Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Mehmet Özdin1 and Hayrullah Yazar2*
Received: March 13, 2023; Published: April 04, 2023
*Corresponding author: Sakarya University Faculty of Medicine, Medical Biochemistry Department, Turkey
DOI: 10.26717/BJSTR.2023.49.007820
Introduction: In this study, the files of discharged and deceased patients were reviewed retrospectively,
taking into account age and gender. Our aim; is to determine the insulin resistance of all patients by calculating
the insulin and fasting blood glucose values and homa indexes in the blood serum.
Methods: Obtained the information of the patients included in the study through the Hospital Information
Management System (HIMS). Considering the age and gender information of discharged and deceased
patients, fasting blood glucose (mg/dL), evaluated insulin (μU/mL) and Homa-index data statistically. In the
study, patients with a HOMA index of ≥2.7 were considered positive for insulin resistance (IR). Obtained
approval of the study from the Sakarya University Ethics Committee (date and number: 03.05.2019, E.5229).
All results were presented as mean ± standard error of the mean (SEM). Statistical comparisons were made
using SPSS 19.0 statistical software (SPSS, Inc., Chicago, IL). For all statistical tests, p<0.05 was considered
statistically significant.
Results: When comparing parameters according to death or discharge status, the glucose levels of the
deceased were found to be significantly higher than those who were discharged. Detected no significant
difference in insulin and homa index. There was a correlation between Homa index, insulin and glucose, as
expected. While there was an important negative relationship between age and insulin (as one increases, the
other decreases), there is a significant positive relationship between age and glucose (as one increases, the
other increases). When evaluated only by gender, it found Homa-index and insulin were significantly higher
in females than in males (discharged and deceased patients together). In those discharged, found insulin and
Homa-index values of females were to be significantly higher than in males. However, found no significant
difference in males and females in deceased patients.
Conclusion: Notably, in all patients who deceased and were discharged, the homa-index and insulin levels
were significantly higher in females than in males. On the other hand, researching this fact with more
comprehensive studies will positively contribute to clinicians in their approach to patients with suspected
insulin resistance.
Keywords: Homa-Index; Glucose; Insulin; Age; Gender; Discharged Patient; Deceased Patients
Abbreviations: CVD: Cardiovascular Diseases; MetS: Metabolic Syndrome; IR: Insulin Resistance; DM: Diabetes Mellitus; TyG: Triglyceride-Glucose Index; HIMS: Hospital Information Management System; HOMA-IR: Homeostatic Model Assessment Insulin Resistance; DiscP: Discharged Patients; DecP: Deceased Patients
Considering that cardiovascular diseases (CVD) are prominent in morbidity and mortality worldwide, it is, of course, essential to investigate the role played by metabolic syndrome (MetS). Therefore, research on metabolic diseases has increased exponentially in the last decade. However, many aspects of this clinical indicator still need to be fully understood (Fahed G, et al. [1]). Insulin resistance (IR) is a significant clinical problem that needs to be addressed in this context. In addition, if specified, IR is an issue that needs to be addressed more seriously in women than in men. Because large-scale studies on women with a history of pregnancy with IR have shown that; recurrent pregnancy loss is highly associated with IR (Cai WY, et al. [2]). It is known that a group of risk factors, including IR and diabetes mellitus (DM), cause higher mortality rates. Metabolic disorders are among the main reasons for this, and lifestyle changes are considered in addition to existing treatment options (Gluvic Z, et al. [3]). In addition, studies investigating the effects of COVID-19 infection, especially in recent years, have shown that; IR increases the risk of death in patients with metabolic problems (Govender N, et al. [4]).
Although the relationship between IR and MetS is accepted, there are different approaches to this issue. For example, the triglycerideglucose index (TyG) was shown to have higher predictive power than Homa-IR in a large-based, prospective cohort study with 12 years of follow-up on the close association of IR with MetS (Son DH, et al. [5]). In our study, besides Homa-IR, we analyzed glucose and insulin values in blood serum retrospectively. In our study, we retrospectively analyzed the glucose and insulin values in blood serum as well as Homa-IR. The information of the discharged and deceased patients were recorded using HIMS. Moreover, the age and gender information of the discharged and deceased patients were also recorded with HİIMS. Because as seen in hospital discharge and mortality studies, age, gender, and frequency of admission were taken into account (Heppleston E, et al. [6,7]). In this respect, our study is compatible with the literature.
Study Population
Approval of the study was obtained from the Sakarya University Ethics Committee (date and number: 03.05.2019, E.5229). The study received patient information retrospectively from HIMS, and deceased and discharged patients were evaluated separately.
Protocol Study Procedures
In the patient files, age, gender, and fasting determined blood glucose and serum insulin values. While receiving these data, The deceased and discharged patients were evaluated separately. Subsequently, the Homa-index values for IR were calculated as Fasting Glucose(mg/dL) fasting Insulin (μU/mL)/405. In the study, the IR of patients with a Homa-index value ≥2.7 was considered positive.
Biochemical and Hormonal Assays
Insulin (μU/mL) was measured by the chemiluminescent microparticle enzyme immunoassay (CMIA) method (ARCHITECT, Abbott Laboratories). The precision of the ARCHITECT Insulin study was determined to be ≤7% complete CV, with a sensitivity better than 1.0 μU/mL. Glucose (mg/dL) was determined quantitatively by enzymatic UV test using the hexokinase method (Beckman Coulter AU5800). The test linearity was in the concentration range of 10-800 mg/dL, while the lowest detectable level for its sensitivity was 0.04 mmol/L.
Statistical Analysis
All results were presented as mean±standard error of the mean (SEM). Statistical comparisons were made using SPSS 19.0 statistical software (SPSS, Inc., Chicago, IL). For all statistical tests, p<0.05 was considered statistically significant.
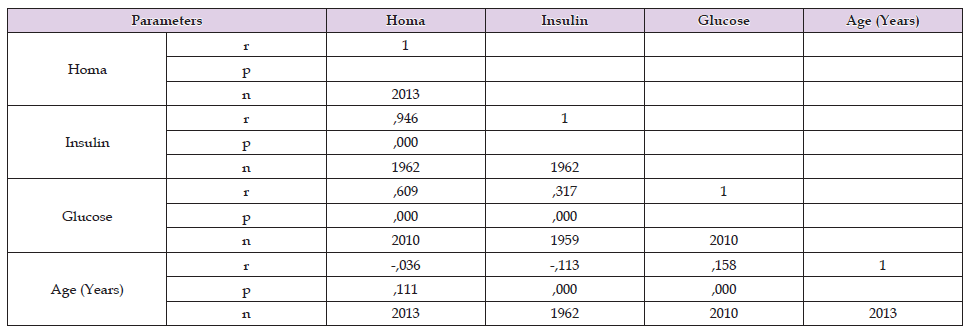
According to the data obtained, Since the Homa index, insulin, and glucose are parallel parameters, correlations were seen between them. There was a significant negative relationship between age and insulin (as one increases, the other decreases) and a meaningful positive relationship between age and glucose value (as one increases, the other increases) (Table 1). In comparing parameters according to death or discharge, Glucose levels of those who died were found to be significantly higher than those those who were discharged. No significant difference was found in the insulin and the homa index (Table 2). When the deceased or discharged persons are evaluated according to their genders, the Homa index and insulin were found to be significantly higher in females than in males (Table 3). However, no significant difference was found between men and females in the parameters measured in the deceased (Table 4). On the other hand, Insulin and Homa index levels of discharged female were found to be significantly higher than men (Table 5).
Table 1. Correlation findings between Homa, insulin, glucose and age parameters Since insulin and glucose are parallel parameters, they are correlated.
Note: DiscP: discharged patients, DecP: deceased patients, SEM: standart error of the mean. SD: standard deviation. In comparing parameters according to death or discharge status, the glucose levels of the deceased were found to be significantly higher than those who were discharged (p<0.05).
Note: According to the genders, homa index and insulin were significantly higher in females than in men (p<0.05). SD: standard deviation, SEM: standart error of the mean.
Note: No significant difference was in the parameters measured in the deceased in males and females (p>0.05).
Note: Insulin and homa index values of discharged females were found to be significantly higher (p<0.05).
Hyperglycemia emerging after IR emerges as an important public health problem because; The mean prevalence of MetS is shown as 31%. MetS, if additionally specified, coronary heart disease is associated with a two-fold increase in the risk of cerebrovascular disease and a 1.5-fold increase in the risk of death from all causes (Engin A [8]). Although MetS examination was not performed in our study, the detection of IR in deceased and discharged patients, taking into account gender and age, is an essential similarity with their research. The fact that the mortality rate was significantly higher in women in our study made us think that the incidence of IR and obesity may differ according to gender. In a study, it has been stated that the pathophysiology and management of obesity and visceral fat deposition in women are different from men (Kapoor E, et al. [9]). Again, regarding the IR treatment process, it is a health problem emphasized more carefully for all clinicians, especially women with a pregnancy history (Cai WY, et al. [2]). As a matter of fact, in our study, the fact that the IR was higher in women was found to be even more critical in this respect because other studies have emphasized the progression of insulin resistance during pregnancy in women (Tarasenko KV, et al. [10]). Studies have shown that obesity is an essential factor in the development of IR (Barazzoni R, et al. [11]). In addition, to mention; Obesity-related, therefore IR-related morbidity and other complications should be evaluated from this perspective.
Vascular surgery patients were examined in a study on the consequences of malnutrition on morbidity and mortality (Von Meijenfeldt GCI, et al. [12]). According to them, dietary guidance can benefit nutritional status and positively affect mortality. The relationship between IR, the subject of our study, and nutrition can be evaluated in this respect. In the study titled «transient blood lipid array and insulin resistance in perimenopausal women», whose mean age is consistent with our study, 1386 women (mean age 46.4 years) were examined (Yu W, et al. [13]). Their study also used Homa-Ir for insulin resistance. According to the results they obtained, they found a bidirectional relationship between lipids and insulin resistance. In our research, It is noteworthy that in all patients who died and were discharged, the homa and insulin levels were higher in women than in men. Homa-Index and blood inulin values were significantly higher in females than males. On the other hand, this may be related to the prevalence of obesity and lifestyle differences in women. In this respect, it is evident that the resulting result needs more extensive research.
Yıldırım KAYACAN. Yasar Dogu Faculty of Sports Sciences, Ondokuz Mayıs University, Samsun, Türkiye.
No financial support was used for this study.
All authors declare having no conflicts of interest.


