Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Salome T Frimpong1*, Uri S Markakpo2 and Adelaide M Ansah Ofei3
Received: February 14, 2023; Published: March 04, 2023
*Corresponding author: Salome T Frimpong, Ghana Health Service, Greater Accra Regional Hospital, P.O. Box 473, Accra, Ghana
DOI: 10.26717/BJSTR.2023.48.007726
Background: Care coordination practice among nurses although essential for good quality healthcare delivery has been challenging.
Objective: The study identified the factors that influence care coordination among nurses in the unit level of a regional hospital.
Methods: A cross-sectional approach was adopted, and 262 participants were selected from eight units in the hospital using a convenient sample technique. A structured questionnaire was used in collecting data.
Results: This study revealed that nurses with low qualifications lead to poor outcome of care coordination practice. Also, the lack or absence of all the predictive factors thus, external factors and patient characteristics, influence the outcome of care coordination practice among nurses.
Conclusion: External factors and patient characteristics influence the practice of care coordination in the 8 units. Providing adequate resources, addressing patients’ condition and adequately training personnel will foster care coordination practice which in turn maximises quality healthcare delivery.
Keywords: Healthcare; Influencing Factors; Nurses and Care Coordination
Hospitals are complex healthcare organizations in which different professionals work synergistically to deliver healthcare services [1]. This situation often leads to rivalry, confusion, errors and delay in healthcare delivery if good interpersonal relationships do not exist among the workforces. Poor interpersonal relationship hinders care coordination among healthcare providers affecting quality healthcare delivery. McDonald, et al. [2], defined care coordination as “the deliberate organization of patient care activities between two or more participants (including the patient) involved in a patient’s care to facilitate the appropriate delivery of health care services’’. This organization of care involves orderly arrangement of both healthcare personnel and other resources needed to carry out all required patient care activities, often managed through the exchange of information among individuals responsible for different aspects of care. Nursing staff forms the largest and costliest resource in the healthcare organization [3]. The role of Registered Nurses (RNs) among the health team is pivotal in ensuring effective delivery of quality healthcare services. However, care coordination among nurses, particularly, in regional hospital, has always been a challenge partly, as a result of inadequate staff, lack of resources, lack of motivation for staff, high turn-up of patients and fragmentation of services in the healthcare setting [4]. Although nursing practice demands coordination within and across units and departments, it is often not approached as formal practice due to afore mentioned factors as well as complexity of patients’ condition, task characteristics, structure and poor relationship, which in turn, may be due to lack of management prioritization of the practice of care coordination among the workforce [5].
Theoretical Framework
The Van Houdt, et al. [6], Theoretical Framework for care coordination was adopted for the study. This composite framework, which is a synthesis of different models, measures external factors, patient characteristics, organizational mechanisms, relational coordination, and the outcomes of care coordination. Even though this framework was considered the most suitable it also has a limitation of not making provision for measurement of nurses’ socio-demographic characteristics and only described the various constructs within it but did not test its applicability for the study of factors that influence care coordination among nurses, hence, was adopted with modification. It was this additional research gap identified that formed the basis for adapting this conceptual framework for the current study.
Care coordination by nurses towards patients depends on several factors which include external factors, patient characteristics and nurses’ socio-demographic characteristics. These factors have individual components which work in synergy to influence the outcome of care coordination. According to Van Houdt, et al. [6] external factors such as social security system, current legislation, existing resources, evidence and positive media coverage have significant influence on the organization of structures within the healthcare institution towards delivery of effective care for patients. Current legislation (National Health Insurance Scheme) in relation to health and allocation of resources to healthcare institutions affects the healthcare organization. Patient characteristics also significantly influence how nurses coordinate healthcare activities in the unit. In addition, patient characteristics determine the organizational mechanisms such as task characteristics, structure, knowledge and information technology, administrative processes, and cultural factors to consider before coordinating healthcare activities.
Study Design and Setting
A cross-sectional survey was used to identify factors that militate against care coordination among nurses in the unit. The approach is used to gather information about individuals at a single point in time and can be justified from a theoretical perspective, allowing inferences to be drawn about the relationships between independent and dependent variables. Finally, the Van Houdt, et al. [6], Theoretical Framework for care coordination (Figure 1) was considered for the study. The framework measured external factors, patient characteristics, organizational mechanisms, relational coordination and the outcomes of care coordination. Even though this framework was considered the most suitable it also has a limitation of not making provision for measurement of nurses’ socio-demographic characteristics, and therefore, was adopted with modification. Since this study was developed upon the theory of factors influencing nurses’ care coordination by Van Houdt, et al. [6], findings are sufficiently supported. Hence, the clear theoretical assumptions provided by the theory about the relationship between external factors, patient characteristics and the outcome of care coordination provided a good tool to test hypotheses. The study was conducted at GARH, which is the only referral secondary health institution in Accra, that provides specialized care and diagnostic investigations that are not available at the district level. The hospital was chosen as a result of it being a secondary facility with a variety of healthcare professionals meeting at the unit to render quality care to patients.
Sampling Technique
The target population were all nurses working in GARH. All permanent professional or auxiliary nurses who have worked in the unit for three months. The sample size was calculated using the population of nurses (both professionals and auxiliaries) working in the GARH. The auxiliaries were included in the study as they form a significant number of workforce (117) which augment the work of the professional nurses. Using Yamane [7] formula, the sample size was calculated to be 238 and adjusted by 10% to 262 for non -response. The convenience sampling technique was used to select 262 nurses from the units. The main reason for using this method was the availability of the respondents at the various units. A selfadministered questionnaire was given to the 262 eligible nurses. Participants were informed about the purpose, risk and the benefits of the study and were assured of anonymity and confidentiality. Questionnaires were administered individually to nurses in the unit and completed questionnaires were sealed in envelopes and kept by the nurse in charge of the unit. Questionnaires were either completed in the unit or taken home by participants. Completed questionnaires were later collected from the unit in charge by the first author. In all, 258 questionnaires were retrieved representing a response rate of 98.5%. Data were collected from February to April 2018 after obtaining institutional consent from hospital administrator.
The questionnaire was made up of both close and open- ended questions and divided into three sections: Section A explored the sociodemographic characteristics whereas the other sections determined external factors and of patient characteristics using a 5-points Likert scale. Face reliability was measured by pre-testing the questionnaire using 60 nurses from a Teaching hospital with similar characteristics as the study setting. Four questions were deleted and six were edited afterward. The Cronbach’s alpha for the different subsets of the questionnaire indicated good internal consistency: external factors (0.742) and patient characteristics (0.938). The scientific and ethics protocol of this study was approved by the Nugochi Memorial Institute for Medical Research Institutional Review Board (NMIMR-IRB) and the Ghana Health Service Ethical Review Committee (GHS-ERC).
Statistical Analysis
The Statistical Package for Social Sciences (SPSS) version 24 was used to perform descriptive, Pearson Correlation and multiple regression analyses. Participants’ socio-demographic characteristics were summarized and presented using frequencies and percentages. Likewise, external factors and patient characteristics were analyzed and presented using mean and standard deviations. The factors were measured individually using a 5-point Likert scale. A score of ≤ 2 indicated a low level, scores of 3 showed moderate level, and scores of ≥ 4 showed a high level. Pearson Correlation analysis was performed to identify the relationship between variables whereas, regression analysis was done to determine the extent to which the factors predict the outcome of care coordination.
Table 1. shows Socio-demographic characteristics of nurses (gender, basic qualification, rank, unit worked and unit workload). Out of 223 participants, 47.09% were between the ages of 26 - 30 years and most (39.30%) of the participants were staff nurses or midwives. The majority (53.54%) of the participants had diplomas whereas 21.68% of the participants had a first degree in nursing. Out of 229 participants, 23.14% worked in the theatre, and only 2.62% worked in the medical unit (Supplementary Table 1). The nurses had worked in their respective units for periods ranging between 3 months to 17 years. Table 2 shows the mean score for external factors as 3.70. The results also show that nurses strongly agree to the fact that the hospital caters for both NHIS subscribers and non-subscribers [mean ± standard deviation (SD): 4.3 ± 0.87]; Enrolment into the scheme gives patients access to certain services (mean ± SD: 4.4 ± 0.83); delay in payment of NHIS claims affect resources needed to provide care (mean ± SD: 4.3 ± 0.98); and all referred cases and self- referred seek healthcare services in the facility (mean ± SD: 5.0 ± 4.69). Table 3 describes the patient characteristics that militate against nurses’ care coordination in the units. The mean score for patient characteristics was 3.67. The results showed that to a very high extent, patients with multiple complex conditions require care coordination among nurses (mean ± SD: 3.94 ± 1.16); patients who seek early care aid in early detection, diagnosis and treatment (mean ± SD: 4.18 ± 1.13); patients’ who adhere to nurses’ regimen recover quickly from their conditions (mean ± SD: 3.96 ± 1.15) and patients’ whose views are respected have stress reduction (mean ± SD: 4.07 ± 1.05).
Table 2: Hierarchical Multiple Regression on the effect of Socio-Demographic Characteristics on Outcome of Care Coordination.
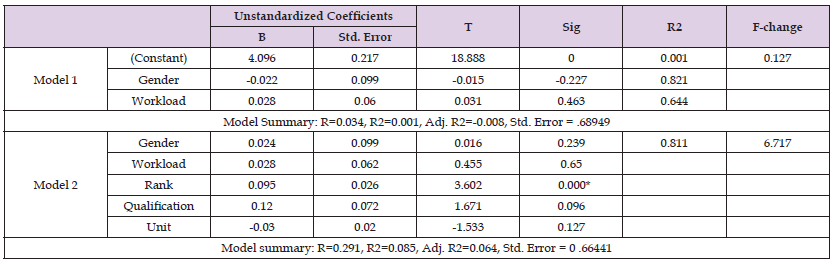
Note: Source: Field data 2018.
Note: Outcome of care coordination (Source: Field data, 2018).
Effect of External Factors on Outcome of Care Coordination
Hypothesis 2: External factors have significant effect on the outcome of care coordination practice among nurses in the unit. From Table 3, it is observed that the hypothesis is fully supported by the data since external factors have significant effect on the outcome of care coordination (β = 0.634, p = 0.000) (Table 4).
Note: Outcome of Care Coordination (Source: Field data, 2018).
Note: Source: Field Data, 2018.
Note : Source: Field Data, 2018.
Effect of Patient Characteristics on Outcome of Care Coordination
Hypothesis 3: Patient characteristics have a significant effect on the outcome of care coordination practice among nurses. Table 5 indicates that the hypothesis is fully supported by the data since patient characteristics have a significant effect on the outcome of care coordination practice in the unit (β = 0.406, p= 0.000) (Table 6).
The study revealed that the socio-demographic characteristics (gender, rank, basic qualification, unit and unit workload) of participants apart from rank, had no significant influence on the outcome of care coordination (β = 0.095, p < 0.001) suggesting that no matter the gender, qualification, unit or unit workload, care coordination can be practiced. According to Van Houdt, et al. [6], external factors such as social security system, current legislation, and existing resources are important issues that militate against care coordination which is necessary for good quality health care among health care professionals. Participants generally believe that external factors militate care coordination practice in the units. The mean score for those external factors were above average, indicating a significant influence on the outcome of care coordination in the unit. These findings corroborate the work of Mosadeghrad [8] who asserted that inadequate resources (materials) such as manometers, thermometers and Glucometers in the units affect the quality-of-care outcome.
The results also show that nurses strongly agree to the fact that the hospital caters for both NHIS subscribers and non-subscribers [mean ± standard deviation (SD): 4.3 ± 0.87]. However, the findings is contrary to the work of Aryeetey, et al. [9] which indicated that challenges such as high patients’ turn up, inadequate personnel and other resources facing health care facilities have not received corresponding attention which can also militate against care coordination practice among health personnel. Furthermore, the study showed that enrolment into the scheme gives patients access to certain services (mean ± SD: 4.4 ± 0.83); delay in payment of NHIS claims affect resources needed to provide care (mean ± SD: 4.3 ± 0.98); and all referred cases and self- referred seek healthcare services in the facility (mean ± SD: 5.0 ± 4.69). Table 3 describes the patient characteristics that militate against nurses’ care coordination in the units. The mean score for patient characteristics was 3.67. The results showed that to a very high extent, patients with multiple complex conditions require care coordination among nurses (mean ± SD: 3.94 ± 1.16); patients who seek early care aid in early detection, diagnosis and treatment (mean ± SD: 4.18 ± 1.13); patients’ who adhere to nurses’ regimen recover quickly from their conditions (mean ± SD: 3.96 ± 1.15) and patients’ whose views are respected have stress reduction (mean ± SD: 4.07 ± 1.05).Hence, provision of quality health care requires a multi-sectorial approach which should be led by the state.
The study indicated that the state is playing its role as health coordinator to improve services delivery (M= 3.5 and 1.28). The role of the state is to ensure that the ministry of health plan and develop policies such as NHIS and see to it that it is implemented by the GHS. There is therefore the need for government to allocate more resources into the health care sector to enable personnel deliver effective and efficient care to the citizenry. Finally, patients are key stakeholders of quality health care. Thus, health professionals’ interaction with patients is recommended to be patient-centered rather than professionally- directed. Patient characteristics such as coping strategy, social network, patient personality and expectations influence care coordination practice among health care professional especially, nurses. Van Den Oetelaar [10] in their study on “Balancing nurses’ workload in hospital wards” also reported that health care service delivery is partly dependent on human resource availability. In addition, a report by the Sudan Institute of Medicine (2010), highlighted the fact that economic resource is highly important in ensuring high level of good quality care among health care providers.
Furthermore, social security and legislation are external factors that are considered to be very important in coordination of health care activities for patients, because they minimize out of pocket spending, reduce the inequality in access of health care services and provide adequate capital for procurement of logistics necessary for effective healthcare delivery [9,11,12]. In recognition of this fact therefore, the National Health Insurance Law (NHIL) was enacted in Ghana in 2003. Following this, Ghana begun the implementation of the National Health Insurance Scheme (NHIS) policy. The NHIS policy has been in existence for over a decade, however, challenges such as high patients’ turn up, inadequate personnel and other resources facing health care facilities have not received corresponding attention which can also militate against care coordination practice among health personnel [9]. In addition to the inherent challenges associated with the NHIS implementation mentioned above, most health care facilities are saddled with poor management of the NHIS in the delivery of services due to high rate of non-reimbursement as a result of errors in processing claim forms [9]. These findings therefore suggest that care coordination is a subject that is affected by a multiplicity of factors which must be addressed holistically in order to ensure good quality care for patients by nurses [6].
This finding agrees with Asah [12], who indicated that enrolment and utilization of the NHIS has influenced accessibility to health care facilities. Similarly, study conducted by Aryeetey et al. [9], indicated that outpatient visits increased by 51% and inpatient visits increased by 64% due to the introduction of the NHIS. This is because once a person subscribes to the scheme he or she can access healthcare at any time and in any accredited health care facility. Although no studies in Ghana have reported on limited access to services, Kotoh, Aryeetey and Van Der Geest [12] indicated that shortage and payment for drugs influence health care service delivery. Nurses sometimes face a lot of challenges in their pursuit to deliver quality care due to delays in getting access to patient medications and other important consumables that are not covered by the NHIS. The study also revealed that the delay in payment of the NHIS claims (M=4.3, SD=0.98) by the government, affects procurement of logistics needed for the provision of quality health care. This finding corroborates with previous studies [11,13] who indicated that claims submitted to government are not reimbursed. The delay in reimbursement of claims in both public and private health facilities has made hospital authorities charge for user fees to ensure sustainability of the health care institutions.
The findings showed that the facility is open to other private health insurance schemes’ subscribers (M= 4.0, and SD= 1.10). With the current challenges such as delay in reimbursement of the NHIS and inequality in health care services, many individuals and cooperate organizations have subscribed to various private insurance to ensure that members receive prompt and better health care services. Subscribers to these private insurances are given preferential services which are prompt and meet all the needs of members due to the regular payment of reimbursement to the healthcare providers. Procurement and supplies go through a lot of processes which impede the provision of quality healthcare. For instance, nurses often waste a lot of time on procedures due to low quality or ineffective materials such as non-functioning sphygmomanometer, disposal gloves and faulty oxygen cylinders. Consumables used by nurses to deliver care are often seen to be of inferior quality due to nurses’ non-involvement in the procurement processes. In spite of these, nurses manage to work with these inferior materials which results in a reduction in the quality of health services. The finding substantiates with that of Sekyere [14], who indicated that lack of finances, interference from top management, unqualified personnel and non -adherence to the procurement Act 663 were some of the factors influencing procurement performance leading to poor outcome of health care delivery
The Greater Accra Regional Hospital is a secondary health facility involved in the training of health professionals. Thus, the findings revealed that training of health professionals influence care coordination among nurses (M=4.2, SD=1.09). Training of health professionals is crucial to the delivery of quality health care to patients. This finding corroborates with Lehwaldt [15] who found that degree nurse education prepares nurses better to work together with other health care professionals. Trainee nurses who come to the hospitals from time to time as part of their training schedules do not only come to acquire practical experience but also complement the efforts of nurses. This brings relief and lessen burden of workload as these trainees come to augment nurses’ activities. Therefore, nurses gain adequate time to plan and implement patient care effectively in the unit. Additionally, the findings clearly indicated that partisan politics is a challenge to the stability of management in the hospital which in turn affects care coordination practice among nurses (M=3.4 and SD= 1.38). This finding also corroborates with the findings of Mosadeghrad [8] who emphasized that lack of management stability serves as impediment for managers to prolong their expertise. In Ghana, most top positions in the public sectors are occupied by party appointees. Managers including health sector are changed whenever there is a change of government. This often slows or delays infrastructural development and allocation of resources to the health facilities which affect quality health care delivery [15-26].
The role of nurses in the health care sector is key to quality health care delivery and patients’ satisfaction. External factors and patient characteristics positively influence the outcome of care coordination. This require that factors that influence care coordination among nurses such as inadequate resources, complexity of patient condition, NHIS challenges and institutional policies in the regional hospitals which negatively affect nurses care coordination are curbed to maximize quality of healthcare delivery in Ghana.
Nil.
There are no conflicts of interest.


