Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Shambel Abate Kebede1*, Sara Muhammed Siraj1, Natnael Dechasa Gemeda1, Berhanu Abebaw2, Abdu Oumer Abdu1, Yeshalem Mulugeta2, Teshale Mengesha Sasiga1 and Yomilan Geneti Muse1
Received: February 22, 2023; Published: March 15, 2023
*Corresponding author: Shambel Abate Kebede, Dire Dawa University, Dire Dawa, Ethiopia
DOI: 10.26717/BJSTR.2023.49.007777
Background: Diabetes mellitus is a chronic disease with a high prevalence and a growing concern worldwide. Dietary management is considered to be one of the cornerstones of diabetes care. There is a lack of data on the dietary pattern of diabetic patients, which underestimates its role in the management of diabetes. Information concerning the dietary pattern among type 2 diabetic patients is limited though the prevalence of DM and its complications are on the rise. there is no recent study conducted about dietary pattern and associated factors in the study area, so this study will fill this gap.
Objective: The objective of the study was to assess the dietary pattern and its associated factors among type 2 diabetes mellitus patients in Felege Hiwot Comprehensive Hospital.
Methods: Institutional based cross-sectional study was conducted among type 2 diabetes patients from March 2021 to May 2021. Systematic sampling technique was used to select the study participants. A binary logistic regression model was fitted to determine independent predictors of dietary pattern among Type 2 DM patients. Adjusted odds ratio at 95%CI and p value of 0.005 was used to declare statistically significant association of each variable on the outcome variable.
Result: A study showed that 47.7% [95%, CI: (42.6, 52.8)] of patients had good dietary pattern. Attained secondary school and above [AOR=2.2, 95% CI (1.3,3.5)], having family history of DM [AOR=2.0, 95%, CI (1.2, 3.2)], having family support [AOR=2.2, 95% CI (1.3, 3.7)], have fruit availability [AOR=2.4, 95%CI (1.1, 5.6)], being a member of diabetes mellitus association [AOR=1.8,95%CI(1.2, 2.9)], and having good diabetic knowledge about recommended diet[AOR=1.8,95%CI(1.1,2.8)] were independent predictors for good dietary pattern.
Conclusion and Recommendation: Majority of type 2 diabetic patients in Hospital had poor dietary pattern due to poor knowledge about recommended dietary pattern . Factors associated with dietary pattern of type 2 diabetes patients were attending secondary school and above, having comorbidity, being diabetes association member, the fruits being available, having family support and knowledgeable have positive association with good dietary pattern. Therefore, creation of awareness about recommended dietary pattern and diversification of feed types for the patients should be conducted that may help them to control their blood sugar level. Therefore, Concerned bodies better to develop health information dissemination programs and strategies that consider the importance of management of DM with diet, Family members should be informed about their important roles in encouraging patients to undergo DM management with diet.
Keywords: Dietary Pattern; Type 2 Diabetes Mellitus; Glycemic Control
Abbreviations: DM: Diabetes Mellitus; EFCT: Ethiopian Food Composition Table; FBG: Fasting Blood Glucose; FFQ : Food Frequency Questionnaire; FMoH: Federal Ministry of Health; IDF: International Diabetes Federation; RDA: Recommended Daily Allowance; T2DM: Type 2 Diabetes Mellitus; WHO: World Health Organization
The term diabetes mellitus defines a metabolic disorder of multiple etiology, which is characterized by chronic hyperglycemia with disorders of the carbohydrate, fat and protein metabolism due to defects in insulin secretion, insulin action or both [1,2]. Diabetes is a major health concern that has reached alarming levels: today, more than half a billion people are living with diabetes worldwide and this number is projected to increase by 46%, reaching 783.2 million by 2045 [2]. Type 2 diabetes (due to a progressive loss of sufficient B-cell insulin secretion, often against a background of insulin resistance) [3]. It is the most common type of diabetes characterized by disorder of insulin action and insulin secretion either of which may be the predominantly features [4]. There are several important risk factors that may lead to type 2 DM. These includes increasing urbanization, dietary changes, reduced physical activity , obesity, increasing age, a family history of diabetes , ethnicity and change in lifestyle changes [5,6]. The treatment of diabetes should begin with non-pharmacological therapies such as lifestyle interventions. A healthy lifestyle with regular physical activity and a healthy diet are very important tools for achieving and maintaining adequate blood sugar control in patients with type 2 diabetes [7]. Dietary patterns represent the entirety of the foods and drinks that a person consumes over a certain period; therefore, they are considered to be the most realistic measure of food intake [8,9]. In recent years, they have proven useful in explaining the relationship between diet and chronic illness [10-12]. Nutritionists and Dieticians, as well as health professionals, need to be informed on the relationships between dietary patterns and associated factors among these patients. This will develop their ability to manage Type 2 diabetes conditions better.
Diabetes is a major cause of morbidity and mortality [13,14]. It is one of the biggest global public health problems. Globally, the prevalence of type 2 diabetes is high and increasing across all countries [14,15]. This increase is driven by population aging, economic development and increasing urbanization leading to more sedentary lifestyles and greater consumption of unhealthy foods linked with obesity [14]. The prevalence is estimated to increase from 425 million people in 2017 to 783.2 million by 2045, more than 34 million in Africa, in Ethiopian 1.733 million people have diabetes with linked health, social, and economic costs [16-18]. According to International Diabetic Federation (IDF) 2015 the prevalence of diabetes mellitus in Ethiopia is 3.2% and there are 23,145 diabetes related deaths every year [14]. Ethiopia has shown limited progress towards achieving the diet-related non-communicable disease (NCD) targets [19]. Diabetes is estimated to affect 5.0% of adult women and 5.8% of adult men [20]. Since Diabetes is becoming a serious public health problem it requires continuous medical care, patients’ selfmanagement, education, and adherence to prescribed medication to reduce the risk of long-term complications [7].
In developing countries like Ethiopia when lifestyles are changing urbanization is expanding, literacy rate is low, and people still exist in poverty, DM and its impact on development and health is particularly critical. In Ethiopia inadequate routine health information and shortage of data on the proper dietary pattern of diabetic patients affect the long term management of diabetes [7,21,22]. Different studies conducted in Ethiopia showed poor self-care practice which in turn indicates poor dietary management [23-26]. Diabetic patients should maintain a diversified dietary pattern and regular eating habit for good glycemic control, prevention of complications and a good quality of life. The recommended dietary pattern for T2DM patients is almost similar to the general population achieving the minimum dietary diversity score of five (5) food groups from ten (10) food groups in a day [27]. The study gives first line information about actual dietary pattern and associated factors of type 2 diabetic patients in the study area. Intern: this should enable relevant health administrators to develop comprehensive and appropriate community-based health promotion strategies to encourage healthy lifestyles and appropriate dietary pattern for prevention and control of type 2 diabetes among its population. This document will also serve as a comprehensive evaluation for the nature of dietary pattern of type 2 diabetic patients. Above all, since there is no recent research conducted in similar area of the interest in the study area, the finding of this study could be used as a reference line data for those who are interested in carrying out further research.
Study Design and Period
An institutional based cross sectional study design was conducted at Felege Hiwot Comprehensive Specialized Hospital (FHCSH) Bahir Dar city from March 30 up to May 1, 2021.
Study Setting
Bahir Dar is found 565 kilometers away from Addis Ababa and located on the Southern shore of Lake Tana, the source of the Blue Nile. The total population size is 218,513 and ranks 7 in terms of population in Ethiopia from 40 cities. In Bahir Dar city administrative, a total of 156 health institutions are found, 3 hospitals,10 health centers,10 health posts and 134 private(primary, medium, specialty clinics and pharmacies) health institutions.
This study was conducted at FHCSH, which is the Comprehensive Specialized Hospital for Amhara Regional State, located in the central of the region Bahir Dar. The Specialty Hospital was founded in 1962 and since that time it has served about 5 million people, being as the referral hospital for many decades. The DM patient’s department is among the five inpatient departments in FHCSH. There are 7110 type 2 DM patients who had follow-up in the hospital of DM ward logbook. Around 840 type 2 DM patients are accounted for per month Population.
Study Population
All those type 2 diabetic patients who were on treatment follow up at outpatient department during the study period were included in the study.
Study Unit
Type 2 diabetic patients (individual).
The Inclusion and Exclusion Criteria
The Inclusion Criteria: All type 2 diabetes patients that had at least one follow up prior to data collection time and who came during data collection period.
The Exclusion Criteria: Patients who have hearing abnormalities and talking problems.
A patient who was critically ill and needed immediate treatment.
Patients who came for follow up for the first time were being excluded.
Sample Size and Sampling Procedure
Sample Size Determination: Sample sizes were calculated for the first and second objectives, and the largest sample size was obtained using the first objective, which was 390.
Sampling Procedure: Systematic sampling technique was used to select the study participant among type 2 diabetic patients, based on the flow rate that come for follow up during a month preceding the data collection. The list of patients (sampling frame) was obtained from the DM ward registration book of the patients registered for follow up in the hospital. Then the data collection was done using every Kth and selected cases were parts of sampling unit. The sampling interval ‘k’ was obtained by dividing the sampling proportion in one month’s(N) to the number of sample(n) at data collection site (n’) i.e. k = N’ /n’. Type 2 DM case flow in preceding month was 840 cases, sampling interval ‘k” =840/369 ~ 2.
Study Variables
Dependent variable.
Dietary Pattern (Good/Poor)
Independent variables
• Socio-Demographics: Age, sex, religion, income, and educational status
• Knowledge Related Factors: Nutritional knowledge, diabetic knowledge
• Health and Health Related Factors: Duration of illness, way of treatment, member of association, comorbidity and FBS.
• Lifestyle Factors: Regular physical activity, dietary changes
• Other Factors: Family support, family history of DM, cost of healthy foods, source of information, and availability of fruits and vegetables.
• Operational and Standard definitions
• Dietary Pattern: Quantities, proportions, variety or combination of different foods and beverages in diets and the frequency with which they are habitually consumed.
• Good Dietary Pattern: Study participants who consumed 5 and above food groups from 10 food groups(27).
• Poor Dietary Pattern: Study participants who consumed below 5 food groups from 10 food groups(27).
• Fasting Test Results: The result of fasting test with respect to glucose level in the body in which the result is normal if it is between 3.9 to 5.5mmol/l (70 to 100mg/dL) and more than 7.0mol/l (126mg/dl) will be poor. It has been rated high, optimal, and low according to the range provided by the International Diabetes Federation(14).
• Physical Activity: Physical activity was assessed using two items. In the last 7 days, how many total have you been physically active for at least 30 minutes? And what do you do in the house or as part of your work? Answers have been summarized (Range 0–22) patients who scored12 and above were coded as having a good physical activity practice (physically active). All others coded as poor physical activity [28].
• Comorbidities: The presence of one or more additional disease occurring with primary disease”.
• Good knowledge: When patients respond the mean or above the mean score on knowledge
• questions.
• Poor Knowledge: When patients respond below the mean score on knowledge questions.
• Doctor’s Advice: Emphasizes the intake of less fat, more fiber, less sodium and more foods that have health-promoting properties such as fish, soy products, fruits and vegetables, and doing physical activity [29].
Data Collection Tools and Procedure
Data Collection Tools: Data were collected using structured questionnaire which was developed and contextualized from different literatures and guidelines. The questionnaires included questions covering diabetic risk factors, demographics, monthly income, duration of diabetes, lifestyle, health profiles of the participants, barriers to adherence to good dietary patterns, diabetic knowledge and sources of information from the study participants using an interview-based structured questionnaire adapted from the WHO manual and reviewing different literature [24-26]. Dietary knowledge of the patient was adapted from a development of a general nutrition knowledge questionnaire for adults [30].
Dietary Data: The questionnaire also included a non-quantitative FFQ. The list of food items in the FFQ is created from locally consumed foods. For obtaining the dietary pattern, a value of one was given if participants have consumed from the food group and a value of zero was given if not consumed from the food group, with a maximum value of 10 if consumed from all 10 food groups. Dietary pattern was termed as low if the minimum DDS is below five and high if it is five and above. The standard questions were adopted from guidelines for measuring individual dietary diversity from FAO 2016 guidelines [27].
Fasting Test Results: the result of fasting test with respect to glucose level in the body in which the result is normal if it is between 3.9 to 5.5mmol/l (70 to 100mg/dL) and more than 7.0mol/l(126mg/ dl) will be poor. FBS data was taken from the patient’s file. The last FBS value was recorded for analysis. It was rated poorly controlled or good controlled according to the range provided by International Diabetes Federation [14].
Data collection procedure. Structured questionnaires were filled up via face-to-face interview by trained data collectors after the questionnaire pretested and relevant modifications were made before the start of the actual data collection. The study participants were invited to participate voluntarily by explaining the rationale of the study at the time of data collection. Two clinical nurses (degree) holder were recruited as data collectors and one public health officer and principal investigator were worked as supervisors. Data collectors and supervisors were trained for two days before and after pretest by the principal investigator on the questionnaire to be familiar with data collection tool. Editing and sorting of the questionnaires were done to determine the completeness and consistency of data every day during the data collection. The completed questionnaires were cross checked and made correction on a daily basis.
Data Quality Management: The quality of the data was assured by proper designing and pretesting of the questionnaire in other hospitals with similar socio-demographic characteristics to ensure its reliability. The questionnaire was prepared in English then translates to local language Amharic and back translated to English to check for its consistency. Pre-testing of the assessment tool was done on 39 type 2 DM patients at Tibebe Ghion Specialized Hospital. Modifications were made to the questionnaire based on the feedback found from the pre-test. The completeness of the data would be checked every day by supervisor and principal investigator, and the data collectors were asked to refill the data if incomplete data are found.
Data Management and Analysis: Data were checked for fulfillment and clean physically. Incomplete and inconsistent data were excluded from the analysis. The collected data is enter to EPI Data version 3.1 and then exported to SPSS version 23 for further analysis. Descriptive statistics were used to describe the sample. The results of the descriptive statistics were expressed as percentages and frequencies. Associations between independent and dependent variables were first analyzed using bivariable analysis to identify factors associated with the outcome variable. Those variables which were found to have an association with the outcome variable at P<0.25 were used in multivariable logistic regression to test for independent association. The magnitude of the association between different independent variables in relation to the dependent was measured using odds ratios, 95% confidence interval (CI) and P-values <0.05 were considered to be statistically significant.
Ethical Consideration: Ethical clearance is obtained from institutional board of Bahir Dar University School of public health research ethical committee. The permission letter was obtained from Amhara Public Health Institute (APHI) and Felege Hiwot Comprehensive Specialized Hospital medical director office. The nature of the study was fully explained to the type 2 DM patients to obtain their oral consent. The participants had also the right to refuse or terminate their participation at any point of time. The information provided by each respondent was kept confidential through anonymous recording and coding of questionnaire.
Socio Demographic Characteristics
A total of 369 diabetic patients were participated in this study, yielding a response rate of 94.6%. Among them, 220 (59.6 %) patients were males. The age of the study subjects was 20 to 83 years with mean (±SD) age of 55.5(±12.4) years. Three hundred fifty one (95.1%) of the study participants were Amhara in Ethnicity and Orthodox Christians followers were 279(75.6%). Three hundred (81.3%) patients attended formal education. Regarding monthly income of the study participants, 95 (25.7%) of them had below 1,100 Ethiopian birr per month whereas 56(15.2%) of the respondents got more than 10,149 Ethiopian birr. One fourth of the respondents were housewives 94(25.5%) and retired 93(25.2%) (Table 1).
Table 1: Socio demographic characteristics of type 2 Diabetes patients who were on follow up at Felege Hiwot Comprehensive Specialized Hospital Bahir Dar, Ethiopia (n=369).
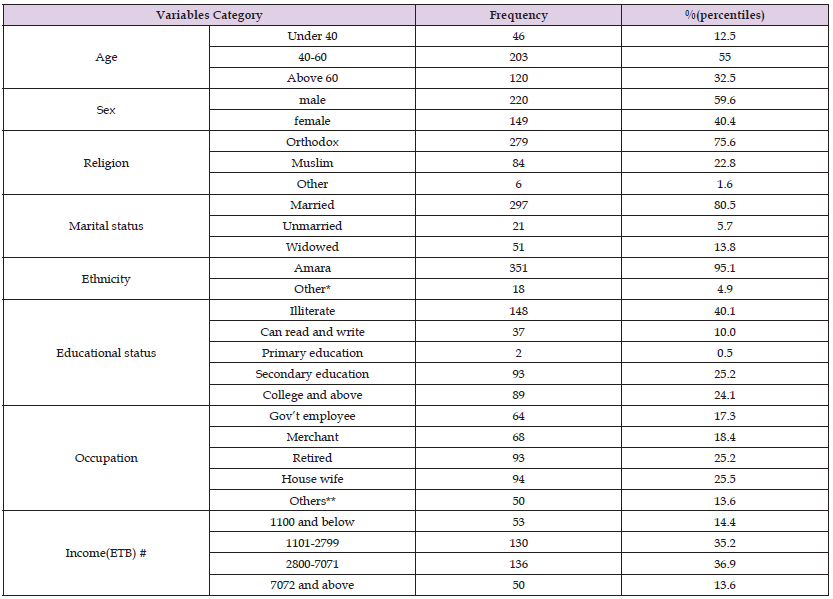
Note: *In Ethnicity Other includes Tigrie and Oromo.
**In occupational status “others” included Farmers, daily laborers, private organization employer and derivers.
#Income is categorized in quartile based on Ethiopian civil service salary scale of 2019/ 2011 E.C.
Health Profile of Type 2 DM Patients
Less than half, 160 (43.4%) patients were on follow up for less than 5 years while 34(9.2%) patients were on follow up for above 15 years. One hundred seventy-eight (48.2%) patients reported that they had family history of DM. Nearly two third, 237 (64.2%) patients had co- morbidity. The majority of the study subjects 347(94%) used oral hypoglycemic agents while 52 (14.1%) used insulin to control blood sugar level. Three fourths, 205 (55.6%) respondents said they had made a change of dietary habit when they knew they have diabetes (Table 2).
Table 2: Health profile of type 2 Diabetes patients who were on follow up at Felege Hiwot Comprehensive Specialized Hospital Bahir Dar, Ethiopia (n=369).
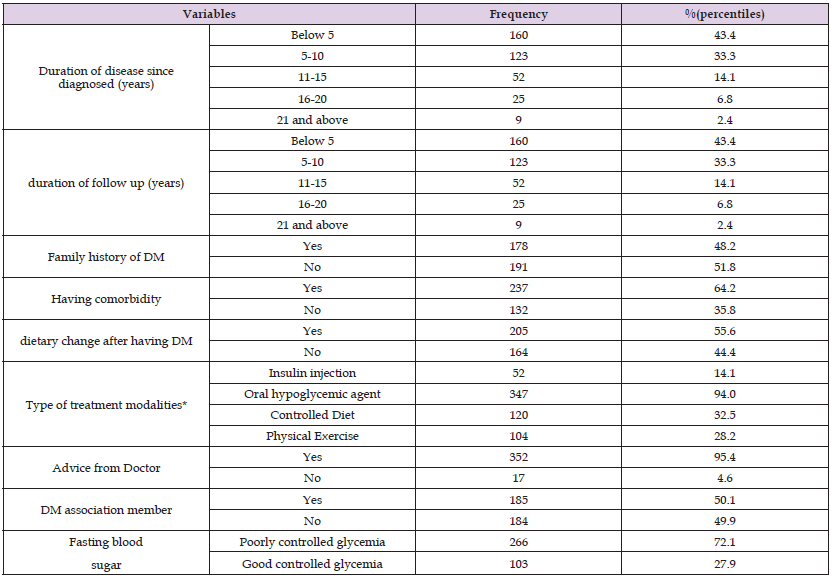
Note: *% more than 100 because some patients used more than one treatment options.
Dietary Knowledge of Type 2 DM Patients
With respect to knowledge about the recommended diet majority of the patient (53.7%) had poor dietary knowledge. The Mean ± SD knowledge score was 7.0 ± 1.65. The majority (81.3 %) of the respondents knew dietary modification as one of the ways to control blood glucose level. Only 45(12.2%) patients knew that consumption of refined grains have immediate effect on blood glucose level. Two hundred fifty-two (68.3%) of patients knew that consumption of vegetables used to achieve good glycemia. The majority of participants, 249(67.5%) of participants knew that skipping meal time couldn’t help to control blood sugar level (Table 3).
Table 3: Dietary knowledge of type 2 DM patients on follow up in Felege Hiwot comprehensive specialized Hospital, Ethiopia 2021 (n=369).
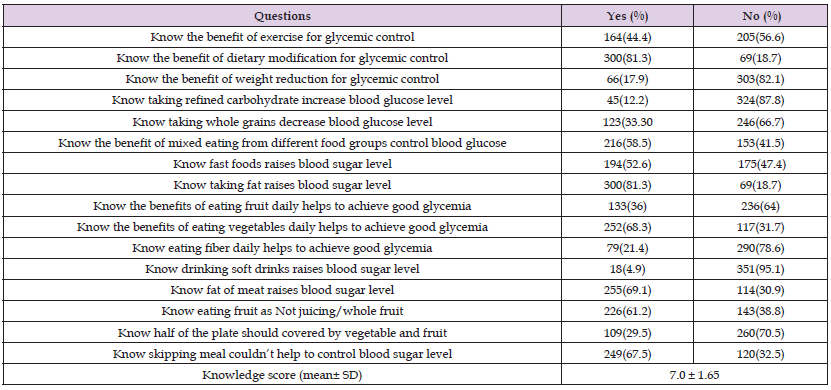
Figure 1 Dietary patterns of type 2 diabetic patients in percent at Felege Hiwot Comprehensive Specialized Hospital, Bahir Dar Ethiopia 2021 (n=369).
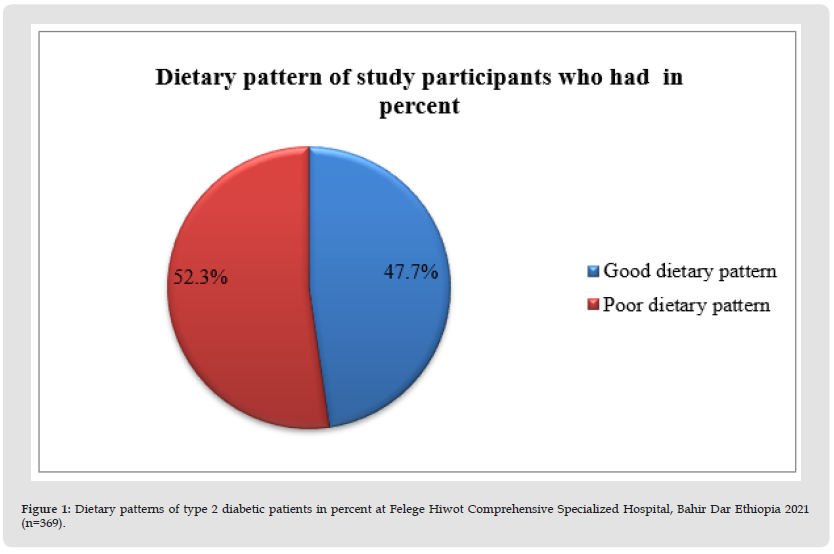
Dietary Pattern of Type 2 DM Patients
About 47.7%, (95% CI: 42.5-52.8) had had good dietary pattern. The most frequently consumed food groups were starchy staples (grains) (100%) and pulses (85.6%). The least consumed food groups were nuts and seeds (6.7%) and followed by diary product food groups (13%). Among 10 food groups’ grains and pulses are the major food groups that were consumed by the study participants daily. About one hundred thirty-eight (35.8%) and two hundred thirty-one (59.8%) of participants consumed fruits and vegetables respectively. Around half of the respondents did not consume any dark green leafy vegetables or any meals fortified with vitamin A substances and other fruits. Among those who consumed fruits 62 of them consumed once per day and the rest consumed twice per week. Among those who consumed vegetables, 80% consumed twice per week and 20% consumed once per day (Table 4).
Factors Affecting the Dietary Pattern of Type 2 Diabetic Patients
The bivariate logistic regression analysis showed that marital status, educational status, monthly income, comorbidity Figure 1, diabetic knowledge on recommended diet, family history of DM, regular physical activity, family support, cost of healthy foods, availability of fruits and vegetables and, dietary knowledge were statistically associated with dietary pattern of type 2 Diabetic mellitus patients. From the multivariable logistic regression analysis type 2 Diabetic patients who attended secondary education and above had 2.2 times higher odds of having better dietary pattern than those who attended less than secondary school[AOR=2.2, 95% CI (1.3,3.5)]. Patients who had family support were 2.2 times more likely to have better dietary pattern than patients who had no family support [AOR=2.2, 95% CI (1.3, 3.7)]. Likewise, patients who have fruit availability had 2.4 times higher odds of having better dietary pattern than their counterparts [AOR=2.4, 95%CI (1.1, 5.6)]. Patients who were a member of Diabetic Association were 1.8 times more likely to have better dietary pattern than those who were not a member[AOR=1.8,95%CI(1.2, 2.9)]. Diabetic patients who had good knowledge about recommended diet were 1.8 times more likely to have better dietary pattern than that of patients who have poor knowledge about recommended diet[AOR=1.8,95%CI(1.1,2.8)]. Similarly, patients who had comorbidity1.8 times more likely to have better dietary pattern than those who had not [AOR=1.8, 95% CI (1.1, 2.9]. (Table 5).
Table 5: Factors associated with dietary pattern of type 2 diabetic patients at Felege Hiwot Referral Hospital, Bahir Dar, Ethiopia, 2021(n=369).
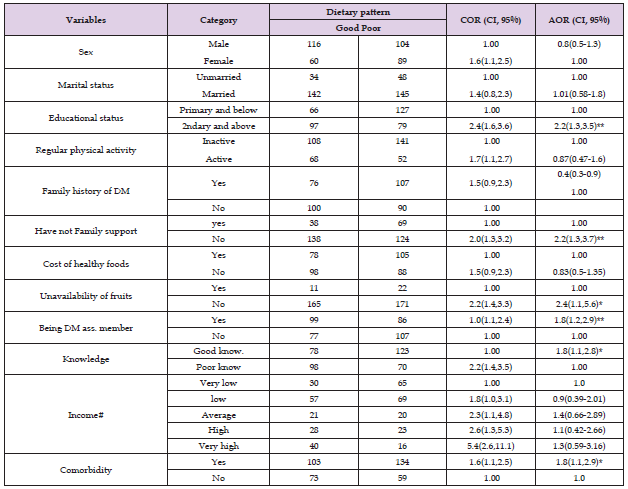
Note: *= Significant during multivariable analysis (p< 0.05), 1.0 =reference, Backward logistic regression was done. Hosmer and lemeshow goodness of fit of the model p-value=0.859.
Unmarried^ includes single, divorced and widowed. COR= crude odd ratio, AOR= adjusted odd ratio, and CI =confidence interval.
The study was conducted with the intention to assess dietary pattern and associated factors among type 2 diabetic patients. The study showed that more than half proportion of type 2 diabetic patients have poor dietary patterns. In this study 47.7% [95%, CI: (42.6, 52.8)] of the participants had good dietary pattern(≥ 5 food groups). The finding on good dietary pattern in this study is better than the study finding in Riyadh Saudi Arabia (41.7%) [31], United Arab Emirates (40%) [32], Tikur Anbessa Specialized Hospital Addis Ababa (22.2%) [23], Dilchora General Hospital Dire Dawa (37.5%) [25] and Felege Hiwot Hospital, Bahir Dar (35.9%) [24].
This difference might be because of the time gap between the studies conducted, socioeconomic status, and difference in diet habit of the patients. At this time the means of getting information about healthy dietary pattern and diabetes management mechanisms disseminated through different Media. Now there is also high internet coverage than before so they can get information easily and in understandable manner. Nutrition education is given through different media on diabetes patients diet than do earlier, so this plays a crucial role for improving knowledge on diabetes diet. But it is lower than studies done in Ahmadabad district of Gujarat state of India (73%) [18], in five health regions of Bahrain (89.5%) [33], and Adare General Hospital Hawassa, Ethiopia (55.2%) [7]. The difference might be due to differences in the study setting and population, data collection tools, socioeconomic status as well difference in diet habit of the patients. Additionally, the differences also might be due to having different information, education, and the availability of a healthy diet in the area and communication strategies in those countries. So, this implies the need for sustained effort to promote healthy dietary patterns for diabetes patients in this study area is crucial.
Another Study Also Done in Uganda on The Factors Affecting Adherence to Nutrition Therapy
Found that the practice of recommended nutrition therapy only 27.1% of the diabetic patients had good dietary pattern [34]. The difference could be explained by the time gap between study conducted, the variation in the settings of the study, difference in the socioeconomic and socio-demographic characteristics, number of study participants, study design used as well as difference in the types of foods available in the two regions. Educational status of respondents had an association with their dietary pattern. Study participants who attended secondary school and above had 2.2 times more likely to have good dietary pattern than counterparts. This is in line with two study findings in Iran [35,36], Bahrain [33], Tikur Anbesa Specialized Hospital, Addis Ababa, Ethiopia [37], Dilchora general Hospital, Dire Dawa, Ethiopia [25] and FHCSH [24]. The association between higher educational attainment of respondents and fitting dietary pattern might be described by the fact that patients with better education have better access to information from books, leaflets, newspaper and social media than uneducated patients. In addition, educated participants were better able to understand nutrition education provided by professionals or through the mass media than uneducated people.
Being an association member of Diabetes Mellitus was also another factor that had positive association with good dietary pattern which had 1.8 times more likely to have good dietary patter than who were not a member. This is due to patients who become an association member they have received diabetes education are more likely to use primary care and preventive services, take medications as prescribed, control their blood glucose level and have lower health costs.
In this Study, Patients Who Had Family Support Were 2.2 Times More Likely to Had Good Dietary
pattern as compared with patients who had not family support. Having family support is a crucial to promoting good dietary pattern. This study is supported by the study done in Bahrain [33],Systematic review on Thailand [38], Nepal [39], Jimma medical center, south west Ethiopia [40], Adare Hospital, Hawassa South Ethiopia [7], Felege Hiowt Comprehensive Specialized Hospital [24] ,and Debretabor General Hospital, North west, Ethiopia [41]. This might be due to being busy and did not understanding what to do, may be due to lack of awareness and insufficient knowledge about dietary regimen of diabetes among families and friends. Family support has a major impact on the patient’s ability to manage their chronic illness on their own. Friends and families can promote good health by influencing a person’s daily behavior, and the loss or reduction of that support can have negative health effects [42]. Family members are key foundations of both instrumental and emotional support. Instrument support includes assisting patients’ complete specific responsibilities, such as making an appointment with health care providers or helping with insulin injections while, emotional support can include providing comfort and encouragement when patients face distress or frustration over the long course of their diabetes care [38].
On the other hand, the findings from this study contradict the study conducted in Yekatit 12 Medical College Hospital, Addis Ababa [37]. These researchers, who examined nutritional practices and related factors in type 2 diabetes, found that social support was not linked to poor nutritional practices in diabetic patients. The differences in results between this study and the present study could be due to variation in the settings of the study and difference in sociodemographic characteristics. Patients who got nutritional education from doctors on diabetes diet were more likely to have good dietary pattern than those who didn’t get. This result is similar to the study result in Dilla University referral hospital, Southern Ethiopia [43], Felege Hiwot Comprehensive specialized Hospital Bahir Dar Ethiopia [24], Iran[35], Dilchora Hospital Dire Dawa, Eastern Ethiopia [25] and Nepal [39]. This is because nutrition education can change eating habits of patients. Frequent education about diabetes at hospitals and frequent DM education per year were associated with the good dietary pattern of the patients. This is in line with a study evaluating nutritional practices among diabetics at Yekatit 12 Medical College Hospital, Addis Ababa [37] and study done in South Africa which has identified the need for nutrition education related to diabetes care for optimal diabetes management [44].
Those who get nutrition education and who get more frequent nutrition education follow the advice from clinicians and have better knowledge and understanding about the foods suitable for condition of their disease, food guides and prescriptions than those who don’t get nutrition education. Availability of fruits and vegetables was another factor significantly associated with good dietary pattern. Participants who have no fruit and vegetables availability problem were 2.4 times more likely to had good dietary pattern than those who did. This result is in line with studies done a report on creating healthy food and eating environments in the United States of America [45] and study done in Adare Hospital Hawassa [7]. This may be due to the seasonality of fruits and vegetables which make the patients suffer from difficulty to take the recommended type and amount of fruits and vegetables, leading to poor dietary pattern. Comorbidity was also another factor affecting the dietary patterns of diabetic patients. Diabetic patients who have comorbidity are 1.8 times more likely to had better dietary pattern than those who had not comorbidity counterparts. This may be due to fear that if they have comorbidity, they will strictly follow good dietary pattern.
Strength and Limitation of the Study
The data was collected by the department staff members, so it gives an advantage to keep the quality of data.
This study has its own limitation; first the assessment of dietary pattern was based on self-reported dietary habits rather than direct observation. This may led to underreporting of socially undesirable responses and recall bias. Using self-reported dietary pattern as a measure of the level of practice may introduce social desirability bias. Since this study used non quantitative FFQ, there may be measurement errors such as over-reporting or underreporting of food consumption in general or of specific foods. Seasonal variation was also not covered and is the other limitation of the study.
The study found that 47.7% [95%, CI (42.5, 52.9)] of respondents had good dietary pattern indicated that majority of respondents had high prevalence of unhealthy dietary pattern and led relatively inactive or sedentary lifestyle. The factors improving the outcome variables were thoroughly analyzed. Attending Secondary school and above, having family history of DM, Bing DM association member, having comorbidity, the price of the food not to be costly, having family support, having good knowledge on recommended diet and availability of fruits and vegetables have positive association with good dietary pattern.
To the Hospital Administrative Bodies
It is better to have a routine nutrition education program and standardize this nutrition education that is given to type 2 patients and help to foster good eating habits among type 2 diabetic patients.
To Ministry of Agriculture
The Agricultural sector is better at designing effective and efficient mechanisms of fruit and vegetables production throughout the year rather than season based.
To family Members and Patients
Family members should be informed about their important roles in encouraging patients to undergo DM management with diet.
Patients are better off becoming an association member because they will receive diabetes education and are more likely to use primary care and preventive services, take medications as prescribed, control their blood glucose level and have lower health costs.
To Researchers
Further study which could see the association longitudinally is also recommended to address seasonal variability.
SAK developed the study proposal, served as the primary lead for study implementation and data analysis, and was a major contributor to writing and revising all drafts of the paper. OS, YM & NDG supported study implementation and data analysis, and contributed to writing the initial draft of the paper. AO, SMS and BA supported study recruitment and contributed to writing the final draft of the paper. TMS & YGM conceptualize and led protocol development for the study, a co-led study. implementation and data analysis and interpretation and was a major contributor to writing and revising all drafts of the paper. All authors contributed to its content. All authors read and approved the final manuscript.


