Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Gláucio Boechat Costa1*, Mark Paul Maggini Boechat2 and Juliana Maggini Leite Abreu3
Received: February 08, 2023; Published: February 21, 2023
*Corresponding author: Gláucio Boechat Costa, Master in Medicine, General Surgeon, Professor of Clinical Surgery at the Iguaçu University (UNIG), Campus V, Medical School, Itaperuna-RJ, Brazil
DOI: 10.26717/BJSTR.2023.48.007710
Abbreviations: CPhI: Chronic Post-Inguinal Hernioplasty Pain; GABA: Gabapentin Group; GPC: Placebo Control Group; VAS: Visual Analogue Scale
Inguinal hernia is defined as a protusion of an organ or abdominal content so through a defect of the abdominal wall in the inguinal region, regardless of whether it is congenital or acquired. These may be direct or indirect, medial or lateral, respectively, in relation to the lower epigastric vasculature. Inguinal hernia repair is today one of the most common operations performed in General Surgery. The popularization of surgical repair of inguinal hernia using the implantation of a prosthesis, globally known as “without tension”, promoted a dramatic reduction in the recurrence of this pathology, and is undeniably the preferred method of surgical repair of inguinal hernia (Goulart, et al. [1,2]). Inguinal hernia is the most common form of presentation of hernial pathology of the abdominal wall, corresponding to more than 70% of all surgical repairs, reaching the third cause of use of outpatient care in 2004. This condition, although not exclusive, affects males much more frequently, in a reason that can amount to 7-9:1 (male:woman), with the risk of developing an inguinal hernia during the course of life to amount to 27% in men and 3% in women (Prakash, et al. [3]). Women have, however, a more pronounced risk of relapse, mostly (up to 40%) in the form of femoral hernia. Although it can be bilateral in about 20% of cases, the most common side for the appearance of a hernia is the right, accounting for up to 55% of total cases (PRAKASH, et al. [3]).The higher incidence of right-sided hernia can be explained by a later descent of the right testicle, with respect to the patency of the processus vaginalis in indirect inguinal hernia; or by the high number of appendectomies performed, in which the incision can compromise the stability of the abdominal wall.
Among the risk factors for increased incidence, advancing age is also reported, and in women, this pathology manifests itself in a later age group. Interestingly, it was found that the increase in BMI of the individual can act as a protective factor, perhaps serving the thickening of the adipose layer as a barrier. It was thought that this finding could be biased by the greater difficulty in diagnosing hernial pathology in these individuals, however other studies in the area showed Agreement. Although the risk of death associated with inguinal hernia is relatively low, it can complicate with strangulation, which is the complication that reports the highest risk, also resulting in intestinal obstruction (PRAKASH, et al. [4-6]).Considering the numbers, the massive volume of hernioplasties performed annually projected the attention dedicated to pathology, due to the holistic limitations aroused in the individual, to a panorama not only clinical, but also socioeconomic (VARGAS, et al. [7]). As such, the current paradigm of successful intervention is, today, centered on the control of chronic post-inguinal hernioplasty pain (CPhI) and the provision of the best health-related quality of life, which minimizes the recourse to health care services and, at the same time, maximizes the individual’s fitness in professional and daily practice (MYLES, et al. [8]).
There are several motivators for the emergence and worsening of chronic pain complaints, factors intrinsically related to the patient, such as age and intensity of pain prior to surgery or characteristics of the hernia, such as laterality; the technique used, either without implantation of a prosthesis or with implantation of a prosthesis, the latter can be performed by an anterior approach or by later approach, which includes laparoscopic techniques; the type of prosthesis that, due to its biomechanical characteristics, can trigger discomfort and foreign body sensation, contributing to the perpetuation of pain; and, finally, also the fixation method, classically at the origin of tissue or nerve trauma if these are not properly identified, which can also be a source of contamination, or, on the other hand, allow the migration of the prosthesis, with extraordinary discomfort and increased risk of recurrence (ROSSI, et al. [9,1,10]). Postoperative pain is one of the main indicators of quality of life evaluated in hernia repair (SABISTON [8]). There are several studies for the treatment of chronic post-surgical pain, but there are practically no studies for acute pain. Thus, this chapter, which results from a master’s thesis in medicine, under the title efficacy of preoperative gabapentin in the control of postoperative pain in patients undergoing inguinal hernioplasty under spinal anesthesia (COSTA, et al. [11]), seeks to evaluate the dose of gabapentin that generates few side effects and, at the same time, confers comfort and postoperative analgesia to patients undergoing inguinal hernioplasty. In this perspective, the general objective is to investigate the effect of preoperative gabapentin administration on postoperative pain control in patients undergoing inguinal hernioplasty under spinal anesthesia. Still, for better direction of the investigation, some specific objectives emerged, such as:
1) To observe the incidence of postoperative pain compared to placebo treatment, at times 1h, 4h, 24h and also 30 days after surgery;
2) To compare the use of postoperative opioid analgesics among a group of patients who received gabapentin or placebo;
3) Observe the occurrence of side effects among the groups, such as: nausea, vomiting and sedation in the postoperative stage.
This is a prospective, randomized, double-blind, placebo-controlled study, whose hypothesis is that patients submitted to the anesthetic technique using gabapentin one hour before surgery will present lower postoperative pain indices on the visual analogue scale when compared to those treated with placebo, and that this benefit may extend beyond the period in which gabapentin is at effective plasma levels, which would characterize a preventive analgesia. In this study, all anesthetic and surgical procedures were performed by the same medical team. After clarification and obtaining consent, patients eligible to participate in the study were allocated to the Gabapentin group (GABA) or placebo control group (GPC) through a lottery. In the Gaba group, 900 mg of Pharmacy-manipulated gabapentin was administered in a single dose one hour before surgery. In the CPG, capsules made in a pharmacy containing Explotab, sodium lauryl sulfate, aerosil, mannitol, and microcrystallized cellulose were administered one hour before surgery.
After standard monitoring and venoclysis, patients were sedated with midazolan 1 to 5 mg. Then, they underwent spinal anesthesia with 0.5% hyperbaric bupivacaine 15 mg. After satisfactory lock level check. they underwent the surgical procedure. The surgical technique adopted was that of Lichtenstein (VARGAS, et al. [7]). Polypropylene Marlex screens were used. Its fixation occurred after reduction of the hernia and thorough dissection of the elements of the inguinal cord, with important care in identifying and preserving the ilioinguinal and genitofemoral nerves. Such fixation was done with 2-0 polypropylene nonabsorbable thread with vascular needle. Pain was evaluated according to the use of a numerical scale from 0 to 10, along with evaluation of side effects of gabapentin at 1h, 4h, 24h and 30 days after the end of surgery. The person in charge of the interview was not aware of the group to which the interviewed patient belongs. In case of need and/or demand on the part of the patient (pain scale ≥ 4), doses of morphine (0.5 mg/kg) were administered in the pacu with a minimum interval of 40 minutes between doses, and the doses used were noted for comparison. Morphine doses (0.05 mg/kg) were also prescribed for up to 6/6 hours postoperatively, when pain occurred.
This model of care made it possible to subsidize the important steps, such as listing the points of care and defining their attributions, instituting flows and clinical guidelines that guide the practice of care for these patients.
The APFEL and RAMSAY scales were used to classify patients ‘ PONV and sedation levels, respectively. For the RAMSAY scale, the score values range from 1 to 6, in which score 1 - anxious, agitated, restless - 2 -Cooperative, oriented, calm-3-responds only to commands- 4- fast response to mild stimulus, glabellar or high auditory stimulus - 5 - slow response to mild stimulus glabellar or high auditory stimulus - 6-does not respond to mild stimulus glabellar or high auditory stimulus (NAMIGAR [12]). The subpopulation studied was composed of 77 patients aged between 18 and 60 years, with a maximum BMI of 30, scheduled in sequence for surgery at the hospital São José do Avaí, Itaperuna-RJ. Patients with chronic opioid use, chronic pain, history of chemical dependence or those allergic to any of the medications used in the study were excluded from the protocol, as well as patients with any cardiac, respiratory, renal or hepatic pathology that is considered severe, BMI above 30Kg/m2, recurrent hernias and inguino-scrotal hernias.
The primary outcome was pain measured at times 1h, 4h, 24h and 30 days after surgery, and was evaluated by the visual analogue scale (VAS) ranging from 0 to 10, in which 0 is equivalent to no pain and 10 to the worst possible pain. The preoperative gabapentin group is expected to have less postoperative pain compared to the placebo group. As for secondary outcomes, the procedure was to initially evaluate the use of morphine in the postoperative period. Such medication was administered when the patient complained of pain, regardless of its classification. The possible side effects of gabapentin, such as altered level of consciousness and nausea/vomiting, were also evaluated. Such data were obtained using the PONV and RAMSAY classification. Referring to the statistical analysis plan, initially, the data were analyzed by descriptive statistics (means, standard deviations, distribution and coefficients of variation). Demographic data (sex, age, Total and adjusted weight, height, body mass index) between groups were evaluated by hypothesis tests for continuous measurements between two distinct groups. The null hypothesis that postoperative pain intensity would be equal was tested against the hypothesis that it would be different between groups, as well as all doses of medications used in the preoperative period. For data analysis, exploratory statistical techniques were used that allowed a better visualization of the general characteristics of the data.
In this sense, the data were presented in frequency tables with absolute frequencies and their respective percentages, as well as descriptive measures (mean, median, standard deviation, 25th and 75th percentiles) for quantitative data. Continuous variables were tested for normality by the Kolmogorov-Smirnov Test. The variables age, weight, height and BMI were compared by Student’s T-test. The variables pain and morphine dose were compared using the Mann-Whitney test. Categorical variables were compared according to the group using The Chi-Square Test and Fisher’s test when necessary. In all tests, the significance level adopted was 5%, so comparisons whose p-value was less than or equal to 5% were considered significant. The software used for the analyses was SPSS version 20.0.
The analyzed database consists of 77 patients, 38 of whom were in the Gabapentin group and 39 in the Placebo group. The groups are homogeneous in terms of gender, age, weight, height and BMI. Mean age of patients using gabapentin was 50.3 years (±13.1), and of the Placebo group 45.2 years (±14.1). Majority of males in both groups and mean BMI of 24.8 kg /m2 (Table 1). (Table 2) shows the clinical characteristics according to the treatment group. The hernia type and side showed no significant difference (p=0.323 and p=0.575), respectively. The mean anesthesia time was 69.4 (±17.8) min for the group using gabapentin and 70.2 (±20.0) min for those using placebo, showing no statistical significance, p = 0.870. The mean time to surgery was also similar in the two groups, 47.5 (±16.7) for the Gabapentin-treated group and 49.3 (±18.7) for the Placebo group, p= 0.660 (Table 2). Postoperative use of morphine in the ward was significantly lower in the gabapentin group compared to the placebo group. In the Gabapentin group, only 5.3% used morphine and in the Placebo group, 74.4%, p <0.001. Regarding the dose used, there was no significant difference, p = 0.953, both groups weighed median of 10mg. Only one patient used morphine in the postoperative period in the recovery room, being the same as in the Placebo group (Table 3).
Note: *Fisher’s test
**T-test; continuous data: mean (±SD);
Source: prepared by the author, (2020)
Note: *Chi-square test
**T-test; continuous data: mean (±SD); (95% CI)
Source: prepared by the author, (2020)
Note: *Fisher’s test
**Chi-square test
***Mann Test
Source: prepared by the author, (2020)
The pain evaluated by the Visual Analog Scale (VAS) was statistically significant when evaluated at 4h and 24h and 30 days postoperatively (p < 0.001). The Placebo group presented higher pain score values at all times evaluated, except 1 hour postoperatively. The highest degree of pain was after 4 h of surgery, presenting the median score of 6 in grupo Placebo, in this same period, the pain showed a median of 1 in the Gabapentin group, p< 0.001 (Table 4). The patients in this study presented a low proportion of Nausea and Vomiting in both groups in all postoperative periods, and there was no significant difference in the treatment used. All of the Gabapentin group did not use ondansetron and only one (2.6%) of the Placebo group used p = 1,000 (Table 5). According to the RAMSAY scale, most patients were cooperative/ calm in all periods evaluated and with similar proportions in both groups. In the first postoperative hour, 12 patients (31.6%) of the Gabapentin group were classified as sleepy and 7 (17.9%) in the Placebo group, but without significant difference, p = 0.129. After 4h and 24h postoperatively, the majority in both groups were calm/cooperative (Table 6). The patients presented a low proportion of headache in both groups and in all periods evaluated, and in those who presented, there was no need for medication (Table 7).
Table 4: Evaluation of pain in the periods 1H, 4h, 24h and 30 postoperative days according to the treatment group.
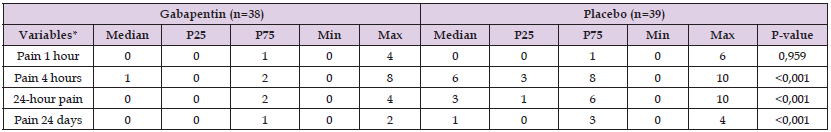
Note: *Mann-Whitney test
Source: prepared by the author, (2020)
Table 5: Evaluation of nausea and vomiting (PONV) in the 1H, 4h and 24h postoperative periods according to the treatment group.
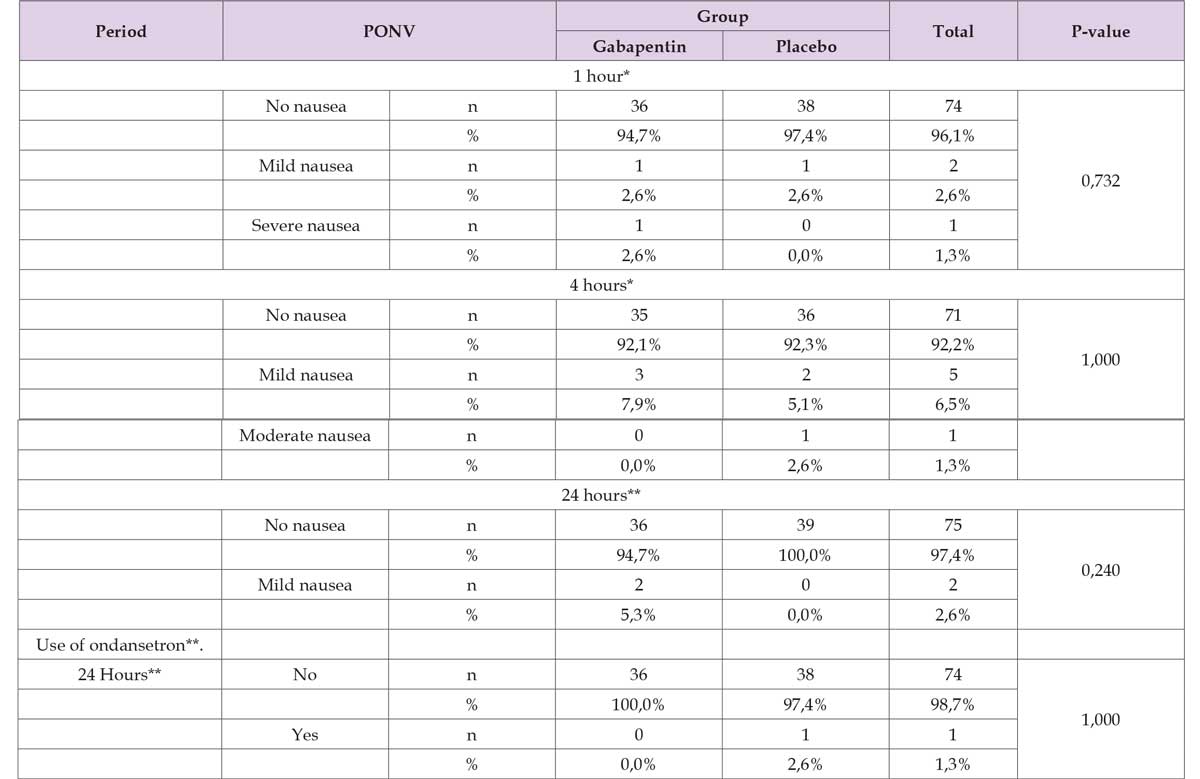
Note: *Chi-square test with Monte Carlo simulation (MMC)
**Fisher’s test
Source: prepared by the author, (2020)
Table 6: Evaluation of the degree of sedation in the 1H, 4h and 24h postoperative periods according to the treatment group.
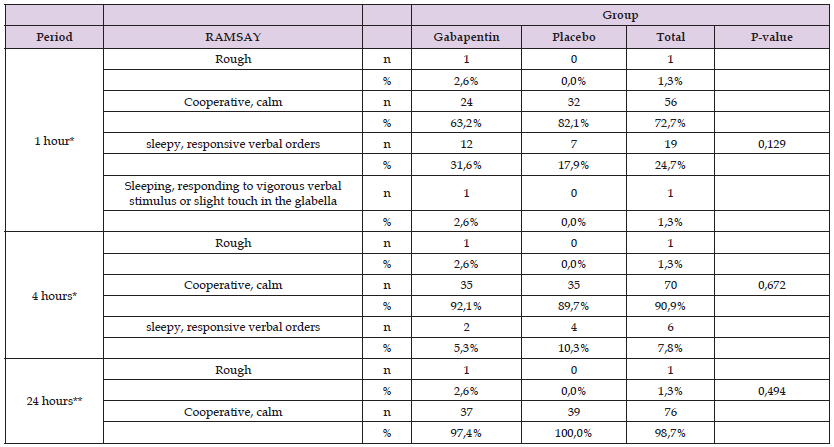
Note: *Chi-square test with Monte Carlo simulation (MMC)
**Fisher’s test
Source: prepared by the author, (2020)
Table 7: Evaluation of headache in the 1H, 4h and 24h postoperative periods according to the treatment group.
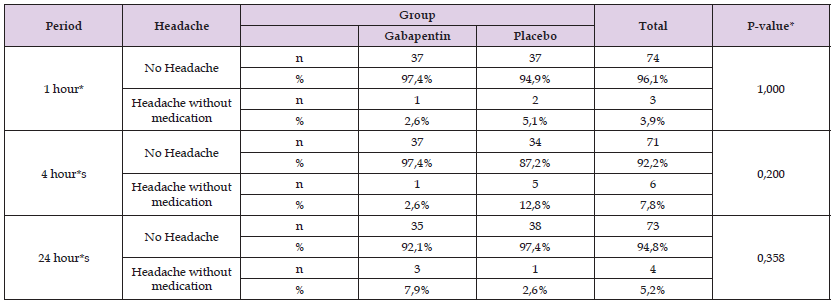
Note: *Fisher’s test
Source: prepared by the author, (2020)
According to Sabiston [13] one of the main quality indicators evaluated in hernia repair is postoperative pain (Sabiston [13]). There are few studies that associate acute postoperative pain with the preoperative use of gabapentin. Of the 77 patients included in the present study, 72 were male (36 allocated to both groups) and 5 females (2 in the gabapentin group and 3 placebo), and were therefore homogeneously distributed. This higher proportion of male patients is well described in the literature, in which 10% of the male world population is affected by inguinal hernias, in contrast, the female sex has a prevalence of 1% (FONTENELE SILVA [14]). Similar results were found in the Bourgouin study in which it was observed that 96.6% of patients were male and 3.4% were female (BOURGOUIN, et al. [15]). In the same study, patients undergoing hernioplasty had a mean age of 43.4 (±14.5) years. Results that disagree with the present study, which presented a mean interval of 50.3 (±13.1) years in the gabapentin group and 45.2 (±14.1) years in the placebo group. Already (LIEDBERG, [16]) conducted a study with an age range of 40 to 60. On the other hand, Sen et al. [17], in a prospective study, used an age range between 20 and 40 years. The systematic review by Teixeira, et al. [18] showed that hernias have a high incidence and about 75% of all hernias occur in the inguinal region, in addition, two thirds are of the indirect type, that is, it descends along the inguinal canal. In the present study, most patients had direct inguinal hernia in 44.7% of patients in the gabapentin group and 51.3% of patients in the placebo group, totaling 48.1% (37 patients) in both groups, corroborating the literature. In a study developed by Carvalho, et al. [19] in Porto Alegre, where the pain of 91 patients after inguinal hernioplasty was observed in the anesthetic recovery room, it was identified that, in the anesthetic recovery room, the participants presented mild pain, 56.5% of those who were submitted only to spinal anesthesia without the use of gabapentin. According to Sen et al. [17], surgical trauma can lead to severe acute postoperative pain, reaching 10% of cases. It also demonstrated that analgesia is usually unsatisfactory despite the use of local anesthetics, anti-inflammatory drugs, paracetamol and opioids.
Turan, et al. [20] describe the significant decrease in pain and the use of postoperative analgesics in patients who used 1.2g of preoperative gabapentin. However, they also observed a significant increase in adverse effects (nausea and vomiting) with such dosage. Even the result obtained Rowbotham [21], with the use of 1200 mg of preoperative gabapentin, which increased side effects. Gregg, et al. [22-24], in turn, demonstrated that doses of 300mg of preoperative gabapentin caused less nausea and vomiting but achieved little effect on analgesia. According to Clivatti, Sakata and Issy (2009), in order to achieve improvement in immediate postoperative analgesia, it seems sufficient to use a single dose of gabapentin preoperatively. The use of gabapentin in larger doses and for a longer period increased the incidence of related side effects such as sedation, vomiting and nausea. In the present study, a dose of 900 mg of preoperative gabapentin was used in order to evaluate postoperative analgesia with fewer side effects. The use of morphine in an assisted dose, as recommended by the anesthesia division of hospital São Jose do Avaí, (0.05 mg/kg) up to 6/6 hours, in the postoperative period was significant in the ward. In the Gabapentin group, only 5.3% were used for morphine and in the Placebo group, 74.4%, p <0.001. Regarding the dose used, there was no significant difference, p = 0.953, both groups weighed median of 10mg.
Also in this study, the pain assessed by VAS was statistically significant when evaluated in 4h, 24h and 30 days postoperatively (p < 0.001). The Placebo group presented higher pain score values at all times evaluated, except after 1 hour postoperatively. The highest degree of pain was after 4 hours of surgery, presenting a score of 6 in the placebo group. In the same period, pain was classified as 1 in the Gabapentin group, p < 0.001. This action ensured effective analgesia, which allowed the patient to reduce analgesic consumption. Although the effects of nausea and vômitos related to gabapentin are known, these symptoms did not reach significance in the present study. The patients presented a low proportion of nausea and vomiting in both groups and in all periods evaluated postoperatively, with no significant difference in the treatment used. This fact probably did not happen due to the dosage of gabapentin used. All patients in the Gabapentin group did not use ondansetron and only one (2.6%) of the Placebo group used it, p = 1,000. This reduction in the incidence of postoperative nausea and vomiting after gabapentin has the potential to improve patient recovery and reduce the number of readmissions after inguinal hernia correction. According to the RAMSAY scale, most patients were cooperative/calm in all periods evaluated and with similar proportions in both groups. In the first postoperative hour, 12 patients (31.6%) of the Gabapentin group were classified as sleepy and 7 (17.9%) in the Placebo group, but without significant difference, p = 0.129. After 4 h and 24 h postoperatively, the majority in both groups was calm/cooperative.
In this study, it was demonstrated that the effect of 900 mg of preoperative gabapentin on postoperative pain control was significant, as it ensured effective analgesia and decreased analgesic consumption due to the lower postoperative pain level when compared to the placebo group. Regarding side effects, patients presented a low proportion of nausea and vômito in both groups, in all periods evaluated postoperatively, with no significant difference. According to the RAMSAY scale, most patients were cooperative/calm in all periods evaluated and with similar proportions in both groups. Thus, the use ofG abapentinwas safe, with minimal adverse reactions and resulting in important postoperative analgesia compared to the Placebo group.


