Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Ning Du1,2, Ji-Guo Yu3 and YaFeng Song1*
Received: January 18, 2023; Published: January 27, 2023
*Corresponding author: YaFeng Song, Institute of Sports and Health, Beijing Sport University, Beijing, China
DOI: 10.26717/BJSTR.2023.48.007634
Adolescent idiopathic scoliosis (AIS) is a three-dimensional spinal deformity and characterized by progressive development during growth, and eventually to a curvature of the spine greater than 10 degrees on the posteroanterior radiograph. AIS usually does not present symptoms in early age, which makes the diagnosis and treatment of these patients difficult. Thus, a follow-up observation of all suspicious AIS patients becomes very important to monitor the progression of spinal cord deformity. Telerehabilitation is a new type of rehabilitation, which links the professional physiotherapists and the patients through telecommunication and information technology. Telerehabilitation can be synchronous (through any device real-time connection between patients and therapists), asynchronous (computer-based intervention for remote monitoring by the physiotherapists and offline adjustments), or a combination of both. The COVID-19 pandemic has caused medical health care system chaos and affected seriously the ongoing disease management in many countries. Telerehabilitation can reduce the spreading risk of COVID-19, the cost of faceto- face rehabilitation service, the pressure on the staff, and the financial burden on the patients. In this review, we briefly describe the development of telerehabilitation, its current status and related technologies, and its application in clinical practice of AIS. In addition, we discussed the limitations of the current telerehabilitation and its future prospection. We believe that telerehabilitation could provide high quality rehabilitation service to the patients, thus becoming the mainstream of rehabilitation to the population of AIS.
Keywords: Adolescent Idiopathic Scoliosis; Spinal Cord Deformity; Telerehabilitation; Telemedicine; Rehabilitation
Adolescent idiopathic scoliosis (AIS) is a rare type of spinal deformity, and occurs in adolescents around 10 years old, accounting for about 0.4% ~ 0.6% of the total population. AIS affects the entire growth period, and the spinal cord deformity may continue into adulthood (Bondar, et al. [1,2]). Scoliosis is characterized by a threedimensional structural change in the coronal plane of the cone with a lateral flexion of more than 10 degrees, spinal axis rotation and a flat sagittal physiological curve. The patients may be accompanied with disability, cosmetic deformity, pain, limited mobility, lower quality of life, and respiratory dysfunction (Tan, et al. [3-6]). In clinic, conservative treatment (exercise and brace treatment) and surgery are the conventional routines of treatment in the patients (Negrini, et al. [7]). However, Brace wearing may induce physical pressure, uncomfortable feeling and limited mobility, which may cause psychological burden to the patients (Maclean, et al. [8,9]). Surgery is an effective alternative in reducing the deformity, yet it would not improve the strength of the relevant muscles (Westrick, et al. [10]), and the surgery induced pain and the high risk of complications during the long postoperative recovery time are also the potential problems. Therefore, therapeutic physical exercise is more acceptable to the patients and their families than the abovementioned conventional treatments (Stefano, et al. [11,12]). For the patients of AIS, the major purpose of therapeutic physical exercise is to prevent the progression of spinal cord deformity following maturation, to increase the muscle strength and flexibility of the spine, to improve cosmetic appearance, to enhance cardiovascular and respiratory functions, and to prevent or alleviate spinal pain syndrome (Flores, et al. [13,14]). The therapeutic physical exercise interventions for patients of AIS include Schroth, individual functional treatment, and scientific exercise approach of scoliosis (SEAS) (Amrici et al. [15,16]). Others therapeutic exercises such as core stabilization exercise, Pilates, and Yoga are also popular conservative treatments (Yagci, et al. [17]).
COVID-19 has caused chaos in medical health care system in many countries, and increased dramatically the difficulty of seeking medical treatment for patients who have physical therapy needs. The closure of outpatient services or travel restrictions have forced people to choose between closing down or switching to telerehabilitation, thus, the COVID-19 promotes the development of telemedicine (Shah, et al. [18]). In a recent study, the data revealed that by June 2020, 93% of medical institutions in Italy have suspended rehabilitation services and outpatients visiting, resulting a passive transition to telemedicine including telerehabilitation where it is possible, while maintaining emergency on-site visits (Ghislandi, et al. [19]). This review was based on the knowledge searched on the following databases (up to 31 October 2022) of mainly English publications: Science Citation Index Expanded, MEDLINE, PubMed, EMBASE, Engineering Index. The search terms are ‘telerehabilitation’, ‘telemedicine’, and ‘adolescent idiopathic scoliosis’, and their combinations of the following query: (‘telerehabilitation’) OR (‘telemedicine’) AND ‘adolescent idiopathic scoliosis. The major aim of this review was to raise awareness of the current achievements and potential applications of telerehabilitation in the field of AIS.
In the 1960s and early 1970s, telemedicine began with telemetry electrocardiogram and health care telemetry in monitoring of astronauts during space flight (Nicogossian, et al. [20]). The development of telemedicine can be roughly divided into three stages: the early 1960s to the mid-1980s as the initial stage, during which the development was slowly (Teoli, et al. [21]). The second stage began from the late 1980s to the late 1990s when the communication and electronic technology developed continuously, and the United States and Western European countries made a great progress in remote consultation and long-distance transmission of medical images (Yano, et al. [22,23]). The third stage began from 2000s till present, when telemedicine is in a rapid and comprehensive development period, and plays an important role in medical diagnosis and treatment (DM Brennan, et al. [24]). COVID-19 has led to a rapid transition to telemedicine, as evidenced by a study where more than 40% of the medical working began using telemedicine after the epidemic lockdown («Epilepsy care during the COVID-19 pandemic,» 2021). Telerehabilitation refers to the use of information and communication technologies to provide rehabilitation services to people remotely in their home or other environments (D Brennan, et al. [25]).
Telerehabilitation develops along with telemedicine and is applied to more and more patients of various kinds of diseases. Data has shown that telerehabilitation has significant effects in reducing pain and improving the quality of musculoskeletal (Adamse, et al. [26,27]). In the field of neurorehabilitation, telerehabilitation helps to improve physical activity levels and balance in patients of multiple sclerosis (Amatya, et al. [28]). In addition, telerehabilitation is more convenient, flexible, and easier to access compare with traditional faceto- face cardiac rehabilitation (Subedi, et al. [29]), and it has similar outcomes as the conventional rehabilitation in reducing dyspnea in patients of chronic obstructive pulmonary disease (Ambrosino, et al. [30,31]). Telerehabilitation was also effective in reducing overweight and obesity and improving physical condition and quality of life in cancer survivors (Kopp, et al. [32]).
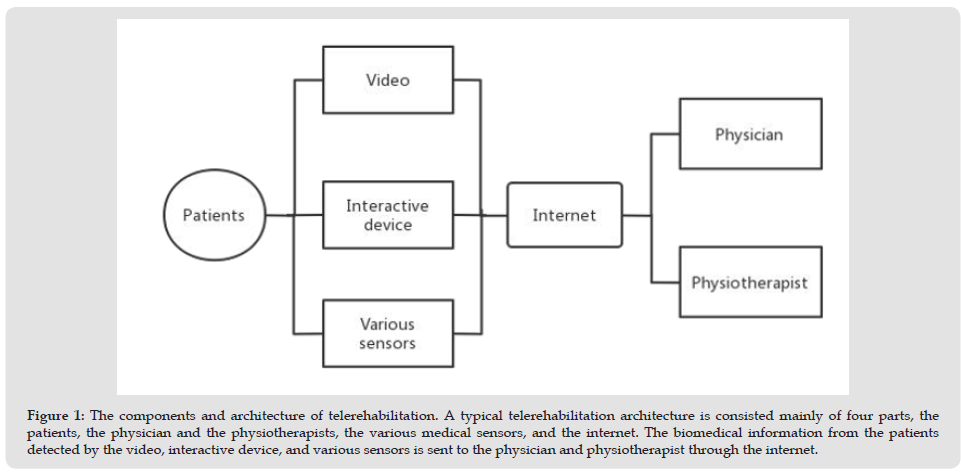
Telerehabilitation is based on information and communication technologies, and it is vitally important to establish an accurate clinical practice system architecture. (Figure 1) shows the components and the architecture of telerehabilitation. As shown in the figure, communication facilities such as information technology, internet of things, medical sensors, and virtual reality technology are essential in telerehabilitation (Saptono, et al. [33-36]). Information Technology is a big family including Big Data, Cloud computing, Internet of Things. Big Data is characterized by huge amount of data, fast processing speed and authenticity (Baladrón, et al. [37]). Application of Big Data in telerehabilitation helps the physiotherapists to diagnose, optimize treatments, and conduct remote monitoring. Telerehabilitation systems focus on visual observation and tactile perception of different body sites of the patients, as well as the patients’ subjective responses to various pressures, temperatures, and humidity, which form two-dimensional, three-dimensional, and even multi-dimensional information (Jager, et al. [38]). In telerehabilitation, Big Data provides the physiotherapists the possibility to remote monitor the process of treatment and make adjustment in real time. Cloud computing can provide patients available, convenient, and on-demand access of network, and by which the physiotherapists and the patients can share a configurable computing resource pool (including network, server, storage, application software, services, etc.), which can be quickly established and does not need too effort to manage (Sethi, et al [39,40]).
Figure 1 The components and architecture of telerehabilitation. A typical telerehabilitation architecture is consisted mainly of four parts, the patients, the physician and the physiotherapists, the various medical sensors, and the internet. The biomedical information from the patients detected by the video, interactive device, and various sensors is sent to the physician and physiotherapist through the internet.
In telerehabilitation, the physiotherapists prescribe the physical exercise to the patients through cloud platform and adjusts the prescription according to the follow-up assessments. The internet of things was formally proposed by the International Telecommunication Union (ITU) Internet Report 2005 and was released by the ITU at the World Summit on the Information Society held in Tunis in 2005 (Meeker). Through radio frequency identification, infrared sensors, global positioning systems, laser scanners and other information sensing devices, many items are connected to the internet of things for information exchange and communication according to the agreed protocol to achieve intelligent identification, positioning, tracking, monitoring and management (Kumari, et al. [41,42]). In telerehabilitation, the internet of things plays an important role in remote data collection and remote monitoring. Medical sensor has a big family, including pressure sensor, acceleration sensor, vibration sensor, biochemical sensor, temperature and humidity sensor, etc., and is characterized by intelligence, multi-parameter, remote control, non-invasive, and miniaturization (Lupton, et al. [43]). Medical sensor can collect human physiological parameters through electric nodes, and after raw data brief processing, the data can be transmitted to the cloud platform through wireless communication (Annaswamy, et al. [44]).
Thereafter on the cloud platform, the data can be further processed and then sent to the database centers where the experts of physiotherapists can evaluate the data and provide real-time feedback to the patients. With the development of technology in medical sensor, micro-wearing devices in combination with wireless technology are presently widely used, which is able to measure a variety of physicochemical parameters and is becoming a fundamental feature of health care and rehabilitation in the future (Sang, et al. [45]). The virtual reality technique is a computer system that can create a virtual world by using computer graphics, simulation technology, multimedia technology, artificial intelligence technology, computer network technology, parallel processing technology, and multi-sensor technology to simulate the functions of human visual, auditory, tactile, and other sensory organs (Berton, et al. [46]). It enables people to immerse themselves into the virtual environment generated by computer and to interact with it through natural ways such as language and gestures. The virtual reality technique has the characteristics of immersion, interaction, and conception, by which the patients produce a sense of reality, achieve human-machine harmony, and generate creative thinking (Llorens, et al. [47]). The virtual reality technique is currently widely used in telerehabilitation, as it makes the rehabilitation exercises more scientific and interesting, shorter in training time but more effective. The rehabilitation for patients of AIS is generally tough and long period; nevertheless, the application of virtual reality in rehabilitation can stimulate the patientsʹ enthusiasm and initiative as virtual reality can generate real-time images by which patients can adjust their training posture and movement (Lei, et al. [48]).
The rehabilitation for patients of AIS requires attention of both recovery from the current diseases and prevention of potential development of secondary disease. Therefore, the rehabilitation for patients of AIS needs to have extra attention on the evaluation of bone maturity and the scoliosis progression. Therefore, on early stage of AIS, i.e., when the Cobb angle is less than 25 degrees, the patients need to have routine examination and review of X-ray films every 4-12 months. In the meanwhile, the patients need posture training and corrective gymnastics (Kuznia, et al. [49]). In addition, at this stage if the scoliosis angle tends to develop, the patients need to wear brace, as brace treatment can delay the progression of scoliosis in patients. On the second stage of AIS, i.e., the Cobb angle is in the range of 25- 40 degrees, and the patients are given brace treatments, especially those with premature bone with high bone growth potential between the ages of 10-20 years old. In the meanwhile, some patients may need extra treatments such as electrical stimulation on paravertebral muscles, posture training, and corrective gymnastics (Sung-Mok, et al. [50]). On the third or final stage of AIS i.e., the Cobb angle is greater than 40 degrees or the patients’ annual review of Cobb angle progression is greater than 5-10 degrees, the patients need surgical treatments. Before and after the surgical treatment, specific corrective gymnastics and posture training is needed to help improve and consolidate the surgical results (Hensinger, et al. [51]).
Studies have shown that surgery and brace wearing could induce significant reduction in health status in patients of AIS (Weinstein, et al. [52]), as surgery could induce pain and seriously affects the quality of life of the patients. Exercise therapy plays an important role in the conservative treatment of AIS patients, thus becoming very popular in the field of rehabilitation. In recent years, data has shown that high-intensity exercise therapy is very effective and widely used in patients of AIS (Lau, et al. [53]). In addition, target training on the muscles along the deformed spinal cord is also widely used as it could effectively prevent the deterioration of spinal cord deformity and enhance patients’ awareness of right postures. As an important part of the rehabilitation, the family members also need to be trained for assisting the patients’ physical exercise training. It is important to note that for the patients of AIS with poor prognosis, during the time of training while wearing the orthopedic braces, they need to be regularly checked for the brace. The braces also need to be adjusted to make it suitable for the current status of the spinal cord deformity during the process of recovery of the AIS patients. In addition, if cardiopulmonary function limitation appears in the AIS patients, it is necessary to perform corrective breathing exercises and respiratory therapy. To prevent muscle atrophy and postoperative complications, electrical stimulation and muscle static contraction training are commonly used, especially in the early stage of rehabilitation.
Presently, telerehabilitation has been applied to patients of various diseases and obtained remarkable achievements; however, research of telerehabilitation on patients of AIS are rare. (Table 1) summarized the current available studies (Table 1). In an early study (Lotan, et al. [54]) applied telerehabilitation of a 12-week individualized physical training program on patients of AIS and observed significant improvements in daily activities in the patients. The effectiveness of the telerehabilitation was closely associated with the improvement in gross motor skills of the patients. The telerehabilitation program even provided the chance to the patients’ family members to learn the rehabilitation process, which was believed to be very helpful in the patients’ rehabilitation. As shown in (Table 1), most of the previous studies focused on devices of monitoring of body reactions to telerehabilitation in patients of AIS. (Chalmers, et al. [55]) compared the prediction of scoliosis brace treatment between human scoliosis experts and fuzzy models using conditional fuzzy C-means clustering to construct a personalized analysis of patients’ data. The results showed that the fuzzy models could provide meaningful brace treatments to the patients similar as that of the scoliosis experts. (Lou, et al. [56]) developed an intelligent brace system to monitor the brace load on the patients in their daily life. The system records realtime data which is sent over the internet to realize remote monitoring of the patients.
Note: GRF: ground reaction forces; GRMs: ground reaction moments; RTT: Rett syndrome.
The system can help medical workers review patients’ data and provide further instructions, and continuously monitor the deformity and to optimize the treatment. To make the brace system to reflect the real-time pressure on the trunk and more comfortable for the patients to wear, the active intelligent brace system can help patients to have a proper interface pressure of a specific range and observed that wearing the system can significantly extend the wearing time of the brace. To predict the ground reaction forces and ground reaction moments during walking, (Sim, et al. [57]) used wavelet neural network to collect the insole plantar pressure information to help improve the gait of AIS patients. Spine exoskeleton robots has also been used in telerehabilitation, which can control the position and orientation of specific cross-sections of the human torso while measuring the forces and moments applied to the body, providing the possibility of 3D dynamic treatment of scoliosis (Park, et al. [58]). In a study on 20 Rett syndrome participants with scoliosis, (Romano, et al. [59]) applied a 6-month individualized training program on the patients, during which the patients received remote supervision for the first two weeks. The telerehabilitation effectively prevented the progression of scoliosis in the patients, and the patients had better muscle balance. (Caesarendra, et al. [60]) developed an anteriorposterior spine X-ray image automation system to measure the spinal curvature in AIS patients. The system used deep learning convolutional neural network methods, including U-Net, Dense U-Net, and Residual U-Net to separate each individual cone. The results revealed that the system could result in better cone angle evaluation than human scoliosis experts.
Although telerehabilitation has develops rapidly, it still has some obstacles for providers and caregivers. Firstly, telerehabilitation is an emerging product of the Internet era, thus many people lack correct understanding of it, and have some concerns about the effectiveness of telerehabilitation. Secondly, telerehabilitation requires reliable broadband Internet access, high quality of hardware, and technical support as well as a wide variety of platforms. In addition, the rehabilitation outcome assessment of scoliosis requires detailed physical examination (such as body shape examination, spinal mobility measurement, neurological function assessment), and in some cases special measurements. Presently, the telerehabilitation still has difficulties in completing a comprehensive physical examination and accurate assessments of the functional status. Compared with face-toface rehabilitation, telerehabilitation cannot provides offline actual examination and carefully care for patients, thus, a good doctorpatient relationship is hard to establish[61].
All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
This work was supported by The National Natural Science Foundation of China to YF Song (H0911-82071413).
The authors declare that they have no competing interest.


