Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Anastasia-Sofia Mindouri1, Evgenia Trevlaki2*, Emmanouil Trevlakis3, Nikos Mallios1, Georgios Domatas1 and Alexandra Xristara-Papadopoulou4
Received: January 21, 2023; Published: February 03, 2023
*Corresponding author: Evgenia Trevlaki, MSc Academic scholar of International Hellenic University, Greece
DOI: 10.26717/BJSTR.2023.48.007643
Background: Cognitive Behavioral Therapy is a form of non-pharmacological therapies of choice, including psychoeducation about pain, cognitive restructuring, problem resolution, relaxation and behavioral activation and has been documented to be effective in treating chronic pain. The purpose of this thesis is to describe recent research data on the effectiveness of this method in improving pain and functionality in patients with low back pain.
Methods: A search was conducted in electronic databases PubMed, google scholar, Pedro, ResearchGate and CINAHL for clinical trials since 2022 in Greek and English language, combining keywords of the central axes of the issue such as “chronic low back pain” or “CLBP”, “ cognitive behavioral therapy “ or “CBT”.
Results: From the initial search a total of 89 articles were found. After the removal of the duplicate (n=9) and the title/abstract screening (n=43), 80 studies remained. After the final screening of the full text, 16 studies were in agreement with the inclusion criteria and were included in the review. Most studies (n=7) examined the benefits of CBT at patients with chronic lumbar pain in all areas (economic method, more effective than medication, etc.), some (n=4) the benefits at chronic pain, (n=2) at patients with high fear of movement and (n=3) the benefits of online CBT.
Conclusion: The application of Cognitive Behavioral Therapy appears to have positive effects on pain intensity, disability, fear of movement, the ability to relax, manage pain, fear of movement, be active and enjoy things are observed.
Keywords: Chronic Pain; Low Back Pain; Cognitive Behavioral Therapy
Abbreviations: CLBP: Chronic Low Back Pain; CBT: Cognitive Behavioral Therapy; LBP: Low Back Pain; NSLBP: Non-Specific Low Back Pain; PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analysis; ACT: Acceptance and Commitment Therapy; MBSR: Mindfulness-Based Stress Reduction; UC: Usual Care Alone; SC: Supportive Care
Chronic pain [1] and chronic pain that frequently limits life or work activities, referred as high-impact chronic pain [2], are among the most common reasons adults seek medical care [3] and are associated with decreased quality of life, opioid dependence, and poor mental health [1,4]. Overall, the prevalence of chronic pain was 20.4%, and the prevalence of high-impact chronic pain was 7.4% (or 36.4% of adults who had chronic pain). [5]. Low back pain (LBP) is a persistent and aversive sensation localized to the lumbar region, associated with both sensory and emotional symptoms. It is a massive burden on patients, families, and the health care system, as 15 to 27% of adults suffer persistent LBP [6]. Persistent LBP or persistent nonspecific LBP (NSLBP) represents a complex interaction of physical, psychological, social and environmental components, including both genetic and cultural factors. [7,8] Chronic LBP is linked to high intensity pain, disability, psychiatric comorbidities (depression, anxiety, personality disorders, substance) and low quality of life. [9] The need of potential treatments to take the complexity of LBP into account and encompass a representative range of medical disciplines and disciplines allied to medicine, combined so as to offer maximum benefit to patients [10] has emerged [9].
Within this context, cognitive-behavioral therapy (CBT) has been established as one of the non-pharmacological therapies of choice [11,12], including psychoeducation about pain, cognitive restructuring, problem resolution, relaxation and behavioral activation. CBT, a form of psychological therapy, has been widely utilized in the treatment of chronic LBP. [11] The major goal of CBT is to replace maladaptive patient coping skills, cognitions, emotions and behaviors with more adaptive ones. [13] From a biopsychosocial perspective, CBT alone does not address all of the important variables potentially contributing to CLBP (e.g. biological factors) but may improve care for patients with psychological co-morbidities. [14] CBT is a form of psychotherapy that has been documented to be effective in treating anxiety, insomnia, depression, addictions, and other mental disorders. [13-22] The purpose of this review is the in-depth understanding of CBT in chronic spinal pain and the presentation of the results that can yield in different approaches, in certain pathologies, for its recovery.
Study Design and Strategy
The results are presented as per the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) reporting guideline (supporting checklist/diagram) [23]. For this review a global literature search was conducted in PubMed, Google scholar, Pedro, ResearchGate and CINAHL, combining keywords of the central axes of the issue such as «chronic low back pain» or «CLBP», «cognitive behavioral therapy « or «CBT». The process of selecting the articles will be presented in more detail in the (Flow Diagram 1). In the present review clinical trials examining the effects of CBT at LBP since 2022, written in the English and Greek language were included (Table 1).
Note: RCT = Randomized Controlled Trial, Qol=Quality of Life, NRS = Numerical Rating Scale, PCS=Pain Catastrophizing Scale, CBT= Cognitive Behavioral Therapy, QALYs=Quality-Adjusted Life Years, ODI=Oswestry Disability Index, BPI=Brief Pain Inventor, RMDQ =Roland and Morris Disability Questionnaire, ODS = Oswestry Disability Score, SC=Supportive Care, NRS =Numerical Rating Scale, CGI= Patient Global Impressions scale
Selection Process
From the initial search a total of 89 articles were found. After the removal of the duplicate (n=9) and the title/abstract screening (n=43), 80 studies remained. After the final screening of the full text, 16 studies were in agreement with the inclusion criteria and were included in the review. In more details, most studies (n=7) examined the benefits of CBT at patients with chronic lumbar pain in all areas (economic method, more effective than medication, etc.), some (n = 4) the benefits at chronic pain, (n=2) at patients with high fear of movement and (n=3) the benefits of online CBT.
Results
In Kayoko Taguchi et al. study [24] the effects of a CBT intervention program with attention-shift, memory work, video feedback, and image training components delivered via videoconferencing was examined. A total of thirty patients (age range, 22-75 years) with chronic pain were randomly assigned to two groups: vCBT (n=15) and TAU (n=15). The evaluation underwent at week 1 (baseline), week 8 (midintervention), and week 16 (postintervention. Only one patient from the therapist with treatment (TAU) group were not analyzed. At week 16 from baseline no significant difference was showed between the groups concerning the changes in pain intensity by the numerical rating scale scores (P=.36), while a significant improvement in the comprehensive evaluation of pain by total score of Brief Pain Inventory was observed (–1.43, 95% CI –2.49 to –0.37, df=24; P=.01). As fas as pain interference is concerned a significant improvement was seen by using the Brief Pain Inventory (–9.42, 95% CI –14.47 to –4.36, df=25; P=.001) and in disability by using the Pain Disability Assessment Scale (–1.95, 95% CI –3.33 to –0.56, df=24; P=.008) compared with TAU.
The incremental cost-effectiveness ratio for 1 year was estimated at 2.9 million yen (about US $25,000) per quality-adjusted life year gained. Although there was no reduction in pain intensity, catastrophizing showed a statistically significant improvement with a large effect size. Depression, anxiety, and disability showed statistically significant improvements, with small to moderate effect sizes.John W Burns et al. [25] conclude that there are reciprocal influences by which cognitive changes can produce improvements. A total of 168 participant were recruited and evaluated weekly for the 10 weeks of group treatment. The results showed that
(1) The two groups (CBT and EDU) presented a similar reduction at pain catastrophizing;
(2) Lagged analyses indicated that previous week reductions in pain catastrophizing predicted next week reductions in pain intensity and pain interference;
(3) Cross-lagged analyses indicated that previous week reductions in pain intensity and interference predicted next week reductions in pain catastrophizing and
(4) The relationships between pain catastrophizing and pain intensity and interference were moderated by session progression such that these links were strong and significant in the first third of treatment but weakened over time and became nonsignificant by the last third of treatment. The existence of reciprocal influences concerning cognitive changes may produce outcome improvements and vice versa.
The results from analyses of changes in slopes between pain catastrophizing and outcomes showed that both interventions were successful in decoupling pain catastrophizing and subsequent pain intensity and interference as treatment progressed. The relationships between pain catastrophizing and intensity moderated as the session progressed, early in treatment, but weakened over time and became more insignificant in the last third of treatment. At Martha MC Castro’s [26] randomized clinical trial, two parallel groups comprising 93 patients with chronic pain was carried out. Forty-eight patients were submitted to CBT and 45 continued the standard treatment. The visual analogue, hospital anxiety and depression, and quality of life SF-36 scales were applied. The evaluation took place before and after the treatment (Table 2). The results presented reduction of depressive symptoms (p=0.031) and improvement in the domains ‘physical limitations’ (p=0.012), ‘general state of health’ (p=0.045), and ‘limitations by emotional aspects’ (p=0.025) at the CBT group. The CBT showed significant improvements in more domains that the control group after the treatment, mainly in the quality of life.
Julie Loebach Wetherell et al. [27] study’s primary aim was to examine the efficacy of an ACT protocol designed for an outpatient primary care setting and compare it with CBT in individuals with diverse chronic pain conditions. The participants (N=114) with chronic (>6 months) pain were randomly divided in two groups: 8 weekly group sessions of acceptance and commitment therapy (ACT) and CBT after a 4-6 week pretreatment period. The evaluation was conducted after treatment and at 6-month follow-up. The results on ACT group showed improvements on pain interference, depression, and pain-related anxiety, while no significant differences in improvement between the treatment conditions on any outcome variables were observed. Αlthough there were no differences between groups, participants in the ACT who completed treatment reported better levels of satisfaction than participants in CBT in terms of it’s about chronic pain. Nanna Rolving et al. [28] investigated the effects of a group-based CBT intervention for patients with persistent LBP and psychological risk factors referred to secondary care. A total of 136 participants with chronic LBP and psychological risk factors. Among 136 participants, 68 (mean age: 41.7 years (SD 11.8)) were randomised to standard care and 68 (mean age: 46.0 years (SD 10.8)) were randomised to the intervention group. Except for age, baseline characteristics were comparable between groups. 12-month follow-up was completed by 92.6% in the intervention group and 80.9% in the standard care group. Both groups achieved significant improvements on disability, with a reduction of -4.8 points (SD 6.1) in the intervention group compared to -3.7 points (SD 5.2), resulting in an insignificant difference between groups. The secondary outcomes presented no significant differences. Nevertheless, a group pain management program was as effective as standard care for patients with persistent LBP (Table 3).
Mary O’Keeffe’s [29] randomized controlled trial examined whether a physiotherapist-delivered individualised intervention (CFT) was more effective than physiotherapist-delivered group-based exercise and education for patients with CLBP. The participants (n= 206) that experienced CLBP were randomized to either Cognitive Functional Therapy (n=106) or group-based exercise and education (n=100). The results of 6 months showed that CFT group reduced disability more than the group intervention (mean difference, 8.65; 95% CI 3.66 to 13.64; p=0.001), and at 12 months (mean difference, 7.02; 95% CI 2.24 to 11.80; p=0.004). Concerning the pain intensity no differences between the groups were observed at 6 months (mean difference, 0.76; 95% CI -0.02 to 1.54; p=0.056) or 12 months (mean difference, 0.65; 95% CI -0.20 to 1.50; p=0.134). The CFT presented significantly important reduction at disability, but not pain, at 6 and 12 months compared to the group exercise and education intervention.
.Economic evaluation alongside a randomized trial of CBT and mindfulness-based stress reduction (MBSR) versus usual care alone (UC) for chronic LBP was conducted from Patricia M Herman [30].
Table 2: Outcomes of intervention in all domains through cognitive behavioral therapy for patients with chronic lumbar spine pain.
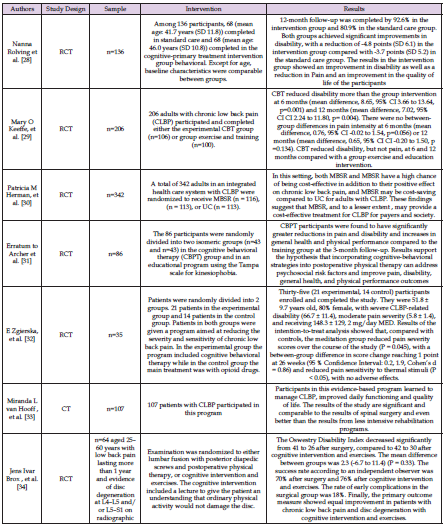
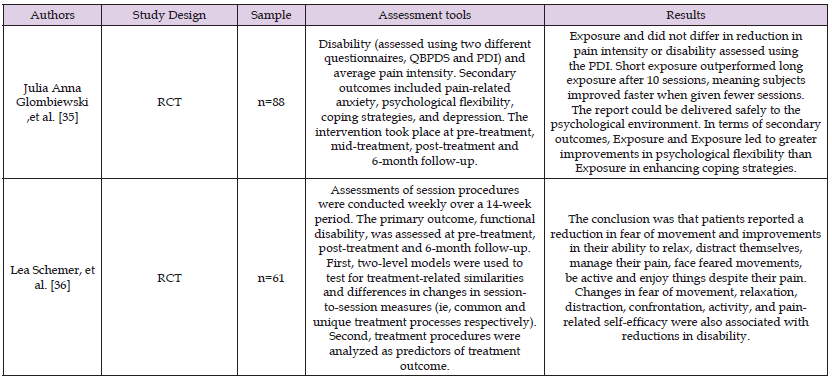
Table 3: Research suggesting that cognitive behavioral therapy has a significant effect on people who experience high fear of movement due to chronic low back pain.
The study 342 people with chronic LBP were randomly divided and underwent MBSR (n = 116), CBT (n = 113), or UC (n = 113). The first and the second group received 8-weekly 2-hour group sessions. Compared with UC, the mean incremental cost per participant to society of CBT was $125 (95% confidence interval, CI: -4103, 4307) and of MBSR was -$724 (CI: -4386, 2778)-that is, a net saving of $724. Incremental costs per participant to the health plan were $495 for CBT over UC and -$982 for MBSR, and incremental back-related costs per participant were $984 for CBT over UC and -$127 for MBSR. These costs (and cost savings) were associated with statistically significant gains in QALYs over UC: 0.041 (0.015, 0.067) for CBT and 0.034 (0.008, 0.060) for MBSR. The results showed that MBSR, and CBT at a lower level, may provide cost-effective treatment for CLBP for payers and society.
The study of Kristin R. Archer [31] examined the effects of a CBPT intervention in patients after lumbar spine surgery. A total of 86 patients that had undergo a laminectomy with or without arthrodesis for a lumbar degenerative condition participated. The evaluation took place pre- and post-treatment, and at a follow-up of 3-months. According to the multivariable linear regression analyses this intervention presented greater decrease in pain and disability, as well as in general health and physical performance compared with the education group. The results showed that CBPT can improve many factors in patients at risk after a spinal surgery. Aleksandra E Zgierska et al. [32] conducted a trial to assess the effects of mindfulness meditation and CBT for opioid-treated chronic LBP. A total of 35 patients, 51.8 ± 9.7 years old, 80% female (21 experimental, 14 control), participated in the study. The sample consisted of severe disability (66.7 ± 11.4), moderate pain severity (5.8 ± 1.4), and taking 148.3 ± 129.2 mg/day of MED. Both groups participated in a 26-week program. According to the results the meditation-CBT group showed a significant reduction in pain severity ratings during the study (P = 0.045), with between-group difference in score change reaching 1 point at 26 weeks (95% Confidence Interval: 0.2,1.9; Cohen’s d = 0.86) and decreased pain sensitivity to thermal stimuli (P < 0.05) compared with the control group. The pain intensity and sensitivity showed greater decrease in the meditation-CBT group relative to the opioid group (Table 4).
The mid-term effects of treatment in a cohort of patients with chronic LBP participating in an intensive pain management program was examined by Miranda L. van Hooff et al. study [33]. All parameters were measured at baseline, last day of residential program and at 1- and 12-months follow-up. A total of 107 patients with chronic LBP participated in this program. Mean scores on outcome measures showed a similar pattern: improvement after residential program and maintenance of results over time. Effect sizes were 0.9 for functioning, 0.8 for self-efficacy and 1.3 for physical functioning related quality of life. Clinical relevancy: 79% reached MCID on functioning, 53% on self-efficacy and 80% on quality of life. Study results on functioning were found to be 36% better and 2% worse when related to previous research on, respectively, rehabilitation programs and spinal surgery for similar conditions (SMR 136 and 98%, respectively).
CBT presented to be more significant and comparable even than spinal surgery and that it is better even than the results of less intensive rehabilitation programs. and the other participants in this research based on substantial evidence concluded that patients who took part in this program learned to manage chronic LBP, improved in daily functioning and quality of life and maintained these results longterm Jens Ivar Brox et al. [34] study aimed to compare the effects of
a CBT-exercise program with lumbar instrumented fusion in patients with CLBP and disc degeneration. A total of 46 patients 25-60 years old with LBP for more than a year and evidence of disc degeneration. The 97% of the participants underwent the 1-year follow-up visit. According to the ODI measurements the fusion group disability was reduced from 41 to 26 after surgery, compared to the CBT-exercise group from 42 to 30. The mean difference between groups was 2.3 (-6.7 to 11.4) (p= 0.33). The other aspects of examination, back pain, use of analgesics, emotional distress, life satisfaction, and return to work, presented no significant difference. The success rate was 70% after surgery and 76% after CBT-exercises. The early complication rate in the surgical group was 18%. Equal improvements was observed according to the primary evaluation for both groups.
Julia Anna Glombiewski et al. [35] study compared Exposure intervention and CBT among patients with CLBP with high fearavoidance models, and the short- (10 sessions) and long-term (6-month follow-up) effects of Exposure and whether this approach can be delivered in an outpatient psychological setting. The sample was comprised of 88 Caucasian participants (55% women) suffered from CLBP and high levels of pain-related anxiety and disability. The participants were randomized to three different psychological groups, Exposure-long, Exposure-short, and CBT. The short evaluation showed fast improvement with fewer sessions, while the secondary outcomes presented significant improvements in psychological flexibility than CBT group. The CBT group presented more effective than Exposure in improving coping strategies at all assessments (pretreatment, midtreatment, posttreatment, and 6-month follow-up).
In Lea Schemer’s study [36] the effects of Exposure and CBT treatment were compared. A total of 61 patients with CLBP (pain duration >3 months; sufficient level of fear-avoidance) from a three arm RCT were participated. Both approaches presented same treatment process. In more details, the results showed significant reduction in pain-management, fear of movement, relaxation, to deal with feared movements, and quality of life. All the previous reductions were related to disability reduction. Τhe effects of a videoconferencing CBT program was examined by Taguchi et al. study [37]. This program included new components (attention-shift, memory work, video feedback, and image training). A total of 30 patients participated and divided in two groups: vCBT (n=15) and TAU (n=14). Although no significant difference was found between the 2 groups in terms of changes in pain intensity by the numerical rating scale scores at week 16 from baseline (P=.36), there was a significant improvement in the comprehensive evaluation of pain by total score of Brief Pain Inventory (-1.43, 95% CI -2.49 to -0.37, df=24; P=.01).
Further, significant improvement was seen in pain interference by using the Brief Pain Inventory (-9.42, 95% CI -14.47 to -4.36, df=25; P=.001) and in disability by using the Pain Disability Assessment Scale (-1.95, 95% CI -3.33 to -0.56, df=24; P=.008) compared with TAU. As for the Medical Economic Evaluation, the incremental costeffectiveness ratio for 1 year was estimated at 2.9 million yen (about US $25,000) per quality-adjusted life year gained. The study’s findings showed that a videoconferencing CBT program can be an economical approach that reduce pain interference, but no pain intensity.Thomas Rutledge et al. study [38] comparted the effectiveness of telehealth CBT and supportive psychotherapy for CLBP. Sixty-one people, with daily lumbar pain for more than 6 months and more than 4 of 10 scale intensity, were enrolled and were randomly divided in CBT (12 sessions, 8-week) or to supportive care (SC). CBT group showed significant improvements on the RMDQ (mean = 11.4 [SD = 5.9] vs 9.4 [SD = 6.1] at baseline and post-treatment, respectively, P < .05; d = .33), NRS (mean = 4.9 [SD = 2.1] vs 4.0 [SD = 1.9], respectively, P < .05; d = .45), and on the CGI (39.1% reporting «much improved» or «very much improved»). SC participants (n = 31) also showed significant improvements on the RMDQ (mean = 11.1 [SD = 5.4] vs 9.1 [SD = 5.2], respectively, P < .05; d = .38), the NRS, (mean = 5.0 [SD = 1.9] vs 3.8 [SD = 2.1], respectively, P < .05; d = .60), and 26.7% reporting «much improved» or «very much improved» on the CGI.
Due to the high prevalence of chronic pain and the increasing emphasis on non-opioid therapies, training healthcare providers to provide cognitive behavioral therapies could be a cost-effective way to improve pain management. Telehealth CBT and SC approaches can provides significant and relatively compared improvements in people with CLBP. M. Gandy’s study [39] examined an internet-delivered CBT (iCBT) at patients with CLBP. The intervention was delivered through 15 SMS prompt with practice skills for chronic pain. A total of 85% rate was measured for the SMS to be helpful and would be recommended to others. Clinical improvements for those receiving SMS, at post-treatment and 3-month follow-up (disability, d = 0.44; 0.58; anxiety d = 0.50; 0.51; depression, d = 0.78; 0.79 and average pain d = 0.49; 0.54), were consistent with participant who had received the course previously without SMS (ps >0.05). According to the results the SMS prompts consisted an acceptable tool of CBT, although it showed no supplementary assistance. SMS prompts provided no further improvementat clinical outcomes of an established cliniciansupported iCBT program.
Over the past three decades, cognitive-behavioral therapy has become a first-line psychosocial treatment for people with chronic pain. [40] The dysfunctional way of thinking affects the patient’s mood and behavior, resulting in this condition intensifying various psychosomatic dysfunctions. Cognitive-behavioral therapy is based on the way of perception and understanding of each patient, that is, the specific beliefs and patterns of behavior. The therapist tries through various ways to achieve a cognitive change, i.e. a change in the patient’s way of thinking as well as his belief system so as to create a permanent emotional and behavioral change. Thus, when people learn to evaluate their thoughts in a more realistic and adaptive way, they experience improvement in their behavior as well as their emotions.In the present review a total of 16 studies were included. Most studies (n = 7) examined the benefits of CBT at patients with chronic lumbar pain in all areas (economic method, more effective than medication, etc.), some (n = 4) the benefits at chronic pain, (n=2) at patients with high fear of movement and (n=3) the benefits of online CBT. A total of 1802 participants were under examination.
As far as chronic pain is concerned CBT presented statistically significant results. All the studies that examined that field showed positive effects in catastrophic cognition, depression, anxiety and disability. According to Kayoko Taguchi, et al. [25-27,37], the intervention of CBT has been shown to have a positive effect when patients suffer from chronic pain due to psychological problems, because it helps to reduce pain as and stress and of depression related to it. JL Wetherell, et al. [27] results suggested that ACT is an equally effective and acceptable adjunctive intervention to CBT for patients with chronic pain. On the other hand, JW Burns et al. [25] argued that although at the beginning the results are very positive, as time passes, the effect of CBT on the patient decreases.
In addition, Kristin R Archer, et al. [31] and M C, Castro et al. [26] observed the effectiveness of CBT in patients after lumbar spine surgery for chronic pain. Jens Ivar Brox, et al. [34] argue that for pain due to disc degeneration more research is needed to have more correct statistical results. Another survey with led by Aleksandra E Zgierska [32] showed that angular-behavioral therapy for LBP can have better results even than opioid drugs can provide a more costeffective treatment. In the research of Patricia M Herman [30] noticed that CBT it can be cost-effective compared to other forms of treatment as well as Miranda L van Hooff [33] found CBT to be better than many rehabilitation programs. Then of interest are the conflicting opinions of researchers Julie Loebach Wetherell [27] and Mary O’Keeffe [29] where the first researcher’s group observes that CBT reduces chronic pain without particularly statistical data, while Mary O’Keeffe, et al. [29] argue that with group exercise and education intervention CBT reduced disability but not pain. On the other hand, Nanna Rolving, et al. [28] concluded that a group pain management program was just as effective as individual approach and patient care.
Other research such as that of Lea Schemer, et al. [36] suggests that CBT has a significant effect on individuals who experience high fear of movement due to chronic LBP. The results showed that a specialized and tailored program aimed at the sufferer’s psychological well-being and in doing so patients reported a reduction in fear of movement and improvements in their ability to relax, distract themselves, manage their pain, face fearful and dependent movements, be active and enjoy things previously avoided due to pain. While Anna Glombiewski, et al. [35] found that Exposure and CBT did not differ in reducing pain intensity or disability. The subjects showed faster improvement when given fewer sessions. In terms of secondary outcomes, exposure led to greater improvements in psychological flexibility than CBT, which was more effective than Exposure in enhancing coping strategies assessments took place at pretreatment, midtreatment, posttreatment, and 6-month follow-up.
Online rehabilitation is a condition that became well known in the last two to three years with the appearance and outbreak of the corona virus where for safety reasons patients had to be at home and so their only way of treatment was with the help of technology. In recent years and with the development of technology, a great interest has been observed from both health providers and patients, for the effect of online CBT on chronic LBP. According to research by Taguchi Kayoko, et al. [24], Thomas Rutledge, et al. [38] and M Gandy, et al. [39], telehealth treatments administered for chronic LBP can provide significant and relatively comparable benefits. Although the latest research believes that sms was an acceptable adjunct to iCBT for chronic pain, there is not much statistical evidence. Generally, the advantages of online recovery are that they can offer clinical assistance to patients from a distance using new technologies that allow the therapist to easily communicate with the patient through audio and video transmission, but at the same time it does not cease to be an economical way of treatment.
This review results demonstrated that CBT has many benefits for patients with chronic pain in the lumbar spine. Indeed, research has shown that the treatment has significant advantages over other pain management methods. A large percentage of patients showed an improvement in their clinical picture, as pain intensity, disability, fear of movement is decreased and improvements in their ability to relax, distract themselves, manage their pain, face fearful and dependent movements, be active and enjoy things are observed. While at the same time the cost of their health care decreased. Online CBT and ACT administered for chronic LBP can provide significant and relatively comparable benefits. This review concludes that incorporating cognitive-behavioral strategies into physical therapy can address psychosocial risk factors and improve pain, disability, general health, and physical performance outcomes. Integrating CBT into a physical therapy curriculum equips physical therapy students with the skills to identify and manage yellow flag patients early. Although all research has shown very significant and measurable benefits related to CBT in patients with chronic LBP, it is still a new and alternative form of treatment in the field of physical therapy. Further research could be conducted on alternative forms of treatment, such as CFT, and the benefits they may present compared to classical forms, but also among themselves. Follow-up data are lacking and further research are needed to examine whether the benefits remain long-term.


