Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Rivas Treviño Alejandra1, Flores Hernández José Gabriel1*, Nieto Romero Adrián1, Quintero Mosqueda Rafael2 and González Magaña Fernando3
Received: March 15, 2023; Published: April 03, 2023
*Corresponding author: Jose Gabriel Flores Hernandez, Centro Médico Issemym Lic Arturo Montiel Rojas, Cirugía plástica y reconstructiva, Mexico
DOI: 10.26717/BJSTR.2023.49.007816
Introduction: Pseudoaneurysms of the maxillary artery and its branches are a rare complication after Lefort I osteotomy and can lead to life-threatening hemorrhage, however, the typical clinical presentation, diagnosis and treatment are not well characterized.
Objectives: To describe the clinical presentation, diagnosis, and treatment modalities of pseudoaneurysm of the maxillary artery and its branches after Lefort I osteotomy and to report a new case.
Clinical Case: A 31-year-old patient with a diagnosis of anteroposterior deficiency of the midface, left laterognathia and Angle class III malocclusion treated with Lefort I osteotomy who presented rupture of a pseudoaneurysm of the right maxillary artery confirmed by angiography and successfully treated by selective transcatheter angioembolization.
Conclusion: A high clinical suspicion of pseudoaneurysm of the maxillary artery and its branches should be maintained in the case of persistent or recurrent epistaxis, especially when it occurs 14 days after the Lefort I osteotomy or when significant bleeding causes hemodynamic instability. An angiography and selective transcatheter angioembolization are recommended once the diagnosis is confirmed.
Keywords: Pseudoaneurysm; Maxillary Artery; Lefort I Osteotomy; Orthognathic Surgery; Angioembolization
The Lefort I osteotomy is a technique widely used in orthognathic surgery for the correction of dento-skeletal deformities that affect the midface. It is considered a safe procedure, however, serious complications (<1% of cases) can develop after unrecognized intraoperative vascular injury, such as hemorrhage, arteriovenous fistulas or pseudoaneurysms (PA), which represent a lifethreatening disease and a diagnostic-therapeutic challenge for the craniomaxillofacial surgeon [1]. Recognizing the clinical presentation of PA rupture will provide a basis for evaluation, detection, and treatment prior to massive hemorrhage. We present the case of a 31-year-old woman who developed a ruptured pseudoaneurysm of the right maxillary artery as a complication of a Lefort I osteotomy. The clinical presentation, diagnostic methods, and treatment options are also discussed.
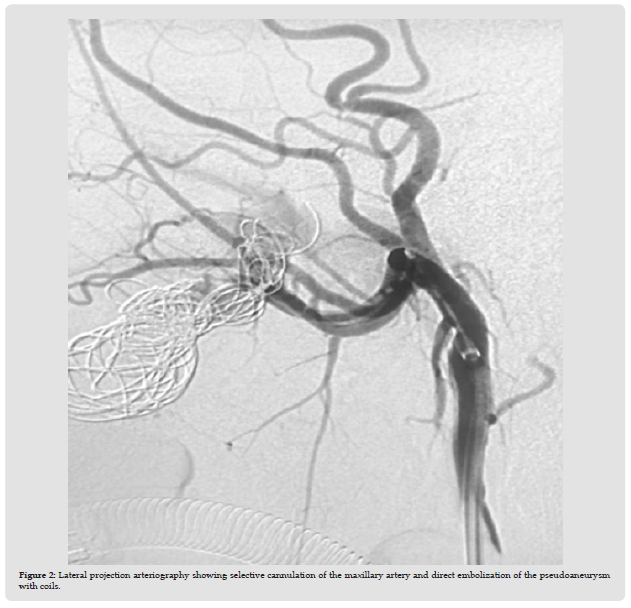
A 31-year-old female patient with a diagnosis of anteroposterior deficiency of the midface, left laterognathia and Angle class III malocclusion treated by high Lefort I osteotomy with 4 mm advancement and impaction. After performing the down fracture, he presented trans-surgical bleeding of 2,500 cc which was controlled by packing with hemostatic material and transfusion of two packed red blood cells. She was later transferred to the intensive care unit where she remained hospitalized for five days. Two weeks after the surgical event, he went to the emergency department after presenting an episode of epistaxis which resolved spontaneously. Eight days later, he presented a new episode of epistaxis which was controlled with anterior nasal packing. Fourteen hours later, he presented an episode of massive epistaxis and grade III hypovolemic shock that required anterior nasal packing and transfusion of two packed red blood cells. Angiography of the external carotid artery revealed a pseudoaneurysm of the right maxillary artery of approximately 2 cm (Figure 1), which was successfully angioembolized (Figure 2). The patient was discharged after a 72-hour hospital stay. During outpatient follow-up, there were no new episodes of epistaxis.
Figure 1 Anteroposterior projection arteriography showing a 2 cm aneurysmal sac directly dependent on the right maxillary artery.
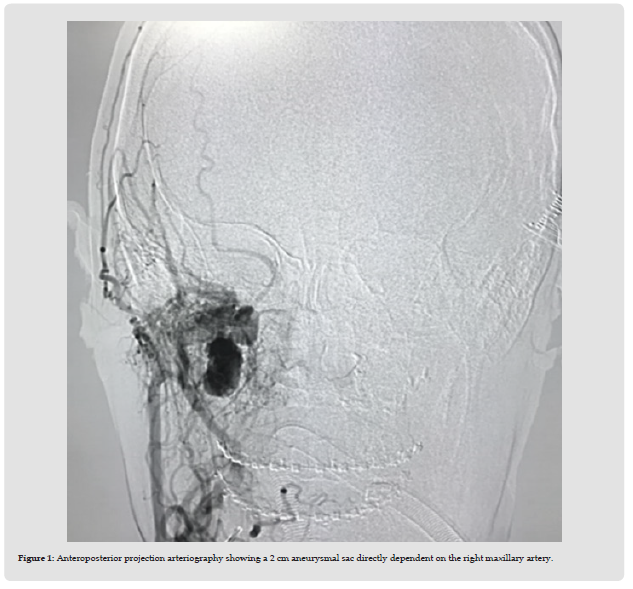
Figure 2 Lateral projection arteriography showing selective cannulation of the maxillary artery and direct embolization of the pseudoaneurysm with coils.
A PA is usually the result of an incomplete tangential tear of the arterial vessel wall, so that continuity of blood flow through the lacerated artery is maintained. Laceration of the vessel causes bleeding into the surrounding soft tissues until a hematoma forms, stopping the bleeding. Over the next 8 weeks, the hematoma organizes by creating a sac around which an endothelial lining forms to produce a pseudointima that remains in continuity with the arterial lumen. With liquefaction of the hematoma, a communication develops between the artery and the aneurysmal sac, resulting in a pulsatile mass. Blood pressure leads to gradual expansion of the PA, which can progressively rupture or grow and put pressure on nearby nerves. Due to this pathophysiology, our patient and most of the cases reported in the literature present intermittent epistaxis 1 to 8 weeks after surgery [1-4].
PA rupture after Lefort osteotomy is an extremely rare but lifethreatening complication. To date, 20 cases have been reported in the literature [4-8]. Injury to the maxillary artery and its branches occurs especially in the pterygopalatine fossa, when the maxillary tuberosity and pterygoid plates are osteotomized, during the down fracture or due to a bone spur after osteotomy. The vessels with the highest risk of injury during the Lefort I osteotomy are the maxillary artery (38.9%) and the sphenopalatine artery (38.9%), followed by the descending palatine artery (16.7%) and the internal carotid artery (5.6%) [9].
Risk factors that have been associated with vascular lesions and the development of late AP after Le Fort I osteotomy are intraoperative bleeding greater than 500 ml, craniofacial and vascular malformations, previous maxillofacial surgeries, and anatomical changes [9]. AP of the maxillary artery and its branches may be asymptomatic or present clinically with nonspecific signs and symptoms. PA enlargement without rupture can cause facial asymmetry, pain, and paresthesias from nerve compression. PAs in other areas of the body present as a pulsatile mass or bruit, however these signs may be absent in PAs of the maxillary artery and its branches as palpation and auscultation become difficult due to its deep location. in the craniofacial skeleton, although in some cases, the patient can feel or hear the pulsations. PAs can progressively enlarge until they rupture, manifesting with multiple episodes of epistaxis that worsen over time or with massive epistaxis that causes hemodynamic instability. On average, most episodes of epistaxis occur 2 weeks after the osteotomy, and the volume of bleeding increases progressively over time [5-6,9].
The number of reported cases of this complication is not sufficient to establish guidelines for the diagnosis and treatment of AP of the maxillary artery and its branches after Lefort I osteotomy, which is why they can remain undiagnosed for weeks or months. Often, it is misdiagnosed until an episode of massive epistaxis occurs. The goal of early diagnosis of an AP is to treat it in a timely manner to avoid life-threatening complications. Angiography can locate the actual site of bleeding, helps delineate the development of collateral blood flow, and whether the contralateral arterial tree is contributing to the problem, allowing for precise treatment. Even if embolization is unsuccessful, the surgical procedure can be carefully planned and safely performed using the vascular map obtained from the angiogram [1-2,9] Angiography is recommended in patients with persistent or recurrent epistaxis presenting after the second postoperative week or who experience significant bleeding causing hemodynamic instability.
Three different forms of treatment have been described for rupture of a PA of the maxillary artery and its branches:
1. Non-Surgical Treatment: control of blood pressure, administration of intravenous fluids and blood products. Anterior and/or posterior nasal packing is usually temporarily effective in cases of mild epistaxis [10].
2. Open Surgical Repair: Bleeding can be controlled by electrocoagulation or direct ligation of the bleeding vessel; however, identification of the vessel is not always possible due to the large amount of blood or retraction of the vessel into an inaccessible cavity. In these cases, packing, placement of topical hemostatic agents or ligation of the internal carotid artery should be performed, proximal and distal to the origin of the pseudoaneurysm followed by en bloc resection [3].
3. Transcatheter Angioembolization (treatment of choice): One of the advantages of angioembolization over surgical intervention is that the more distal vessels originating the source of bleeding can be selectively embolized while sparing the more proximal vessels [6]. This is particularly important after the Lefort I osteotomy where wishes to preserve the vascular supply of the osteotomized segments and thus avoid aseptic necrosis of the maxilla [9]. Complications of angioembolization include intraoperative rupture of the pseudoaneurysm, embolic phenomena to the brain due to thrombi from the pseudoaneurysm cavity or embolization material, ischemic necrosis of the maxilla and tooth loss [3].
Understanding the typical clinical presentation of AP rupture of the maxillary artery and its branches after a Lefort I osteotomy will allow diagnosis and treatment before life-threatening bleeding occurs. Angiography is recommended for persistent or recurrent epistaxis, especially when presenting 14 days after the Lefort I osteotomy or significant bleeding causing hemodynamic instability, and angioembolization once the diagnosis is confirmed.


