Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Shiomi Ushida1, Satoshi Ichigo1, Hiroshi Takagi1, Kazutoshi Matsunami1, Yuji Ito2 and Atsushi Imai1*
Received: February 20, 2023; Published: March 17, 2023
*Corresponding author: Atsushi Imai, Department of Obstetrics and Gynecology, Matsunami General Hospital, 185-1 Dendai, Kasamatsu, Gifu 501-6062, Japan
DOI: 10.26717/BJSTR.2023.49.007782
High-grade endometrial stromal sarcomas (HG-ESS) are rare tumors of endometrial stromal origin and occur primarily in perimenopausal women. They are extremely uncommon in adolescents and young adults. Due to the rarity of this tumor, there are limited reports in the literature referring to the clinical manifestation and diagnostic images. We report a case of HG-ESS in a 26-year-old nulligravida woman, who initially experienced abnormal uterine bleeding and acute abdomen, and also review the reported cases of HG-ESS in adolescents and young adults. Our patient’s magnetic resonance imaging and contrast-enhanced computed tomography of the abdomen demonstrated a prominent irregular tumor (5cm x 10cm x 6cm) causing the endometrial cavity to expand and diffuse peritoneal and omental implants. Total abdominal hysterectomy with bilateral salpingo-oophorectomy, omentectomy, and elective lymphadenectomy were performed. We made a diagnosis of stage IIIc HG-ESS, and adjuvant chemotherapy followed. The HG-ESS is a very rare disease. The dismal prognosis of this disease prompted us to keep the high degree of suspicion for HG-ESS while working up any case of abnormal uterine bleeding and abdominal pain.
Abbreviations: HG-ESS: High-Grade Endometrial Stromal Sarcomas; MRI: Magnetic Resonance Imaging; CT: Computed Tomography; ER: Estrogen Receptor; PR: Progesterone Receptor
Endometrial stromal sarcoma (ESS) is a rare tumor originated from endometrial stroma and accounts for <0.2% of all uterine malignancies [1,2]. It affects a younger group, and the mean age is between 42 and 58 years. Approximately 15% of affected women are premenopausal. High-grade ESS (HG-ESS) is seen in the older age group, with a mean age of around 60 years and is usually very aggressive [3,4]. It is extremely rare for HG-ESS to be diagnosed in adolescents and young woman (Table 1). The prognosis of HG-ESS in this subset of women is generally poor due to its rapid progression and the disease presenting at a later stage. We aimed to review accumulated reports of this clinical entity, and include a current case of HG-ESS in a 26-old-year woman who presented with abnormal uterine bleeding and acute abdomen.
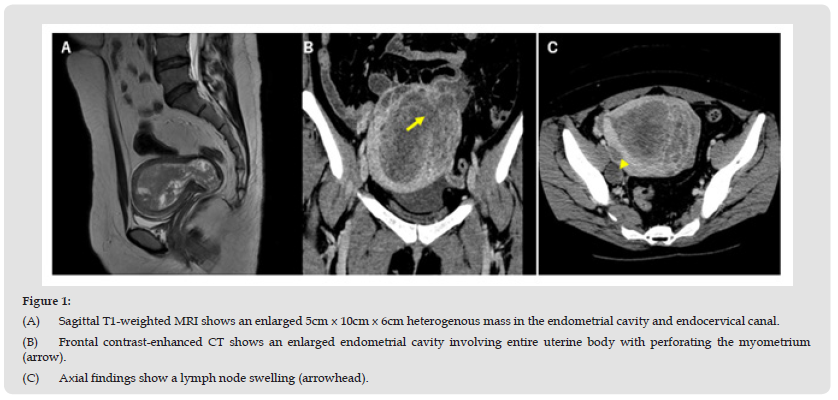
Figure 1 (A) Sagittal T1-weighted MRI shows an enlarged 5cm x 10cm x 6cm heterogenous mass in the endometrial cavity and endocervical canal. (B) Frontal contrast-enhanced CT shows an enlarged endometrial cavity involving entire uterine body with perforating the myometrium (arrow). (C) Axial findings show a lymph node swelling (arrowhead).
A 26-year-old nulligravida woman complained of a 4-month history of excessive and prolonged vaginal bleeding and a palpated mass at the lower abdomen. Three months before this visit, she had presented to a local physician with symptoms of severe anemic and vaginal spotting. Her past medical history was unremarkable.
On gynecological examination, a cauliflower-like growth of about 2cm was seen from the endocervical canal. The exophytic polypoid mass was friable and bled when touched. A biopsy of the mass was performed to obtain tissue for further histopathological study. Magnetic resonance imaging (MRI) revealed an enlarged, well-defined uterine border with heterogeneously thickening in the endometrial cavity involving entire uterine body and cervix (Figure 1A). The histopathological examination showed the possibility of endometrial stromal sarcoma with heterogenous elements of leiomyosarcoma. Immunohistochemistry revealed positive diffuse staining for CD10, cytokeratin AE1/AE3 and SMA, while the tumor cells were negative for desmin, CD45, S100P and p40. The final diagnosis was most suggestive of high-grade ESS. During a 1month consideration with her partner on the diagnosis of a high-grade ESS and life-threatening situation, the patient developed sudden onset of acute abdomen and, with a progressively distended abdomen. Her contrast-enhanced computed tomography (CT) of the abdomen revealed a prominent irregular tumor causing the endometrial cavity to expand and diffuse peritoneal and omental dissemination (Figure 1B). Pelvic lymph node metastases were also present (Figure 1C).
She was submitted to emergency laparotomy. At surgery, the tumor was diffusely spread throughout the pelvis and upper abdomen and the omentum, that could be responsible for the pain. The uterine serosa was diffusely involved and contained multiple tumor plaques. The surgical procedures included total abdominal hysterectomy, bilateral salpingo-oophorectomy, partial omentectomy, and resections of enlarged pelvic lymph nodes. The postoperative period was uneventful, and her final histopathological report was high-grade endometrial stromal sarcoma with more than 10 mitosis/10 highpower field. Sections of the omentum revealed multiple metastatic foci. Additional immunohistochemistry studies revealed positive diffuse staining for CD34 and vimentin. The tumor stained negative for estrogen receptor (ER), progesterone receptor (PR), Melan A, HMB45, Synaptophysin, Chromogranin A, CD56, c-kit and EMA. We made a diagnosis of stage IIIC high-grade endometrial stromal sarcoma on theses examination results. Psychological support was provided. The patient started adjuvant chemotherapy consisting of adriamycin (30mg/m2) for days 1-3 given every four weeks.
The ESS only affects women in the second half of their reproductive life [1,2]. The incidence of HG-ESS is rare, and it is extremely uncommon in adolescents and young women [3,4]. Because of the low incidence of HG-ESS, there is lack of specific clinical manifestation and the imaging features. A literature review found eight single case reports of highgrade endometrial stromal sarcoma in adolescents and young adults (Table 1). They often show abnormal uterine bleeding, abdominal pain (acute abdomen) and pelvic mass. All previously reported cases are in advances (stages III and IV) at the time of initial diagnosis. Three cases have been reported in teenage girls [5-7]. One of them had her menarche at the age of 14 years and oral contraception at the age of 15 years [9]. HG-ESS have a significantly different biological features from LG-ESS: low-grade ESS may represent estrogen-dependent while HG-ESS arising in adolescents is still under investigation [8]. Transvaginal ultrasonography and endometrial curettage can be helpful in diagnosing endometrial polyp, uterine leiomyoma or adenomyosis but are unpredictable in diagnosing ESS. MRI may also detect it by the presence of heterogenous areas within the lesion of myometrial invasion due to aggressive tumor permeations. Taken together with contrast-enhanced CT, they can be used for the preoperative diagnosis of the possible extent like in the current case. On microscopic observation, immunohistochemistry is particularly helpful to obtain the definitive g diagnosis. The immunohistochemical markers such as h-caldesmon and CD-10 may solve the diagnostic problem as CD staining is positive in ESS but not in leiomyosarcoma. We included CD-10 staining to establish the diagnosis.
The treatment includes debulking surgery followed by total hysterectomy with bilateral salpingo-oophorectomy and omentectomy [1,9,10]. The role of pelvic and para-aortic lymphadenectomy remains controversial [11]. Because HG-ESS has the high risk of recurrence and metastasis, postoperative adjuvant therapy plays a critical role. Up to now, chemotherapy and pelvic external radiotherapy has been widely used as an adjuvant therapy for HG-ESS. In particular, anthracyclines have a specific capacity against sarcoma. Amant, et al. [12] described the case of transperitoneal HG-ESS complicating pregnancy (15 weeks). They explored all possibilities to maintain the pregnancy, including antracyclin-base chemotherapy and cytoreductive surgery, even during pregnancy. She finally succumbed to the disease six weeks after diagnosis [13-16]. In summary, we described the clinical findings and imaging of a rare case of HG-ESS affecting a 26-yearold woman. Although the patient is still under intensive adjuvant chemotherapy, the dismal prognosis of this disease prompted us to r keep the high degree of suspicion for HG-ESS while working up any case of abnormal uterine bleeding and abdominal pain.
The authors declare that they have no conflict of interest.


