Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Giuliana Fulco Gonçalves1, Maria Helena Wanderley Costa Dantas1, Amália Cinthia Meneses Do Rêgo2 and Irami Araújo-Filho3*
Received: March 06, 2023; Published: March 13, 2023
*Corresponding author: Irami Araújo-Filho, Postgraduate Program in Biotechnology at Potiguar University/ UnP. Full Professor Department of Surgery, Federal University of Rio Grande do Norte. Full Professor, Department of Surgery, Potiguar University. Ph.D in Health Science/ Natal-RN, Av. Hermes da Fonseca, 1444 - Apto. 1302 - Tirol - Natal - State of Rio Grande do Norte, Zip code: 59020-650, Brazil
DOI: 10.26717/BJSTR.2023.49.007770
Gallstone disease and complications from gallstones are common clinical problems. The clinical presentation is from asymptomatic attacks of biliary pain requiring elective or emergency surgery. Bile duct stones can also associate with cholelithiasis, usually treated with cholecystectomies; about 10% of gallstones will develop gallstones, but only a smaller percentage in the bile duct. To avoid complications of choledocholithiasis, these stones should be removed. The direct open surgical approach to the bile duct can be made, but with the advance of techniques, endoscopic, radiologic, and laparoscopic surgical procedures have increased in number. In the era of laparoscopy and miniinvasiveness, therapeutic approaches can be performed in two sessions or one session. Comparison of these two approaches showed equivalent success rates, but the one-session treatment is characterized by a shorter hospital stay, and more cost benefits. This review article aims to provide medical student’s readers with a general summary of gallbladder stone disease in association with the presence of common bile duct stones by discussing surgical anatomy, clinical and diagnostic aspects, and possible treatments. A shorter hospital stays, and more cost benefits characterize the one-session treatment.
Keywords: Choledocholithiasis; Endoscopic Retrograde Cholangiopancreatography; Cholelithiasis; Laparoscopic Cholecystectomy; Biliary Tract Diseases
Bile is a liver-harvested liquid compound that plays a role in digestion. It travels through a system of branching bile ducts known as the biliary tree. The hepatocytes generate the bile at the cellular level, and canaliculi, which are thin tubular channels, collect it [1,2]. These canaliculi then direct the bile to an intralobular bile duct that contains all the bile from each lobule, which is the functional component of the liver. The intralobular ducts subsequently drain into interlobular ducts that exist between the lobules [3]. These interlobular ducts converge to create the two main bile ducts of the liver: the right hepatic duct (DHD) and the left hepatic duct (DHE). These ducts converge outside the liver to become the common hepatic duct, which goes through the hepatoduodenal ligament to the gallbladder [4]. The common bile duct (CBD) is formed by the combination of the DHC and the cystic duct. The point where bile enters the second part of the duodenum is marked by the hepatopancreatic ampulla, also called the ampulla of Vater, which is situated at the junction of the common bile duct and the pancreatic duct. The sphincter of Oddi’s smooth muscle fibers regulate the flow of bile into the duodenum and large intestine by opening into the duodenal papilla [3-5] When the sphincter of Oddi is closed, bile can also flow into the gallbladder for storage via the cystic duct [1-3].
The canaliculi of bile contain microvilli, which increase their surface area. The intralobular ducts can be found alongside the hepatic artery and portal vein. The portal triads, which are composed of these three structures, are surrounded by a layer of connective tissue referred to as Glisson’s capsule. The interlobular ducts are also part of this structure [6,7]. The right hepatic duct drains segments V, VI, VII, and VIII, which make up the right lobe of the liver, while the left hepatic duct drains segments II, III, and IV, which constitute the left lobe of the liver. The caudate lobe of the liver (segment I) is drained by small ducts from both the right and left lobes [8].
Extrahepatic segments of the right and left hepatic ducts. Common hepatic duct. Approximately 4cm long. Cystic duct: Outflow tract of the gallbladder. Approximately 7mm in diameter. Contains the cystic duct valves (or Spiral Valves of Heister). Common bile duct: contains 4 parts: supraduodenal, retroduodenal, intrapancreatic and intramural. The average diameter should be less than 6 mm. Ranging from 6.0 cm to 8.0 cm in length (Figure 1) [3-5].
Figure 1 Anatomy of the bile ducts and the arterial supply of the gallbladder. The four portions of the common bile duct are observed: supraduodenal, retroduodenal, intrapancreatic, and intramural.
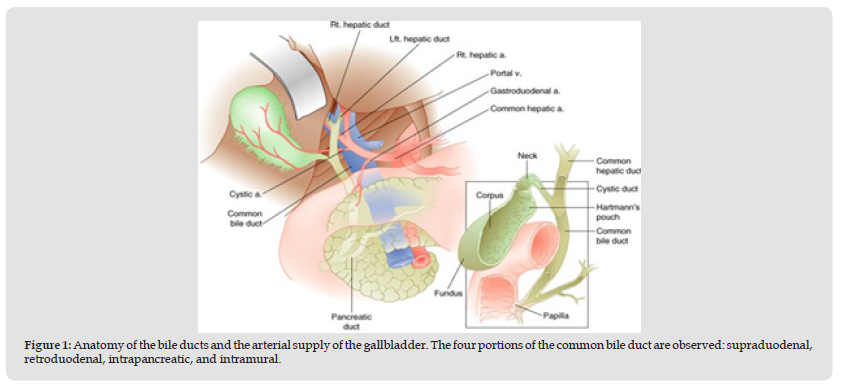
Note: Cameron J.
In terms of structure and purpose, the biliary tract primarily functions to transport and discharge bile. Bile is responsible for aiding in the digestion and absorption of fats and fat-soluble vitamins, as well as the elimination of fat-soluble waste materials [6]. The gallbladder plays a role in the storage and concentration of bile. The major constituents of bile consist of cholesterol, bile salts, and bilirubin, with bilirubin providing the distinct yellow-green hue of bile and also being excreted in the bile, which is responsible for the coloration of stool [2].
Arterial
The biliary system is supplied with blood from the celiac trunk, which branches off the abdominal aorta and gives rise to the common hepatic artery, splenic artery, and left gastric artery. The arterial supply to the bile ducts is of clinical significance in liver transplantation and biliary tract surgery [7,8]. The common hepatic artery is mainly responsible for supplying oxygenated blood to the liver. The blood supply to the biliary tree depends on a complex network of plexuses from subsidiary branches of major vessels, including the cystic, hepatic proper, gastroduodenal, and posterior superior pancreaticoduodenal arteries [3,4]. The paracholedochal net supplies the medial side and lateral to the bile duct, while the choledochal plexus runs at the top of the duct. However, different parts of the biliary tree receive varying amounts of blood supply from nearby arteries [9]. For instance, the supraduodenal choledochus, which is located just below the junction of the cystic duct and hepatic duct, receives the least blood supply, making it prone to ischemic attacks. This has significant implications in liver transplantation, where the arterial supply is often interrupted [3].
Vein Drainage
The vein network the biliary tree drains to is parallel to its arterial counterpart. For the most part, the drainage consists of venules connected directly to the hepatic vessels without differentiation into a cystic vein. The main difference is that the epi-choledochal venous plexus drains into the epi-choledochal network [2]. The epi choledochal plexus has an upper and lower outlet; the first joins the portal vein close to the hilar of the liver, while the second drains into the superior mesenteric vein before merging with the portal vein (Figure 2) [4].
Figure 2 Arterial and venous blood supply of the liver, gallbladder, pancreas, spleen, and the biliary ductal system.
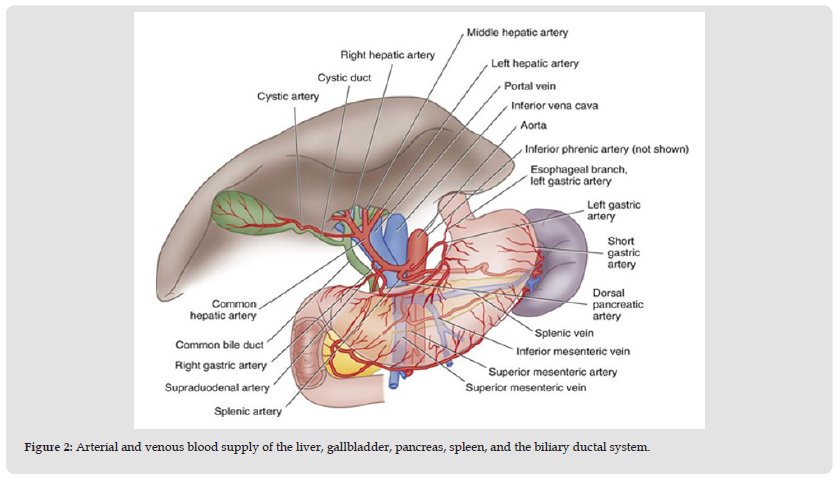
Note: https://basicmedicalkey.com/surgery-of-the-liver-biliary-tract-pancreas-and-spleen
Note: Netter F.
Lymphatic Drainage
Lymphatic drainage from the gallbladder is more commonly described than that from the bile ducts. From the gallbladder, lymph flows through the cystic lymph nodes, hepatic lymph nodes, and finally through the celiac chains (Figure 3) [5,6].
Innervation
The celiac plexus provides sympathetic and parasympathetic innervation to the biliary tree. Sympathetic fibers are carried by splanchnic nerves, while parasympathetic fibers are carried by the vagus nerve [10].
When stimulated, the visceral efferent fibers of the splanchnic nerve cause the gallbladder to relax, which allows bile to flow into the gallbladder through the cystic duct for storage [9-11]. In contrast, the hormone cholecystokinin, which the duodenum secretes when food enters the small intestine, primarily mediates gallbladder contraction and bile secretion. Parasympathetic fibers from the vagus nerve aid in this process [4-6].
Note: Netter F.
Anatomical Variation
Various configurations of bile ducts have been discovered through cadaveric and intraoperative cholangiography studies. Figure 4 displays a number of anatomical variations of bile ducts, some of which are more common than others [5]. Surgeons rarely encounter the presence of an accessory duct (Duct of Luschka) that runs from the liver and enters the gallbladder. The cystic duct typically arises from the gallbladder and merges with the common hepatic duct to form the common bile duct, with the confluence commonly found in the middle third of the right hepatic duct [12]. However, some individuals exhibit anatomical variations, such as a low fusion of a long cystic duct and the common hepatic duct, which is present in roughly 8.6% of the population. Other variations, such as the absence of a cystic duct or duplicated ducts, have been reported previously [6].
Cholelithiasis
The diagnosis of cholelithiasis can be made by the clinical picture, which is very characteristic and confirmed by ultrasonography (Figure 4). If ultrasound findings are unclear or complications are suspected, computed tomography and magnetic resonance imaging can provide helpful information [7]. There is no consensus on the most appropriate conduct in asymptomatic gallstones, but most clinicians and surgeons prefer not to operate on patients without specific symptoms preemptively. Some argue that prophylactic surgery has no concrete benefit in asymptomatic gallstones (Figure 5) [11-13]. Exceptions refer to particular situations:
• Patients residing in remote locations, which would make care difficult in case of complications.
• Immunosuppressed patients or using chemotherapy such as cyclosporine A and tacrolimus, considered pro-lithogenic.
• Insulin-dependent diabetics, more susceptible to infections.
• Patients with a “porcelain” gallbladder due to the risk of developing cancer.
Surgery is the treatment of choice in symptomatic gallstones and can be performed by laparoscopy or conventional surgery.
Figure 5 Cholelithiasis diagnosed by ultrasound. Typical image is observed of small intravesicular stones with posterior acoustic shadowing.
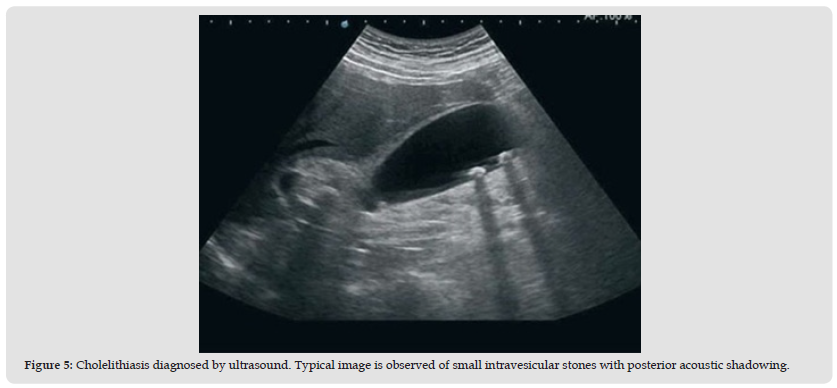
Note: https://basicmedicalkey.com/surgery-of-the-liver-biliary-tract-pancreas-and-spleen/
Acute Cholecystitis
In the past, there was controversy as to whether the best treatment for acute cholecystitis would be urgent cholecystectomy or treatment with antibiotics to control inflammation and elective surgery within three months, when theoretically, there would be better clinical and technical conditions [14]. Prospective studies comparing patients randomly selected for one or another procedure demonstrated that postponing the operation was not always possible, either due to the worsening of the acute condition or due to recurrence or complications such as choledocholithiasis or pancreatitis during the waiting time, leading to emergency operations in worse clinical conditions in 14-30% of cases, increasing mortality to up to 28% and also causing worsening of local conditions with fibrosis and adhesions that increase the risk of injury to biliary structures [8,15]. The recommended conduct became cholecystectomy in the acute phase as soon as possible. Immediate laparoscopic cholecystectomy or within 24h of admission is the ideal treatment, as it has a meager conversion rate due to technical difficulties, which is not different from the findings in elective surgery [16].
When there are more severe cases with systemic alterations and organic insufficiencies, it is necessary to consider them. Treatment (with volume replacement, antibiotics, etc.) may improve an individual with a new focus of infection that may progress to gangrene. The presence of necrosis worsens the prognosis9.
In cases of prohibitive surgical risk due to severe organic failure or technical conditions, such as portal hypertension, cholecystostomy by a transparent-hepatic puncture can offer satisfactory results. In the absence of this resource, it is possible to perform a surgical cholecystectomy, even with a minimal incision and local anesthesia, if prior demarcation of the gallbladder is completed with the help of ultrasound [1-3,17]. This procedure allows the postponement of the laparoscopic cholecystectomy after the patient’s clinical improvement, which generally occurs between 24-48h. Other case series and retrospective studies suggest that cholecystectomy in elderly and high-risk patients is more effective and has lower mortality than percutaneous cholecystostomy [10-12]. Antibiotics with a Gramnegative spectrum should be started during the preparation for the operation and, depending on the surgical findings and intercurrences, may be suspended after the operation, or maintained and adequate for cultures of the gallbladder content or its wall [18].
Posoperative Complications
Morbidity and mortality from surgical treatment of acute cholecystitis are very low. They are mainly related to the severity of the critical condition and the presence of portal hypertension and systemic complications of advanced age [17-19]. Other complications associated with the disease’s severity, such as peritoneal infection, pancreatitis, and organ failure, are uncommon in both procedures. Iatrogenic bile duct injuries in acute cholecystitis occur in approximately 0.1% of cases operated by laparotomy [13,20]. The incidence of injury with the laparoscopic procedure is similar; on the other hand, the recommendation is not to hesitate to convert the system if there is difficulty in identifying structures [7,21]. Postoperative mortality in the treatment of acute cholecystitis is an infrequent event. Therefore, success in treating acute cholecystitis depends on rapid indication, preoperative care, and early surgery [11].
Choledocholithiasis
The existence of a calculus in the common bile duct defines Choledocholithiasis. Its incidence in the Brazilian population is approximately 1.5%; therefore, it is a subject of extreme importance in clinical practice [12]. The disease is classified into two main types, depending on the origin of the calculi in the common bile duct: primary or secondary. Their differentiation is significant in defining the therapeutic approach (Figure 6) [8-10,22].
Note: https://medicalterminologyblog.com/gallstonescholelithiasis-choledocholithiasis/
Primary: Defined by the calculus formation within the common bile duct. It involves 5-10% of patients. They are usually brown calculi with composite components (calcium bilirubin + cholesterol) [23-25]. They are related to obstructive biliary processes (biliary stasis), factors that increase pressure within the common bile duct, and local infections. In addition, most patients who develop primary choledocholithiasis have previously undergone cholecystectomy due to yellow or black stones [2,14].
Secondary: Defined by calculi formation in the gallbladder or proximal biliary tract and subsequent migration of these calculi to the common bile duct. They involve 90-95% of patients [18,26]. Stones can be yellow (75%), rich in cholesterol, or black (25%), rich in bilirubin. The first is closely related to excess serum cholesterol, which evolves with high cholesterol in the gallbladder, precipitating calculi formation. The second is usually in small proportions (<1cm in diameter) and has an essential relationship with chronic hemolysis6, [13-15]. About 8-20% of patients with gallbladder stones evolve with the migration of these stones to the common bile duct. Thus, cholelithiasis is the main risk factor for the development of choledocholithiasis [14,27]. In this context, the risk factors for the development of cholelithiasis are female gender, age around 60 years, obesity/dyslipidemia, cirrhosis, and infections, among others, which are essential for the development of secondary choledocholithiasis [13,28]. As risk factors for choledocholithiasis of primary origin, there are mainly biliary stasis (caused by bile duct stenosis, secondary compression of the same) and biliary tract infections [29].
Clinical Condition
Half of the patients with choledocholithiasis may progress asymptomatically. In these patients, the calculus passes through the common bile duct and is expelled into the second portion of the duodenum without obstructing the biliary tract [24-26]. In symptomatic patients, the most characteristic symptom of the disease is fluctuating jaundice – the patient evolves with periods of jaundice interspersed with periods of remission of the icteric condition [17,24]. This is because the stone moves in the common bile duct, temporarily clearing the bile flow (with an improvement in jaundice) until it impacts a new, more distal location of the chimney [11,26]. In addition, the typical picture of these patients may include pain in the right hypochondrium of the abdomen (similar to the pain found in patients with acute cholecystitis, however, of a transient nature) and other signs of cholestasis, such as jaundice, choluria (urine stained dark) and acholia fecal (light stool) [26-28]. Once the diagnosis is made based on the clinical picture, laboratory tests detecting direct hyperbilirubinemia (conjugated bilirubin) in periods when there is obstruction of the biliary tract, in addition to an increase in alkaline phosphatase and gamma-GT (canalicular enzymes which, when increased, suggest obstruction of the biliary tract. Imaging tests will seal the diagnosis [13,23]. Ultrasound, cholangioresonance, endoscopic ultrasonography, and endoscopic retrograde cholangiopancreatography (ERCP), depending on the case, will confirm the diagnosis [29,30].
Treatment
All patients diagnosed with choledocholithiasis should be treated surgically due to the high risk of serious complications [14]. In case of urgency, the immediate conduct is the hemodynamic stabilization of the patient and the clearance of the obstruction as soon as possible. In cases that are not urgent, there is some time to investigate and schedule the unblocking procedure on an elective basis. The second step in defining the treatment is to discern the origin of the calculus impacted in the biliary tract [24-27]. The secondary origin choledocholithiasis must undergo cholecystectomy and treatment to clear the biliary tract. If the diagnosis of choledocholithiasis occurs before the cholecystectomy (ideal situation), the most indicated is to perform ERCP and clear the biliary tract even before the cholecystectomy [29-31]. From ERCP, endoscopically, it is possible to perform a papillotomy (opening of Vater’s papilla) and, therefore, remove the calculi that are impacted in the common bile duct (Figure 7) [15]. In patients diagnosed with choledocholithiasis during cholecystectomy, the ideal is to perform surgical exploration of the common bile duct at the same time, preventing the patient from undergoing a new invasive procedure after surgery [16]. However, elective endoscopic papillotomy in the postoperative period can be scheduled. Another option is in cases of intrahepatic calculi, stenosis of the sphincter of Oddi, and primary choledocholithiasis when conventional or laparoscopic surgical treatment can be considered, such as a Rouxen- Y choledochoduodenostomy or choledochojejunostomy [17].
Biliary Tract Injury
Bile duct injury is a potential complication of cholecystectomy. Incorrect identification of critical anatomical structures is a common cause, mainly due to anatomical variations of the cystic duct. The incidence is higher in a laparoscopic procedure than in an open procedure [18]. During the operation, it is essential to identify the bilocystic triangle (Calot’s triangle) - an anatomical space defined superiorly by the inferior border of the liver, medially by the common hepatic duct, and laterally by the cystic duct. Calot’s triangle contains structures such as the cystic artery and the cystic lymph node (Mascagni’s node) [30-32]. Rarely, an accessory hepatic duct or right hepatic artery can also be found traversing this space. To avoid unwanted arterial or biliary injury, surgeons must establish a «critical view of safety.» [24,25]. The critical safety view comprises three components: identifying the Triangle of Calot, exposing the gallbladder’s lower portion (infundibulum), and revealing only the cystic duct and cystic artery for ligation [19]. Cholecystectomy, the surgical removal of the gallbladder, is usually performed laparoscopically. Indications for cholecystectomy include symptomatic cholelithiasis, cholecystitis, porcelain gallbladder, and gallbladder polyps larger than 0.5cm. Cholecystectomy is recommended for patients with asymptomatic cholelithiasis if there is an increased risk of gallbladder carcinoma or other complications [20].
Clinical Evaluation
The biliary tract provides an outlet to transport bile to the gastrointestinal tract, which facilitates the absorption of fat-soluble nutrients. In general, acute obstruction of the biliary tract can lead to steatorrhea, while chronic obstruction can cause deficiency of fatsoluble vitamins (A, D, E, and K) [22,30]. Proximal to the obstruction site, it also harbors an opportunity for bacterial infection, as in the case of ascending cholangitis21. If left untreated, a chronic biliary obstruction can lead to portal hypertension and its associated complications [12]. Congenital anomalies associated with the biliary tract include biliary atresia, choledochal cysts, and congenital biliary ectasia. Biliary atresia is the most common cause of conjugated hyperbilirubinemia in young infants. The etiology of the disease is not well understood; however, genetic and environmental factors have been implicated [22]. Several mechanisms have been proposed, including failure to recanalize during bile duct formation and repeated structural insult leading to extensive luminal fibrosis. Patients usually have normal growth but gradually develop jaundice and cat stool within two months of birth [23,24].
Injury After Laparoscopic Cholecystectomy
Complications can arise from cholecystectomy, such as injury to the bile duct, which can occur due to incorrect identification of anatomical structures. This is more common in laparoscopic procedures than open procedures, and it is crucial to identify the bilocystic triangle (Calot’s triangle) during the operation. 18 Calot’s triangle is defined by the inferior border of the liver, the common hepatic duct, and the cystic duct and contains important structures such as the cystic artery and the cystic lymph node (Mascagni’s Node) [30-32]. Occasionally, an accessory hepatic duct or right hepatic artery may also be present in this area, which can increase the risk of injury. Surgeons must establish a «critical view of safety» to avoid injury to the artery or bile duct [ 24-25]. The critical safety view involves identifying the Triangle of Calot, exposing the gallbladder’s lower portion, and only revealing the cystic duct and cystic artery for ligation. Cholecystectomy, which is the surgical removal of the gallbladder, is commonly performed laparoscopically and is indicated for symptomatic cholelithiasis, cholecystitis, porcelain gallbladder, and gallbladder polyps larger than 0.5cm. In patients with asymptomatic cholelithiasis, cholecystectomy is recommended if there is an increased risk of gallbladder carcinoma or other complications [19-20].
Clinical Management
Clinical assessment involves examining the biliary tract, which serves as a pathway for bile transport to the gastrointestinal tract, aiding in the absorption of fat-soluble nutrients. Acute biliary obstruction can result in steatorrhea, while chronic obstruction can lead to a deficiency of fat-soluble vitamins (A, D, E, and K) [22,30]. Additionally, bacterial infection can occur proximal to the obstruction site, as seen in ascending cholangitis [21]. Chronic biliary obstruction, if left untreated, can lead to portal hypertension and its associated complications [12]. Congenital anomalies associated with the biliary tract include biliary atresia, choledochal cysts, and congenital biliary ectasia. Biliary atresia is the most frequent cause of conjugated hyperbilirubinemia in young infants. The etiology of the disease is not well understood, but genetic and environmental factors have been linked to its development [22]. Several mechanisms have been proposed, including failure to recanalize during bile duct formation and repeated structural damage resulting in extensive luminal fibrosis. Within two months of birth, affected infants usually develop jaundice and pale stool but have normal growth [23,24].
Laparoscopic Cholecystectomy / Complications
Bile duct injury is a potential complication of laparoscopic cholecystectomy and is considered the most significant one. Patients with such injuries are usually referred to tertiary referral centers immediately or after unsuccessful reoperation [25]. The rates of successful repair are higher in these centers, making it highly recommended for patients to be referred early to such centers. An interdisciplinary team, including surgeons, radiologists, endoscopists, and anesthesiologists, should also be consulted to manage the patient’s initial condition [26]. The optimal time for BTI repair is still controversial and depends on several factors, including the patient’s general condition, favorable local abdominal factors for a successful repair, and the surgeon’s experience. [27-32] Performing the definitive operation early (within the first 72 hours), in the period, or in the late period (after 1.5 months) of the injury significantly affects the morbidity of patients [27-30].
Biliary colic is characterized by intermittent, dull pain in the right upper quadrant due to transient blockage of bile flow, while cholelithiasis refers to gallstones present in the gallbladder. Choledocholithiasis indicates the presence of gallstones located in the common bile duct, while biliary pancreatitis is pancreatic inflammation due to blockage of the pancreatic duct by gallstones. Cholecystitis is gallbladder inflammation due to prolonged obstruction of the cystic duct, and cholecystectomy is the surgical removal of the gallbladder. Cholangitis, on the other hand, is an infection of the bile ducts, while cholangiocarcinoma is an aggressive cancer of the bile ducts.
None.
The authors thank the Federal University of Rio Grande do Norte, Potiguar University, and Liga Contra o Cancer for supporting this study.


