biopsy reported granulomatous dermatopaniculitis with central caseous necrosis. Ziehl Neelsen (ZN) negative. He received antifungals (isoniazid, rifampicin, pyrazinamide, ethambutol) for 2 years with partial responses; in addition to thalidomide, gamma globulin subcutaneously and intravenously. He died at the age of 11 after complications of multifocal pneumonia and pulmonary hemorrhage.
Second Case: 6-month-old male, BCG vaccinated at birth, reports multiple respiratory infections, presented disseminated dermatosis characterized by multiple subcutaneous nodules.
Biopsy: non-caseating granulomas. ZN positive. Disseminated miliary TB and severe combined immunodeficiency (T-B+NK-) were diagnosed. He received a haploidentical hematopoietic progenitor cell transplant from a maternal donor with ex vivo depletion at 10 months of age, antiphimics (isoniazid, rifampicin, streptomycin, ethambutol) for 2 years, in addition to intravenous gamma globulin; with good response to treatment.
Third Case: One-year-old male, BCG vaccinated at birth, with a disseminated dermatosis made up of multiple erythematous nodules.
Biopsy: Non-caseating granulomatous dermatopaniculitis, ZN positive.
Diagnosis: disseminated miliary TB and severe combined immunodeficiency (TB-TB+NK-). He received antifungal treatment (rifampicin, ethambutol, clarithromycin, isoniazid, levofloxacin) for 2 years 9 months, intravenous and subcutaneous gamma globulin; in addition to transplantation of haploidentical hematopoietic progenitor cells from a maternal donor with ex vivo depletion, with a good response to treatment (Figure 1 & Table 1).
Figure 1 A y B, 2 A y B, 3 A y B: Morfología Cutánea, Hallazgos En La Biopsia De Pacientes Pediátricos Con TB c e IDP.
First documented in 1826 by Laennec, cutaneous TB accounts for only 1 to 2 percent of all cases.1 Like other forms of TB, a resurgence of cutaneous TB has been observed in parts of the world where the infection by the human immunodeficiency virus (HIV) and multidrugresistant tuberculosis are prevalent. [9] The high prevalence of tuberculosis worldwide, its transmissible nature, and the significant morbidity and mortality associated with this infection make TB a major public health problem. [10] M. tuberculosis is the most frequent causative organism of cTB. However, M. bovis and bacillus Calmette- Guérin (BCG) vaccine, a vaccine composed of attenuated M. bovis, have also been associated with the development of skin lesions. [1] Skin lesions are relatively uncommon manifestations of TB, occurring in only 1 to 2 percent of infected patients. The clinical findings vary, and may be Inflammatory papules, verrucous plaques, suppurative nodules, chronic ulcers or other lesions. Factors such as the route of bacterial entry into the skin, the immune status of the host, and the presence or absence of host sensitization to M. tuberculosis influence the morphologic presentation of TB on the skin. [9] Well-defined granulomas without caseous necrosis are seen preferentially in lupus TB and consist of foreign-body or Langhans-type giant cells. Welldefined granulomas with caseous necrosis are seen in verrucosa cutis, acute miliary, orificial, papulonecrotic TB. [3] Ill-defined granulomas with intense caseous necrosis are typical of colliquative TB, where massive central necrosis is observed with abscess formation and, in many cases, suppuration.
[3] In the cases presented, 2 types of histological patterns were identified, slightly different from what is reported in the literature. In case 1 the classic pattern was identified, characterized by a granuloma with caseous necrosis although with negative ZN, while cases 2 and 3 showed granulomas with many scattered histiocytes that corresponded to a non-caseating granuloma and a ZN with countless acid-bacilli. resistant alcohol (ABAR), which indicates that the presence of bacilli can be much more identifiable in this type of pattern and not in the classic pattern as would be expected. It was also striking that these patients were cases of disseminated BCG, but with clinical manifestations of lupus TB and miliary TB.
The cases reported by those who received the BCG vaccine corresponded to BCGosis or disseminated BCG disease. It is important to insist on not applying the vaccine until the child’s immune status is known, to avoid complications that can be fatal. The histopathological findings in all clinical forms of cTB presentation are similar in terms of the presence of an inflammatory infiltrate made up of lymphocytes, epithelioid histiocytes, and giant cells. Histological differences will depend on the immune response that may generate variations in the host’s ability to organize the granulomatous process. This article aims to demonstrate the 2 types of granulomas found in cutaneous tuberculosis, but above all that the classic pattern (caseating granulomas) is not always the one that presents a large number of acid-resistant bacilli, but non-caseating granulomas such as in the 2 cases described.


