Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Christian Camilo Galindez Guerrero1*, Carlos Felipe Duran Mendez1, John Jairo Zuleta Tobón2 and Edgar Augusto Arenas Marin2
Received:January 24, 2023; Published:February 14, 2023
*Corresponding author: Christian Camilo Galindez Guerrero, Gynecologist and Obstetrician, Universidad de Antioquia, Medellín - Antioquia, Colombia
DOI: 10.26717/BJSTR.2023.48.007684
Purpose: To assess whether belonging to the Afro-descendant population is an independent risk factor for developing complications of preeclampsia.
Materials and Method: Case-control study, including patients with severe PE hospitalized at the San Vicente Fundación University Hospital in Medellín (Colombia), between January 2014 and December 2019. Patients with severe PE complicated by acute kidney injury, cardiomyopathy, edema, pulmonary, eclampsia, cerebrovascular accident, hepatic subcapsular hematoma, abruptio placentae, intensive care unit admission for preeclampsia-related complications, or death, versus patients with severe PE who did not develop complications. A logistic regression was performed taking into account the clinical history of risk, the quality of care provided, the presence of Help syndrome, variables considered a priori as potentially confusing.
Results: 160 cases and 480 controls were included. A total of 216 complications were identified, the most frequent being eclampsia and acute kidney injury. The Afro-descendant race was not associated with an increased risk of complications of preeclampsia (OR: 0.91; 95% CI 0.49 - 1.65) while belonging to the subsidized social security scheme (OR: 1.82; 95% CI 1.14 - 2.88), the failure in the quality of care (OR: 2.08; 95% CI 1.37-3.15) and the presence of a clinical history of risk (OR: 1.63; 95% CI 1.09 - 2.67) were associated with an increased risk of developing complications of PE. Conclusion: African descent is not an independent risk factor for developing complications of PE.
Keywords: Race Relations; Preeclampsia; Pregnancy Complications
Preeclampsia (PE) is defined as the development of arterial hypertension (AHT) that occurs after the 20th week of gestation, associated with proteinuria and/or target organ damage. PE is classified as severe and non-severe. The severity criteria are given by appearance of hypertensive crisis, thrombocytopenia, elevated liver enzymes, renal failure, pulmonary edema and/or presence of «premonitory symptoms». However, as it is a systemic disease, complications can occur in all organs and systems [1]. In Colombia, according to the latest consolidated Public Health Surveillance System (SIVIGILA), for the year 2020, 14.6% of maternal deaths occurred due to hypertensive disorders associated with pregnancy (THAE) [2]. This figure is comparable to that presented worldwide, being among the first three causes of maternal mortality [3]. Historically, the Afrodescendant population has been considered to have a higher risk of presenting THAE, as well as an increased susceptibility to developing more severe forms of PE [4]. In addition, multiple studies indicate that the Afro-descendant population has a higher rate of maternal morbidity and mortality and hospital readmissions associated with PE [5]. However, in these patients there are other factors that could influence the risk of developing PE complications, such as belonging to the first quartile of income, having public social security or presenting a higher comorbidity index [6,7]. In studies carried out in countries where the majority of the population is Afro-descendant, The main objective of this study is to assess whether belonging to the Afro-descendant population explains the increased risk of developing PE complications or are other conditions present in this population that are really increasing this risk.
This is an observational analytical case-control study. Patients with severe PE were included, hospitalized at the San Vicente Fundación University Hospital (HUSVF) in the city of Medellín - Colombia, between January 2014 and December 2019. The HUSVF is a highly complex hospital and a reference site at the local level and nationwide that attends approximately 1500 deliveries a year. Cases and controls were identified from the HUSVF electronic record of medical records. Initially, the patients were filtered by the following diagnoses according to the ICD10 code: O10 (Pre-existing hypertension complicating pregnancy, childbirth and the puerperium), O11 (Pre-existing hypertensive disorders, with added proteinuria), O14 (Gestational hypertension with significant proteinuria), O14 .0 (Moderate preeclampsia), O14.1 (Severe preeclampsia), O14.9 (Preeclampsia, unspecified), O15 (Eclampsia), O15.0 (Eclampsia in pregnancy), O15.1 (Eclampsia during labor ), O15.2 (Eclampsia in the puerperium) and O15.9 (Eclampsia, unspecified period). The only exclusion criterion was ignorance of the woman’s race. Patients who met the criteria for severe PE established by the American College of Obstetrics and Gynecology (ACOG) 1 were included.
Admission to the intensive care unit (ICU) secondary to PErelated complications and death (described in the medical history). Patients with severe PE who did not present any of the mentioned complications were considered controls. The primary exposure variable was race. This breed was assigned subjectively according to the evaluators who recorded the information in the medical records. A woman was considered to belong to the Afro-descendant group if “black race” was recorded in the HUSVF electronic record the rest of the patients were in the non-Afro-descendant group. Guided by the objective, which is to assess the risk of complications once the PE has progressed to severe, the following variables were established a priori in the protocol as potential confounding conditions for the development of PE complications.
Risk Clinical History
Presence of at least one of the following antecedents: chronic hypertension, preeclampsia or eclampsia, chronic kidney disease, pulmonary hypertension, heart disease, any autoimmune disease, pre-gestational diabetes, multiple pregnancy and consumption of psychoactive substances, for which it was taken into account the information recorded in the clinical history by the treating team. These diseases have been reported in the literature as risk factors, not only for the development of PE, but also for its potential complication. The history of preeclampsia is evaluable only for women who have had a previous pregnancy, therefore, this variable was categorized into three groups: history of preeclampsia, no history of preeclampsia, and no exposure (nulliparous women). Quality of care provided. It is plausible to accept that the inadequate diagnosis and treatment of a woman with PE contributes to the development of the complication. Inadequate quality of care was considered in any of the following cases:
1. Patient with any of the severity criteria proposed by ACOG(1) in
2020 in whom PE was not classified as severe.
2. Patient with severe PE criteria according to ACOG(1) in whom
magnesium sulfate infusion was not started or infusion was not
administered for at least 24 hours postpartum or inappropriate
doses were used (bolus <4 grams, infusion <1 gram/hour).
3. Patient who presented two blood pressure measurements with
a difference of 15 minutes and found systolic blood pressure
above 160mmHg and/or diastolic blood pressure above 110
mmHg and antihypertensives were not started or when they were
used in inadequate doses or presentations, such as, for example,
an initial dose of labetalol less than 20 mg, use of prolongedrelease
nifedipine, dose Initial hydralazine less than 5 mg.
4. Patient who had expectant management with less than 26
weeks or more than 34 weeks of gestational age or those with
uncontrolled hypertensive crisis despite the use of at least two
antihypertensives at full dose, eclampsia, pulmonary edema,
abruptio placentae, persistence of premonitory symptoms or
stillbirth.
5. Patient with severe PE in whom fluid balance monitoring was
not performed during the hospital stay.
The Other Variables Collected in the Study Were
Marital status, residence, origin defined as the place where the first medical care is received, level of education, gestational age at the time of delivery in weeks, number of prenatal check-ups, number of pregnancies, primipaternity and type of delivery. In the planning of the study, which is recorded in the protocol evaluated by the Ethics Committee, sample size simulations were made, modifying the number of controls for each case, since the number of cases that were studied was not previously known. could find. It was expected that 25% and 15% of the women with and without a complication of preeclampsia, respectively, would be of African descent. With a confidence of 95% and a power of 80%, the necessary sample size calculation with a 1:3 ratio; It was 160 cases and 480 controls. The tabulation of the variables was carried out in the Microsoft Excel program and Google Spreadsheets. The qualitative variables are presented as absolute and relative frequencies, the quantitative variables as measures of central tendency (mean or median) according to the distribution of the data, previously evaluated with the Kolmogorov-Smirnov test. For the evaluation of the effect of the race in equal conditions of the other potential causes of complications, a logistic regression was carried out using the ENTER method. The outcome variable was the presence of a complication, defined as the presence of one or more of those already mentioned, and the exposure variable was the Afrodescendant population.
All variables considered a priori as potentially confounding were taken into account. independent of its p value in the univariate analysis, and additionally, variables that in the descriptive univariate analysis had a p value less than 0.25 and that could potentially be considered true risk factors for the evaluated outcome were taken into account. To carry out this regression, compliance with the different assumptions necessary for it to be valid was evaluated, and the results are presented in terms of adjusted OR with their respective 95% confidence interval. This research was carried out prior approval by the research department and the ethics committee of the Hospital San Vicente Fundación and was implemented according to the guidelines of resolution 8430 of October 4, 1993 of Colombia.
1959 medical records of patients admitted to the San Vicente Fundación University Hospital (HUSVF) in the city of Medellín - Colombia with a diagnosis of PE in the period between January 2014 and December 2019 were reviewed. 801 had a diagnosis of non-severe PE , 116 were excluded due to ignorance of race and [8] because they were referred to another institution by administrative order of their health provider entity (EPS). In the remaining 1,034 histories, 160 patients with severe PE with complications were identified. Of the remaining 874 patients with severe PE who did not develop complications, 480 controls were randomly selected, taking into account that they would have been seen in the same years of care as the cases. . The number of Afro-descendant women was lower than assumed in the calculation of the sample size, 69% of all patients resided in urban areas while 28.7% in rural areas. Only 20% of the total population received higher education and 1.3% did not receive any type of formal education; the level of education could not be established in 11.2% of the total number of patients. 22.6% of the women were single during pregnancy and the marital status was unknown in 7% of the population studied. The presence of primipaternity could not be determined in 48.7% of the total sample. One patient required management in the ICU without presenting complications related to PE. This patient had a history of pulmonary hypertension and admission to the ICU was due to decompensation of her underlying disease.
Note: *Mean values (Standard deviation) †Values are median (25th percentile and 75th percentile). ‡At least one clinical risk factor. Some patients presented more than one risk clinical history.
Note: *1 patient admitted to the ICU without complications related to PE is excluded.
Table 3. Associations of the different potentially confounding variables and the development of PE complications.
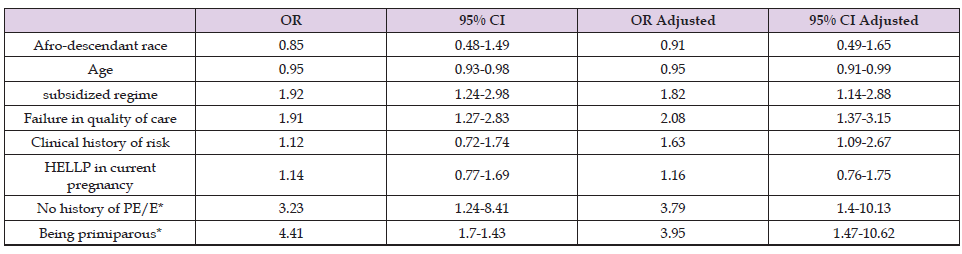
Note: *Compared with having pre-eclampsia in a previous pregnancy.
She subsequently developed PE without complications and was classified in the control group. Within the group of patients with PE with complications, there were 4 maternal deaths (Table 1). A total of 216 complications were identified (some of the patients developed 2 or more complications), the complication that occurred most frequently was eclampsia with 36.6% and acute kidney injury with 23.6%, the rest of the complications Complications can be identified (Table 2), and complications are distinguished according to Afrodescendant and non-Afro-descendant race. Failure in the quality of care was identified in 23.6% of the total population studied, there was a proportionally higher frequency of failures in the quality of care in Afro-descendant women compared to non-Afro-descendant women (28.7% vs 22 .8%), however, this difference did not reach statistical significance (p=0.24). There were more errors in the quality and the opportunity of the diagnosis in the group of cases with 8.8% while for the control group it was presented in 5.6% (p=0.16). The delay in the start of antihypertensive therapy was identified in 20.2% of the cases and in 17.3% of the controls (p=0.52). There was a higher proportion of failures to start magnesium sulfate in the PE group with complications versus the control group with 9.5% and 6.3% respectively (p=0.17). The crude and adjusted associations of the different potentially confounding variables and the development of PE complications (Table 3).
Other things being equal, the Afro-descendant race was not associated with an increased risk of PE complications, on the contrary, belonging to the subsidized social security regime, failure in the quality of care, and the presence of a clinical history were. risky. Univariate analysis (Table 1) found that not having had PE or eclampsia in a previous pregnancy, compared with having had it, was associated with an increased risk of developing PE complications in the current pregnancy, even after pregnancy. adjust for other factors. Compared to that same group.
Unlike previous publications, [7,9,10] this study found that, other things being equal, the Afro-descendant race does not behave as an independent risk factor for developing PE complications. On the contrary, failure in the quality of care, belonging to a public health regimen and having any of the risk clinical antecedents proposed in the study are independently associated with an increased risk of presenting complications. of PE. These latter findings were also found in previous studies, [7,11]. Many investigators have used race to assess differences in clinical outcomes. Unfortunately, even after controlling for socioeconomic indicators such as education, income, environmental exposures, and other risk factors, an increased risk of adverse health outcomes is sometimes observed among Afrodescendants [7,12]. This increased risk often presents as an intrinsic biological difference between races. However, it is likely that these «intrinsic differences» are actually related to unmeasured risks or exposures and that such expressions reflect the still existing racism [13]. In Colombia, the maternal mortality rate for the Afro-descendant population is 105.1 per 100,000 live births, while for the indigenous population and other races it is 236.5 and 55.6 per 100,000 live births, respectively 2 (Image 1). In other words, population minorities are the most vulnerable. Something that has been shown both in Latin America [14] and in the United States, where minority groups such as American Indians and Alaskan natives have an increased risk of developing PE and its complications [15].
These differences could be partially explained by socioeconomic, cultural, lack of of medical resources, inadequate implementation of medical management guidelines, lack of updating of health personnel or even biases given by the patient’s race in medical care, [14,16]. It is striking to find in this study that not having been exposed to a history of PE or eclampsia, even including primiparous women, was associated with an increased risk of PE complications in the current pregnancy. A possible explanation for this phenomenon could be that these patients had a rapid recognition of the symptoms and consulted the medical service in a more timely manner, although stricter surveillance of these patients by the health personnel could also be considered upon learning of their history [17]. Among the limitations of the study is the difficulty in identifying other types of delay in timely and adequate care for pregnant women [18], such as the lack of recognition of the problem by the patient, the time that elapsed between the presentation of symptoms and receiving medical care, the lack of resources at the first level of care, the transfer time from the first level of care to the referral center of greater complexity, due to the absence of recording these data in the medical records. It was also not possible to identify other factors that have been associated with an increased risk of developing PE complications [7,19], such as low socioeconomic status, The main strength of this study lies in having included conditions that determine poor quality of care and that were associated with an increased risk of developing PE complications. It is noteworthy that, in previous publications, despite having a larger number of patients, they do not take into account this important confounding variable, essential from our point of view to determine various clinical outcomes as has already been mentioned in previous research [7,16,20-27].
Our results are consistent with the hypothesis that Afrodescendant race per se does not have a cause-and-effect relationship with PE complications. On the contrary, an increased risk of developing PE complications is found in patients who presented factors that may be related to each other, such as failure in the quality of care and public health security. Based on our results, it is at least theoretically possible that, by impacting on modifiable factors such as reducing the failure rate in the quality of care, it could influence obtaining better outcomes with these women.


