Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Kartik Bhagat* and Rhea Potdar
Received: March 15, 2023; Published: March 27, 2023
*Corresponding author: Kartik Bhagat, Tbilisi State Medical University, Georgia
DOI: 10.26717/BJSTR.2023.49.007799
The case report consists of a mixed pathology in the vein of Galen complex - a Galenic malformation with its own aneurysm. Furthermore, the aneurysm was seen to have its own diverticulum. Investigations included multiple imaging modalities to yield the final diagnosis of the patient. A carefully curated approach to treatment and a safe recovery of the patient has been followed in the report. Differential diagnoses may include but are not limited to cerebral venous thrombosis and intracranial hemorrhage. The age group in which the malformation arises is important with respect to the outcome. Infants and children with the diagnosis have a more optimistic prognosis compared to neonates as they have a higher likelihood of developing heart failure. In conclusion, the rarity of the case stems from the presence of a mixed pathology and warrants a very intricate understanding of neuroanatomy.
Keywords: Vein of Galen; Malformation; Intranidal; Aneurysm; Diverticulum; Endovascular; Embolization; Mixed Pathology
Abbreviations: VoGM: Vein of Galen Malformation; VoGAM: Vein of Galen Aneurysmal Malformation; AVMs: Arteriovenous Malformations; HR: Heart Rate; BP: Blood Pressure; Temp: Temperature; RR: Respiratory Rate; CT: Computed Tomography; MRA: Magnetic Resonance Angiography; DSA: Digital Subtraction Angiography
Brain AVMs are a leading cause of hemorrhage in children and adults. Vein of Galen Malformations are usually diagnosed in infancy or early childhood and differ from Vein of Galen Aneurysmal Malformations. But the case at hand is neither a VoGAM nor a simple VoGM. Here we see a saccular aneurysm arising on a Galenic malformation; complicated with an aneurysmal diverticulum - the most likely source of the bleed. The case is a culmination of different vascular pathologies - a so called ‘mixed pathology’. The choice of treatment in such cases is of great importance and interest to not just neurosurgeons, but doctors in general; globally. The overall mortality in brain AVMs is 0.7 to 2.9% per year [1]. Brain arteriovenous malformations (AVMs) are comprised of a complex tangle of abnormal blood vessels called the nidus, not clearly an artery or a vein and lacking a true capillary bed [1]. There is usually high flow through the feeding arteries, nidus, and draining veins (with increased pressure on the venous side), which may result in rupture and intracranial hemorrhage [1]. The hallmark feature is shunting of blood directly from the arterial to venous circulation [1]. In Galenic malformations, the cardiovascular system takes a toll; and clinically, its relevance is seen when the patient presents with signs of heart failure [2] due to higher-than-normal pressures and flow draining into the jugular systems (Figures 1-6).
A 9 y/o Georgian male was presented to the ER with sudden, unbearable headache and blurry vision; positive meningeal signs were noted along with nuchal rigidity. No past relevant history was noted. Vital signs: HR – 99 bpm, BP – 100/70 mmHg, RR- 23 breaths/min, Temp – 37.1oC. At imaging, a head CT showed an intraparenchymal hemorrhage. MRA confirmed the presence of a vascular pathology, followed by a DSA, which showed a vein of Galen malformation with an intranidal aneurysm. Furthermore, the aneurysm was found to have a diverticulum – the most likely source of the bleed. Images of all imaging modalities are attached below.
Table 1: Spetzler-Martin Scale –
Lower score (1-3) = Better outcome
Higher score (4-5) = Worse outcome and warrants least invasive
procedures.
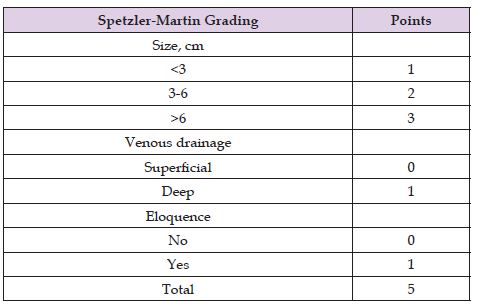
Currently, three treatment options exist for brain AVMs, namely – microsurgery, endovascular embolization, and radiosurgery. An endovascular surgical approach was preferred, and the aneurysm was treated using platinum coils. The AVM remnants were embolized using Histoacryl glue. Hypotensive drugs were used for the first 24 hours post-op to maintain normovolemia and normotension. On recovery, the patient was seen to have a modified Rankin Score of 0 (Table 1).
According to Martin M Mortazavi and co-authors, “Offering the best treatment option is dependent on an understanding of the aberrant anatomy and pathophysiology of these entities, and tailored therapy is recommended” [3]. In accordance with the above statement, the patient was treated using an endovascular embolization not just due to the presence of a VoGM, but also the complex angioarchitecture of the pathology involving an intranidal aneurysm (with a diverticulum), highlighting the rarity of the case. Patients are advised to have MRA and DSA scans done at the 1st, 3rd, and 5th years post-op.
We’d like to thank Dr. Erekle Ekvtimishvili affiliated with the High Technology Medical Center, University Clinic, Tbilisi, Georgia for helping us with our case report.
Kartik Bhagat and Rhea Potdar declare that they have no conflict of interest.


