Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Hayam A Elawamy1, Eman Z Younis2*, Fawzia A Al majberi3 and Mohamed M Nagem4
Received: January 05, 2023; Published: January 26, 2023
*Corresponding author: Monisha Mohan, Department of Science and Humanities, Indian Institute of Information Technology, Design and Manufacturing, Kancheepuram, India
DOI: 10.26717/BJSTR.2023.48.007628
Background: Cryptosporidium spp., is the most common parasite that infects a large variety of humans and animals. Cryptosporidiosis is an Infection caused by Cryptosporidium; a protozoan that can live in the gastrointestinal tract of humans and animals and goes through the stool of an infected animal or person and causes diarrhea in humans, wild animals and domestic. Its infection remains a major health problem. These opportunistic parasitic diseases are threatening the life of many children and immunocompromised patients.
Objective: We aimed to estimate the prevalence of cryptosporidiosis and other correlations with parasitic intestinal infection among individuals attending Al Akeed Medical Laboratory in Benghazi. A total of 1340 fecal specimens from patients attending Al Akeed laboratory (aged > 1 to 75 years) from different hospitals of Benghazi, Stool samples were analyzed microscopically and screened for Cryptosporidium species using the modified Ziehl Neelsen stain.
Result: Out of all 1340 collected samples, the prevalence of cryptosporidiosis was 30% (402 out of 1340), and 402 were observed positively by (mZN). The odds ratio was for Cryptosporidium detection in patients with diarrhea (Odds ratio 2.5, CI=2.3-2.8). Our results showed that the Participants with diarrhea are more likely to be infected with Cryptosporidium protozoan parasites (52.1%) than 13.5% (104 out of 770 without diarrhea) infected with C. parvum. Co-infections with other intestinal parasites were found in 800 out of the 1340 positive isolates. The parasites identified in this study were Entamoeba histolytica\dyspar cyst (48.50%), Giardia lamblia cyst (37.3%), Hymenolepis nana (26.11%), Ascaris lumbricoides, (6.7%), respectively. No significant difference between cryptosporidiosis infectious and other intestinal parasites.
Conclusion: The Prevalence among participants was 30%. Additionally, there is an association between Cryptosporidium and diarrhea among participants was very high (52.1%). Infected patients with Cryptosporidium had diarrhea and were at risk 2.5 times more likely to patients have diarrhea than non-infected.
Keywords: Diarrhea; Cryptosporidium spp; mZN stain; Libya; Oocyst
Infections of intestinal parasites are still a serious public health problem globally [1]. Cryptosporidium is a unicellular parasite contaminated food and water are most commonly responsible for transmission. In the first of 1907 discovered by Tyzzer [1], and described as a protozoan parasite [2,3]. About 20 Cryptosporidium species were detected, two species among them reported in humans [4]. Cryptosporidium (hominis and parvum). Cryptzptosporidiosis is a pathological condition caused by a parasitic disease that can be life-threatening for children and patients immunocompromised. In industrialized countries the parasitic protozoa Cryptosporidium spp. attracts notice with large epidemics while in many developing countries being undiagnosed and neglected [5,6] Cryptosporidium spp are protozoan parasites that infect a wide range of humans and animals globally [7]. Cryptosporidium is a protozoan parasite that is associated with gastrointestinal diseases in all classes of vertebrates [8]. Cryptosporidium is one of the highest prevalences of childhood diarrhea in poor countries. Initially, Cryptosporidium spp. was reported by Tyzzer as infective in mice [1] and then was pushed to the background until the first human case was noted in 1976 [9,10]. In developing countries, the parasite was gradually associated with malnutrition and death caused by diarrhea in children.
In the 1980s, Cryptosporidium was recognized as an important cause of persistent diarrhea in immunocompromised patients (AIDS) [11,12]. Many factors may promote the spreading of this parasite in the human population, particularly in young children. The spreading of these parasites occurs through the fecal-oral route and by the consumption of contaminated water or food [13]. Cryptosporidiosis usually results in watery diarrhea [14], and additional signs include low temperature, nausea, intestinal pain and vomiting and occasionally a headache, anorexia, malaise, faintness and myalgia [7]. Aim of the study: The present study was undertaken to determine the community prevalence rate of Cryptosporidium infection and related risk factors among the general population and assess the importance of Cryptosporidium in the causation of acute diarrhea in patients of all age groups who attending to Al Akeed laboratory, Benghazi, Libya.
Study design and subjects: A retrospective study was conducted from March 2019 to February 2020, with a total of 1340 fecal samples from diarrhea, bloody diarrhea, abdominal pain, parasitic infections, etc.) The information was collected from the parasitology department patients who attended Al Akeed Medical laboratory in Benghazi, city. These patients attending suffer from different symptoms (watered registration notes. Fecal carriage of C. parvum oocysts was investigated in 1340 stool specimens collected from patients >1 year to 75 years. Specimen collection and Staining Lugol’s Iodine modified Ziehl Neelsen; (mZN stain) and microscopy, Routine stool examination applied to all specimens was taken from a sterile container. Microscopic examination of the stool specimens was done by a screening of the stool specimen, wet mount preparation along with 1% Lugol’s Iodine was used to detect various parasites.
There are many techniques used for the identification of C. parvum oocysts in feces. On the other hand, modified ZN staining is effective, inexpensive, non-invasive and easy to perform lab tests which showed the presence of Cryptosporidium oocysts. The oocysts of Cryptosporidium spp had spherical morphology of organisms, size, and blurred inner structure. The specimens collected show the signs and symptoms of diarrhea.
The dried smear was fixed with absolute methanol for 3-5 minutes. A Carbol-Fuchsine solution was added to the full smear slide for 15-20 minutes. The slide was washed gently with tap water using a dropper. After this, 4-6 drops of decolourizer acid alcohol were added to the smear, and the slide was washed off with clean water again. The counterstain methylene blue was added for 4-5 minutes and washed with water. The backside of the slide was rubbed, cleaned and put in the draining rack for 5 minutes to air dry the smear. The smear was examined microscopically, using the 40x and 100x (oil immersion lens) objectives and scanned thoroughly for parasite identification. The presence or absence of oocysts was recorded.
Statistical Analysis
A retrospective Statistical analysis was performed by using the Statistical Package of Social Sciences (SPSS) version 20, Pearson and chi-square tests were used to detect significant differences between various groups. A P-value less than 0.05 was considered statistically significant.
Prevalence of Cryptosporidiosis Parvum Among Patients
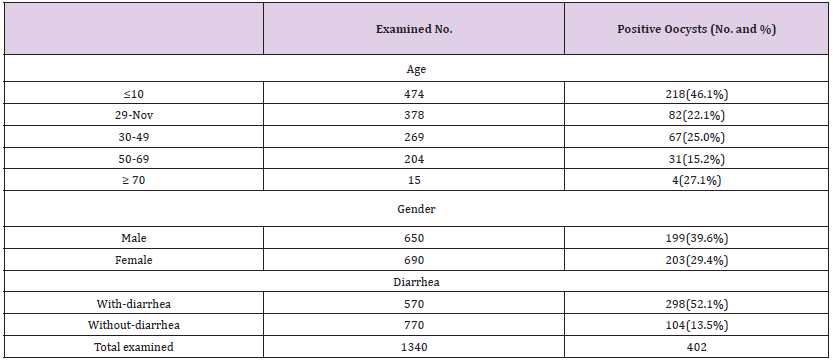
The participants were 1340 examined stool specimens. Applying modifying Ziehl Neelsen (mZN stain), to detect Cryptosporidium parvum oocyst, positive samples were 402(30%) with Cryptosporidium parvum oocysts. Among examined 570 Patients have diarrhea detect 298 (52.1%) suffering from infection with Cryptosporidium parvum but 770 without diarrhea and 104(13.5%) infected with C.parvum patients with diarrhea were more likely to have Cryptosporidium oocysts in their stool [Odds ratio of patients with diarrhea and infected with Cryptosporidium were 2.5 times more likely to patients have diarrhea and non-infected with Cryptosporidium oocysts(χ2 = 17.64, df=1, Odds ratio 2.5, CI=2.277- 2.870, P=0.05)]. Regarding the prevalence between males and female, the higher percentage were in men (39.6%) than in women (29.4%), while there was no significant difference (Sig; P=0.32). The results by the age group showed that the aged group ≤10 years has got the highest percentage (46.1 %), followed by the age group ≥70 years with 27.1% while the 50-69 years, age group showed the lowest percentage (15.2%) among the participants (Table1).
Table 1: Prevalence of Cryptosporidiosis parvum among patients according to age, gender and presence of diarrhea. Number (No.), Percentage (%).
Cryptosporidiosis and Diarrhea According to Month
Figure 1 Note: Cryptosporidium parvum(C. parvum) Figure 1: The graph provides the percentage of infected Cryptosporidium parvum patients with diarrhea and without diarrhea.
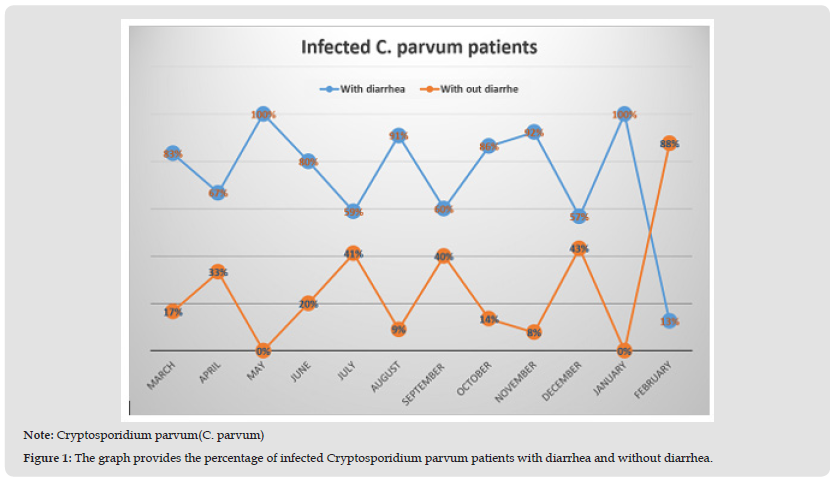
This table illustrates the prevalence by percentage (%) of studied participants’ monthly infection rate over two years. To begin firstly with examined specimens during this study, the highest rate of infection with C. parvum parasites seen during December was 60(78.9%) followed by October, March, November (67.8%), (66.7%), (66.3%) respectively, indicating a marked seasonal variation and occurrence of indigenous cases of cryptosporidiosis. In addition, the lowest rate percentage of infection was recorded on August 11(5.8%). More likely to have Cryptosporidium oocysts in their stool (P=0.05). Cryptosporidium parvum was detected. In addition, 30%(n=402) were infected with Cryptosporidium and monthly rate conditions were significant differences p<0.0014 found in the prevalence of cryptosporidiosis in participants when the months during the study period (Table 2 & Figure 1). Including 402 infected cases with Cryptosporidium, 298(74.1%) cases had diarrhea and 104(25.8%) without diarrhea. Obviously, in January/2019 and May/2020, all cases were infected associated diarrhea, however, in November and August were (92% and 90%), despite infected without diarrhea (7% and 10%), respectively, furthermore the lowest percentage of crypto infection recorded in February (12.5%). While the highest rate of crypto infection among cases without diarrhea was in February (87.5%) (Figure 2).
Table 2: Prevalence of Cryptosporidiosis among patients according to month and presence of diarrhea and without diarrhea.
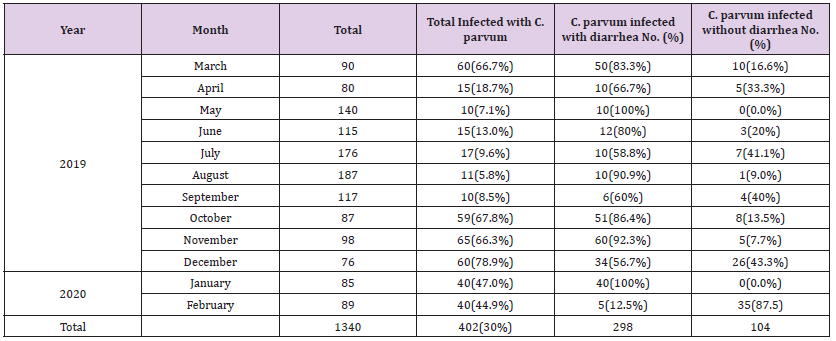
Note: Cryptosporidium parvum(C. parvum), Number(No.), Percentage(%).
Figure 2 The chart shows the percentage of infected patients with intestinal parasites. Note: Cryptosporidium parvum (C. parvum), Trichuris trichiura (T. trichiura), Blastocystis hominis (B. hominis), Endolimax nana cyst (E. nana cyst), Ascaris lumbricoides (A. lumbricoides), Hymenolepis nana (H. nana), Enterobius vermicularis (E. vermicularis), Giardia lamblia (G. lamblia), Entamoeba histolytica\ dyspar (E. histolytica\ dyspar).
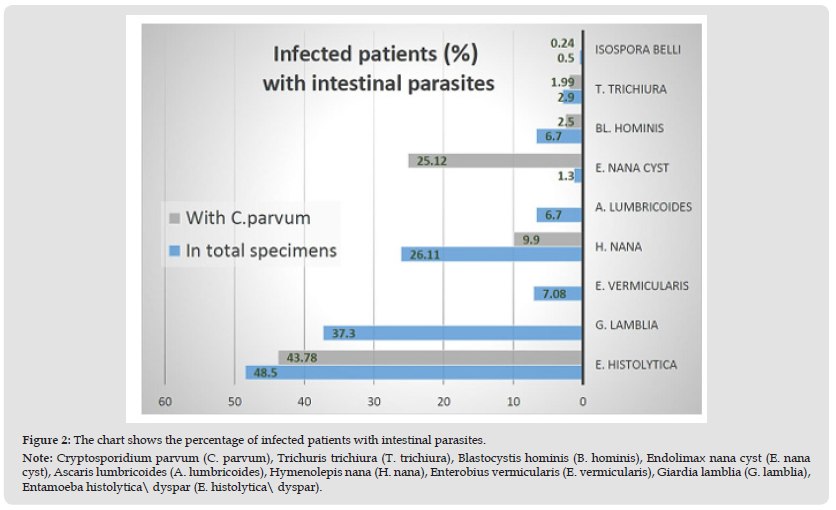
Specifically, the following intestinal parasites were highest prevalent in subjects Entamoeba histolytica\dyspar 650(48.5%) from 1340 total examined samples, among those infected with Cryptosporidium parvum oocyst were (43.78%). The next highest prevalent was Giardia lamblia (37.3%). However the lower presence of Hymenolepis nana 350(26.11%), Endolimax nana 17(1.3%), Blastocystis hominis 89(6.7%), Trichuris trichiura 39(2.9%), also low through C.parvum 40(9.9%), 101(25.12%), 10(2.5%), 8(1.99%), respectively. Nevertheless, Enterobius vermicularis 95(7.08%), and Ascaris lumbricoides, 89(6.7%) had no association with C. parvum plus Giardia lamblia. The lowest parasite was Isospora belli 7(0.5%) also with association C.parvium 6(0.24%). Although the presence of C.parvium with intestinal parasites Data analysis revealed that there was no significantly different (Pv>0.05).
Since cryptosporidiosis is under-famed public health, in the present study, out of 1340 fecal specimens collected from studied participants and examined by Modified Ziehl Neelsen (mZN stain), Cryptosporidium oocysts were detected in 420 (30%). Our finding was consistent with that of Abdulsadah, et al. [15] in Iraq 33.83% [15] and slightly different from Yemen 43.4% [16] but our prevalence was much higher than the (10.0%, 17.3%) reported in Sudan by Tamomh [17] and Kuwaiti by [18]. We could not explain the difference in the prevalence of Cryptosporidium infection but in our study, the prevalence in females and males were (29.4% and 39.6%, respectively), both sexes showed almost the same level of susceptibility to infection and results showed no significant evidence, differences were observed between infected men and women consistent with the results of [18] Adamu, et al. [19] in Ethiopia, who reported that Cryptosporidium positive people were 50.6% in men and 49.4% in women, similarly [19]. Some reports have found that no association of Cryptosporidiosis with a sexual group [20]. In addition, other authors found that females are more often infected than males [21]. In our study the Cryptosprdium prevalence rates were decreased with an increase in age among examined participants, current research indicated that children aged <10 years were more likely to be infected with Cryptosporidium oocysts (46.1%).
This is supported by results from several other studies in developing countries [22,23], while the lowest infection rate was observed in 15.2% of examined aged 50-69 years. This agreement with other studies conducted in Kuwait, Egypt and Korea [18,23- 25]. Children are more exposed to infections by Cryptosporidium spp due to a lack the knowledge about good food and water, maybe eating without washing their hands, playing in soil, sewage and water, exposed to more fecal-oral contact, or through contaminated food or water, or this attributed difference may be explained to their weak immune responses [25,26]. One of the enteric coccidian parasites is Cryptosporidium parvum that has become a cause of concern as an important agent of diarrhea and it causes watery diarrhea among both children and adults. In our study, cryptosporidiosis was a risk factor related to patients with diarrhea 2.5 times and these results finding agree with previous studies [17,20]. The prevalence of Cryptosporidium among participants with diarrhea had been higher in the participants without diarrhea in many studies. In our study, we found that (52.1%) of the studied participants with diarrhea had C.parvum infection, higher than participants without diarrhea these similar to that reported earlier elsewhere [27,28].
This study showed the association of Cryptosporidium infection with rainy months conditions, and also recorded a high significant difference between prevalence (%) of Cryptosporidium infection and monthly rate conditions in December (78.9%) infected with Cryptosporidium followed by October, March, November, 67.8%, 66.7%, 66.3% respectively, and the lower prevalence (%) of Cryptosporidium was in August (5.8%) followed by May, September, July, June, April (7.1%), (8.5%), (9.6%), (13.3%) and (18.7%) respectively. This may be explained by during these months a rainy to heavy rainfall could help the transmission of Cryptosporidium, However, in most studies, the highest numbers of cases have been detected during the rainy season and these results finding are in agreement with previous studies [29,30] (Clavel, et al. [29,30]).
It can be concluded that a risk factor with diarrhea associated with Cryptosporidium infection clear, C. parvum can induce causes of diarrhea However, more studies have to be done to elucidate this association and to further understand cryptosporidiosis pathogenesis. Also, in the future, we need to analyze water sources, because water is one of the most important sources of Cryptosporidium infection.
Cryptosporidium parvum infection was prevalent among Inhabitants patients of Benghazi very clear in this study, especially among children, the gender has no differences. Additionally, the current study has documented diarrhea as a risk factor associated with Cryptosporidium infection.
The authors thank the all-staff members of laboratory- Al Akeed laboratory, Benghazi, Libya.


