Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Rustam G Khabchabov* and Elmira R Makhmudova
Received: February 08, 2023; Published: February 16, 2023
*Corresponding author: Khabchabov RG, Dagestan State Medical University of the Ministry of Health of the Russian Federation, Lenin Square 1, Makhachkala, 367000, Russia
DOI: 10.26717/BJSTR.2023.48.007695
Background: structural changes in the myocardium damage the antioxidant barrier of the cardiac conduction pathways, which contributes to the rapid oxidation of one or more ectopic nodes with the development of paroxysmal tachyarrhythmias. To evaluate the effectiveness of the complex treatment of paroxysmal atrial fibrillation and flutter (AF and TP), in comparison with monotherapy of an antiarrhythmic drug of the IC class - propanorm.
Methods: the study involved 63 patients with the first-occurring paroxysmal form of atrial fibrillation and flutter. Patients in the control group underwent standard therapy (propanorm, dabigatran), the study group used complex treatment (propanorm, sodium bicarbonate, Kudesan Q10, solcoseryl, dabigatran).
Results: the study showed; the combined therapeutic effect on the mechanism of atrial fibrillation and flutter with the structural pathology of the atria leads to a significant effect, in comparison with only one antiarrhythmic drug.
Conclusion: this effect is achieved due to additional antioxidant therapy with sodium bicarbonate and Kudesan (Q10), as well as the repository - solcoseryl.
Keywords: Flutter; Atrial Fibrillation; Reparents; Antioxidant Drugs
Abbreviations: AF: Atrial Fibrillation; CARAF: Canadian Register of AF; MI: Myocardial Infarction; WPW: Wolf-Parkinson-White Syndrome; cGMP: Cyclic Guanosine Monophosphate; EF: Ejection Fraction
Atrial fibrillation and atrial flutter (AF and TP) are treated by AHA/ACC/HRS experts as supraventricular tachyarrhythmia with uncoordinated atrial activation and, as a result, ineffective atrial contraction [1]. AF and TP affect 2.3 million people in the USA and more than 6 million in the EU countries. In Russia, it accounts for more than 40% of all arrhythmias, leading for hospitalization reasons among all cardiac rhythm disorders. Over the past twenty years, the frequency of hospitalisations for AF and TP has increased threefold, which is associated with an increase in its prevalence, with a simultaneous increase in resistance to pharmacological therapy [2]. The paroxysmal form makes up more than 40% of all cases of AF and TP, while in every fourth patient it is transformed into a permanent one.
Thus, data from the Canadian Register of AF (CARAF) show that 63% of patients with paroxysmal AF and TP experienced recurrences of arrhythmias for 5 years, while 25% experienced progression of the disease to a permanent form. Antiarrhythmic drugs have limited effectiveness in the treatment and prevention of AF and TP, and do not modify the structural substrate for AF and TP. Currently, there are few controlled clinical studies on the choice of an antiarrhythmic drug, taking into account the many mechanisms and causes of AF and TP. Therefore, modern algorithms for drug treatment of AF and TP should include the combined use of antiarrhythmic and non-antiarrhythmic drugs in order to comprehensively affect the causes and risk factors for the formation of this rhythm disorder [3].
Currently, there are four risk factors for trembling and fibrillation of the heart [4]:
1) Structural pathology of the heart - acute ischemia and myocardial infarction (MI), sclerotic and post-infarction heart failure, cardiomyopathy and heart defects with hypertrophy and dilatation, myocarditis, pericarditis, etc.;
2) The syndrome of weakness of the sinus node, which leads to passive heterotopia, while the main function of automatism can take on any ectopic node or nodes. A known fact of the development of brady-tahi syndrome is the development of atrial fibrillation on the background of bradycardia;
3) Thyrotoxicosis and hyperadrenal functioning of the adrenal glands with the development of prolonged tachycardia. As with Wolf-Parkinson-White syndrome (WPW), tachycardia contributes to excessive irritation of ectopic nodes and activation of heterotopia, including atrial fibrillation.
4) WPW syndrome. In WPW syndrome, it is known that additional pathways of the heart can retrogradely conduct an electrical impulse back to the atria, which irritates the ectopic nodes of the atria and there is an active heterotopia, most often paroxysmal tachycardia and atrial fibrillation.
In the literature, it is noted that with monotopic ventricular extrasystoles, Kudesan exchange rate dosage is 2 mg/kg/day. as part of complex therapy, it has a general anti-arrhythmic effect in 50% of patients, causing their complete suppression of arrhythmia in them and improving the results of basic therapy by 10% [5]. Long-term regular intake of Coudesan makes it possible to replenish its deficiency in the blood and body tissues, leading to a significant improvement in myocardial functional parameters, reducing the need for concomitant treatment with cardiovascular drugs in the complete absence of toxicity. Improvement of myocardial function became noticeable a month after the start of Kudesan, after 6 months. reached a maximum and subsequently remained stable against the background of coenzyme intake [6]. A study conducted by YuV Shubik and BA Tatarsky found that solcoseryl turned out to be a rather effective antiarrhythmic agent in the treatment of high-gradation ventricular extrasystoles according to B Lown, the effect of which is realized through membrane-stabilizing and antihypoxic effects on cells, including myocardial cells [7]. Citing the above data, we want to say that in the electrical work of the heart is not all clear. The occurrence of arrhythmias occurs due to some pathological processes that must also be affected. In a study conducted by Professor David Kass, an enzyme called PDE-5 was found to be responsible for disorders in the main pathways in patients with heart disease. In the same study, it was found that the PDE-9 enzyme is responsible for disorders in other pathways of the heart.
Earlier studies have shown that an excess of PDE-5 causes damage to the cardiac pathways, interfering with the cyclic guanosine monophosphate (cGMP) signalling molecule and the PKG protein. Subsequently, it was found that an excess of PDE-9 causes heart failure, fibrillation and cardiac arrest, disrupting the action of cGMP in the cardiac pathways. PDE-9 accelerates the breakdown of cGMP, which reduces the production of PKG protein. The researchers note that drugs that block PDE-9 activity are being tested in Alzheimer's disease and can be used to treat heart failure [8]. The following is the electrophysiology and developmental mechanism of AF and TP, which was taken as the basis for this study. This is a pathological process with demyelination of nerve fibres and the development of multiple sclerosis, in which nerve fibres lose their insulating myelin layer, and the work of the nervous system is destabilised. The myelin barrier helps to quickly carry out impulses from the brain cells to various organs along the axons, protecting the axons from damage. Due to the fact that ion currents cannot pass through myelin, the entrance and exit of ions is carried out only in the area of interceptions [9].
Electrophysiological processes in AF and TP. The antioxidant barrier existing in the heart between the myocardium and the pathways creates a connective tissue isolation membrane and T-cells. The insulating membrane starts from the sinus node and reaches the Purkinje fibres of the atria and ventricles, and the Purkinje fibres themselves lack this membrane, but they are enveloped in antioxidant T-cells that Purkinier described, considering that their main purpose is to conduct electricity, not to create barrier. These T cells are located between conducting B cells (Purkinje) and the myocardium itself. And if there is damage to the antioxidant barrier, then the myocardial intercellular fluid, which contains a large amount of Na+ and Cl- ions, and, therefore, more acidic, especially during hypoxia and acidosis, penetrates to the ectopic sites. Such hyperacidity leads to irritation of ectopic nodes, which normally should not occur. The destruction of the antioxidant barrier in the structural pathology of the heart is possible with PDE 5-9 enzymes, which David Casse described [10].
The mechanism of macro and micro-reentry wave formation during fibrillation and heart flutter. In the heart, there are proximal and distal ectopic nodes. The proximal ones are located in the major pathways of the heart: the tracts of Bachmann, Wenckebach, Torel, AV node, bundle of His, right and left leg. Distal ectopic nodes are located in the branches of the atria and ventricles, they are smaller than the proximal nodes, but there are more of them, as there are more branches than large pathways [11]. When one of the proximal ectopic site closest to damage is oxidized, it activates and paroxysmal tachycardia starts, and if the damage to the oxidative barrier of the connective tissue is insignificant, then we will see paroxysmal tachycardia on the ECG, since most of the electricity will pass to Purkinje fibres and excite myocardium in a natural way. But if the damage to the connective tissue oxidation barrier is significant, then most of the electrical impulse will go to the myocardium through the damage, and on the ECG we will see F atrial flutter waves, although this will be the same paroxysmal tachycardia. This is explained by the fact that the power of the emission of electricity directly into the myocardium through damage will be so powerful and unhindered that it will lead to an increase in atrial heart rate compared with the frequency of paroxysmal tachycardia [11]. How does a macro-reentry wave form during atrial flutter? It all depends on the angle of damage of the oxidative barrier of the connective tissue, which will form a certain vector of movement of an electrical impulse into a closed circuit or the path of rotation of the macro-reentry wave.
Fibrillation of the heart does not form one powerful release, as in trembling. Damage to the distal branches of the connective tissue or transitional T-cells will lead to the oxidation of 2–3 distal ectopic nodes less powerful than proximal ones. This will form several micro-reentry waves that will collide with each other, from which their movements will be messy and chaotic [11]. Accordingly, during the development of paroxysmal tachyarrhythmias with structural heart disease, the antioxidant barrier is damaged, their treatment should be complex. For this, it is necessary to use both antiarrhythmic and alkaline preparations to eliminate the over-oxidation of the conductive paths, as well as reparants, which should speed up the restoration of the integrity of the myocardium and the antioxidant barrier [11]. The aim of the study was to evaluate the efficacy and safety of complex treatment with reparants, antiarrhythmic and antioxidant preparations of patients with atrial flutter and atrial fibrillation, taking into account the above arrhythmia formation mechanism.
Investigated 63 patients with newly emerged paroxysmal form of AF and/or TP. Patients were treated in the cardiology department of the Republican Hospital No. 2 of the Ministry of Health of the Republic of Dagestan (Makhachkala) in the period from 2016 to 2018. Inpatient treatment lasted an average of 10 days, after discharge of patients, outpatient observation and treatment lasted 1 year.
Inclusion Criteria
The first emerged paroxysm of atrial flutter and atrial fibrillation, not more than seven days old.
Informed consent of the patient to participate in the study.
Exclusion Criteria
Permanent atrial flutter and atrial fibrillation.
The impossibility of prospective observation.
Participation in any other study.
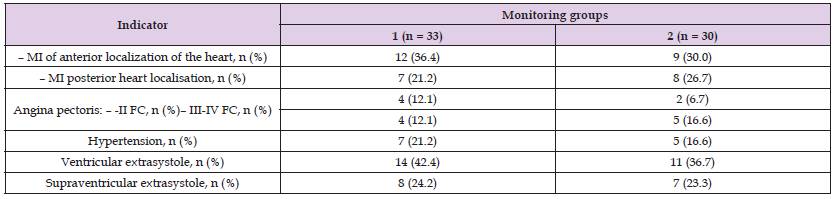
Patients were randomised to two groups by the random number method. Each patient was assigned a number from a table of random numbers. Then these numbers were ranked in ascending order, and in accordance with the selected rule were divided into two groups. Patients with even numbers were included in the first group (n = 33), which was the main group, with odd numbers - in the second group (n = 30), which was the control group. The ratio of men and women was 49 (77.7%) and 14 (22.2%), respectively (Table 1). The study included patients with cardiac and infarction wards with diagnoses: acute MI (n = 36), stable angina (n = 15) and arterial hypertension (n = 12) (Table 2). In the first group, the patients received the following therapy:
Note: For all these indicators, the groups were not statistically significantly different from each other (p>0.05)
Table 2: The initial characteristics of the studied patients (parameters CM-ECG, laboratory data and ECG signs of transferred MI).
Note: For all these indicators, the groups were not statistically significantly different from each other (p> 0.05)
Propanorm (PRO.MED. CA Prague AO) - the daily dose is 450 mg (150 mg three times a day every 8 hours). The dose is increased gradually (every 3–4 days) to 600 mg / day for two doses per day. The course of admission is 3 months.
Sodium bicarbonate 4% –200 ml i/v drip once, followed by switching to Kudesan Q10 (Akvion/Russia) - 10 drops (0.5 ml) two times a day with meals for 3 months, previously dissolving in a small amount of water.
Solcoseryl (SolcoBasel/Poland) - the drug was administered in 2 ml IV drip (previously diluted in 250 ml with 0.9% sodium chloride solution) for 4 weeks.
Patients investigated in the second group received Propanorm (PRO.MED. CA Prague AO) - the daily dose was 450 mg (150 mg three times a day every 8 hours). The dose was increased gradually (every 3–4 days) to 600 mg/day for two doses per day, within 3 months; Dabigatran was prescribed to all patients - an anticoagulant, a direct inhibitor of thrombin to prevent the development of thrombosis for the period before the restoration of sinus rhythm. The following research methods were performed for patients of both groups: daily, three times a day ECG examination using NeuroSoft (Ivanovo) computer program of Poly-Spectra; on the second day and in a month, daily monitoring of ECG (SM-ECG) using the “DiaCard” computer program of ZAO “Medicom” (Moscow); echocardiography - twice, at the beginning of the study and a month later. Statistical processing of the research results was carried out using the STATISTICA 6.0 software package (StatSoft, Inc, Tulsa, OK, USA). The analysis of the normal distribution of the traits studied was performed using the Shapiro-Wilk criterion. Quantitative information is presented as mean values standard deviations (M ± SD). The statistical significance of differences was assessed by Student's t-test for dependent and independent samples, with non-uniform distribution, the Wilcoxon non-parametric test (x2) was used. The statistical significance of differences or the effect of the shift due to treatment was assessed at p≤0.05.
According to the ECG results, in the first study group, the sinus rhythm (CP) of the heart recovered in 21 (63.6%) patients after 6 hours from the start of admission to hospital and treatment. In 7 more (21.2%) patients, the heart rhythm recovered after 48 hours from admission to hospital, and after 7 days CP of the heart recovered in the remaining 5 (15.1%) patients, respectively, in all 33 patients. The decrease from baseline values statistically significant (p<0.001). According to the results of SM-ECG, on the second day, paroxysmal AF and AFL were noted in 9 (27.3%) patients, after 1 year - in none of the patients (p<0.05) (Table 3). According to the ECG results, in the first study group, the sinus rhythm (CP) of the heart recovered in 21 (63.6%) patients after 6 hours from the start of admission to hospital and treatment. In another 7 (21.2%) patients, the heart rhythm recovered 48 hours after admission to the hospital, and after 3 months in the remaining 5 (15.1%) patients, respectively, in all 33 patients (Table 4). The decrease from baseline values statistically significant (p<0.001). According to the results of SM-ECG, on the second day, paroxysmal AF and AFL were noted in 9 (27.3%) patients, after 1 year - in none of the patients (p<0.05) (Table 3).
Note: the statistical significance of intragroup differences by t-test for dependent data (p1-2- between the first and second stages), n-number of patients with detected rhythm disturbances and u2 before and after Wilcoxon, step by step.
ote: the statistical significance of intragroup differences by t-test for dependent data (p1-2- between the first and second stages), n-number of patients with detected rhythm disturbances and u2 before and after Wilcoxon, step by step.
Note: p - the reliability of differences in the value of the index before treatment
When analyzing echocardiographic parameters after 3 months and 1 year, significant changes were revealed in both groups. In the main group 1, there was a significant increase in both the end-diastolic volume (RDC) of the left ventricle (LV) from 126.9 ± 4.3 to 134.7 ± 4.2 (p<0.05) and systolic volume (CSR) of LV with 73.6 ± 9.01 to 76.8 ± 3.5 (p<0.05). The total ejection fraction (EF) significantly increased from the original: from 42.7 ± 8.4 to 50.8 ± 3.1 (p <0.05). A significant (p<0.05) increase in the stroke volume (LV) of the LV from 55.0 ± 6.4 to 62.6 ± 5.1 was also noted (Table 5). In the second group, a significant increase in LV LV from 53.8 ± 4.9 to 58.9 ± 5.7 (p<0.05) was also noted. Changes in the remaining parameters studied were unreliable: LV CLW increased from 145.0 ± 37.4 to 146.9 ± 26.8 (p>0.05), LV CSR increased 83.2 ± 7.8 to 85.1 ± 32.6 (p>0.05), total EF increased from 42.6 ± 9.5 to 44.2 ± 68.9 (p>0.05). Thus, in the first group there was a statistically significant decrease in the number of patients with paroxysmal AFL and AF compared with the control group. If we draw a parallel between all patients who have had myocardial infarction with sudden structural restructuring of the heart myocardium and patients with prolonged structural restructuring of the heart - malformations, cardiomyopathies, aneurysms, etc., then we can say with confidence that in patients who have had myocardial infarction, the processes of regeneration of the pathways and the antioxidant barrier are restored, in contrast to patients with long-term pathology. Thus, out of 36 patients with acute MI, in 24 patients the heart rate recovered in the first 6 hours, versus 16 patients with other nosological heart diseases (p<0.05).
This suggests that suddenly developing necrotic processes of the myocardium can also quickly regress due to proper treatment, and long-lasting structural reorganization of the myocardium requires a more prolonged combined treatment. The results of the ultrasound examination of the heart also speak of the positive effect of antiarrhythmic treatment in combination with antioxidant treatment in the main group due to the long-term elimination of atrial fibrillation and the improvement of the metabolic processes of the myocardium. None of the groups showed any side effects from the therapy, all patients followed the treatment regimen prescribed by them, there were no failures and withdrawals from the study.
A one-year study showed that the complex pharmacological action on the causes of heart fibrillation and flutter leads to a significant short-term and long-term effect, compared with the use of only one antiarrhythmic agent. This effect is achieved through additional antioxidant therapy with sodium bicarbonate and Kudesan (Q10), as well as a reparant - solcoseryl. Monotherapy with propanorm probably leads only to anesthetic stabilization of ectopic foci, followed by the activation of the body's compensatory capabilities to restore the antioxidant barrier, which is important, but not always sufficient to restore heart rhythm.
The authors do not have financial support.
No conflict of Interest.
Not required (quality improvement project with need for consent waived by the institutional review board).


