Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Martin Daniš M.D.1* and Miroslav Mako M.D.1,2*, Jozef Haring M.D.1,3,Georgi Krastev M.D. PhD.1,2
Received: January 01, 2023; Published: January 25, 2023
*Corresponding author: Martin Danis and Miroslav Mako, Faculty Hospital of Trnava, department of Neurology, Slovakia
DOI: 10.26717/BJSTR.2023.48.007626
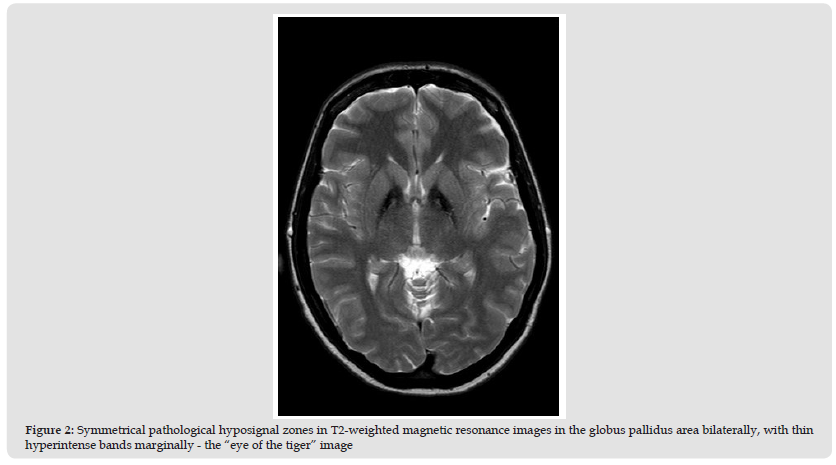
In this paper we present a case of a 39-year-old patient, who presented with a 4 year history of gradually worsening symptoms of uncontrolled movements of the right limbs, walking difficulties and unsteadiness pulling her to the right. During clinical examination we observed choreoathetoid movements and dystonic posture of the head and the limbs on the right side of the body, rigidity of the right limbs, postural and rest tremor of the hands, positive Romberg’s and Babinski sign on the right. On brain MRI we could see pathological hypodensity zones symmetrically in the region of globus pallidus bilaterally - typical for the “eye of the tiger” sign that corresponded to a neurodegenerative metabolic disease with brain iron accumulation (NBIA). On the molecular genetic examination of the PANK2 gene we identified a pathogenic variant c.1583C> T (p.Thr528Met) in the PANK2 gene in the homozygous line. According to these results we confirmed a diagnosis of pantothenate kinase associated neurodegeneration (PKAN).
Keywords: NBIA (Neurodegeneration with Brain Iron Accumulation); PKAN (Pantothenate Kinase-Associated Neurodegeneration); Extrapyramidal Syndrome; Dystonia
An image of increased signal intensity on T2-weighted images in the central area of the globus pallidus (caused by necrosis and edema) surrounded by a zone of reduced signal intensity (representing iron deposits) on brain magnetic resonance is called eye of tiger sign. Most often, this picture occurs in diseases associated with neurodegeneration with iron accumulation (Hayflick, et al. [1]). This group of genetically determined diseases is characterized by an increased accumulation of iron in the basal ganglia with a variable clinical picture dominated by a combination of extrapyramidal symptoms with deterioration of cognitive functions (Hogarth [2]).
A 39-year-old female patient with a negative family history, mental retardation caused by perinatal asphyxia, a trained seamstress, admitted to the neurological department for a history of about 4 years of gradually developing difficulties in terms of uncontrollable movements of the right limbs, a tendency to instability to the right and unsteady walking. The neurological examination objectified choreoathetoid dyskinesias of the right limbs with dystonic posture of the head and limbs to the right (Figure 1), increased muscle tone in the sense of rigidity, postural and rest tremor of the hands, positivity of Romberg’s and Babinski’s signs on the right (video). Laboratory parameters showed only a borderline increase in the serum iron level, other samples, including withdrawal factors and parameters of the thyroid gland, were normal. Magnetic resonance imaging of the brain in T2-weighted images showed pathological hyposignal zones symmetrically in the globus pallidus area bilaterally, with thin hyperintense bands marginally – a typical «eye of the tiger» sign (Figure 2).
Figure 2 Symmetrical pathological hyposignal zones in T2-weighted magnetic resonance images in the globus pallidus area bilaterally, with thin hyperintense bands marginally - the “eye of the tiger” image
The magnetic resonance imaging was consistent with neurodegenerative metabolic disease with iron accumulation. Subsequently, on the basis of relevant examinations, Wilson’s disease was ruled out. As part of the differential diagnosis, EEG examination showed normal brain activity without specific pathological activity. Ophthalmologic examination was normal. EMG examination for polyneuropathy was also negative. Symptomatic therapy with benzodiazepines (10 mg per day), baclofen (20 mg per day) and levodopa (400 mg per day) was started, during which the twisting movements, tremor and dystonia subsided. Tay-Sachs Morbus, Sandhoff Morbus, b-galactosidase deficiency and Huntington’s disease were excluded by genetic examination. By molecular genetic examination of the PANK2 gene, the pathological variant c.1583CT (p.Thr528Met) in the PANK2 gene was identified in a homozygous state. This finding in patients corresponded to neurodegeneration associated with pantothenate kinase disorder (PKAN).
PKAN is the most common type of NBIA. It is an autosomal recessive hereditary disease with a prevalence of approximately 1-2: 1,000,000 linked to a mutation of the PANK2 (pantothenate kinase 2) gene. The PANK2 gene encodes the mitochondrial enzyme pantothenate kinase, which is a key regulatory enzyme in the biosynthesis of coenzyme A in mammalian cells. PKAN was first described by neuropathologists Julius Hallervorden and Hugo Spatz in 1922. Based on the clinical symptoms and their time of onset, the disease is divided into classic and atypical forms (Hayflick, et al. [1]). Classic is characterized by walking disorders, with frequent falls and manifests itself before the age of six. It is manifested by a combination of extrapyramidal (dystonia with dominant involvement of the lower limbs, chorea, parkinsonism) and pyramidal (spasticity, hyperreflexia, positive irritative pyramidal phenomena) symptoms, deterioration of cognitive functions, pigmentary retinopathy, and various oculomotor disorders. The development of the disease is relatively rapid, often with a complete loss of the ability to walk between 10 and 15 years of age. The atypical form is characterized by the onset of symptoms between the second and third decade of life and a heterogeneous clinical picture. The first symptoms are usually speech disorders (palilalia, dysarthria) and psychiatric syndromes (mood disorders, personality changes), motor disability is usually present only in later stages, typically as a combination of dystonia and parkinsonism (Hvízdošová, et al. [3]). In contrast to patients published in the past, where the primary symptoms were speech and mental disorders with the onset of clinical symptoms between the second and third decade of life (Poplawska-Domaszewicz, et al. [4]), the patient in our case report was dominated by extrapyramidal symptoms in combination with pyramidal, while the onset of symptoms occurred in the third decade of life.
The asymmetry of clinical symptoms that was present in the case of the presented patient rarely occurred in previously published patients (Ch. H. Lee, et al. [5]). In addition to the neurological examination with the finding of typical clinical symptoms, imaging examinations (MRI) and genetic examination are important in diagnosis. In the MRI image (in T2-weighted images) there is a typical finding of iron deposits in the globus pallidus and substantia nigra pars reticulata with the characteristic image of the «eye of the tiger sign» (Poplawska- Domaszewicz, et al. [4]), which were also present in the presented patient. Treatment of patients with PKAN is mostly symptomatic. Benzodiazepines are used to improve muscle contraction and relieve twisting movements. Oral trihexyphenidyl, clonazepam, baclofen, or a baclofen pump are used in dystonia therapy. The positive effect of benzodiazepines and baclofen was also demonstrated in this case. In some patients, as well as in the case of the mentioned patient, dopaminergic substances - levodopa, bromocriptine - can have a positive effect on dystonia. The application of botulinum toxin also plays an important role in the therapy of dystonia in patients with this disease. In case of failure of the conservative procedure, surgical intervention is important in the therapy of dystonia. The main surgical option is deep brain stimulation (Gregory, et al. [5]).
Based on an international study, bilateral deep brain stimulation of the globus pallidus internus had a positive effect on alleviating dystonia (Petrleničová, et al. [6]). In patients with severe dystonia, stereotactic pallidotomy and bilateral thalamotomy with subsequent partial relief of symptoms may be indicated. Iron chelates, especially deferiprone, which, according to a randomized study, slowed down the progression of the disease are also becoming a perspective for the future. (Klopstock et al., 2019). In patients with atypical PKAN who have preserved residual PANK enzyme activity, administration of excessive doses of pantothenate (vitamin B5) may be effective. Antioxidant therapy (coenzyme Q10, alpha-tocopherol, ascorbic acid, etc.) remains a formally untested option (Petrleničová, et al. [6]). Based on the clinical symptoms, MRI findings and the effect of the established therapy, we believed that the final diagnosis of the presented patient could be PKAN disease, which was finally confirmed on the basis of a genetic examination. The prognosis of patients with PKAN is variable and depends on the clinical course and its form (classic or atypical). In patients with the classic form, the disease has a gradual course in the sense of progression over several years, which leads to death in early childhood (Philip [7]). Some patients undergo slow progression and may continue to function until their third decade of life. The atypical form of PKAN is less aggressive than the classical form and therefore most individuals remain functional usually within 15 to 40 years from the onset of the first symptoms of the disease (Kurian and Hayflick [8]).
Neurodegeneration with iron accumulation represents a large heterogeneous group of rare genetically linked diseases that should be considered in the differential diagnostic process in diseases with extrapyramidal symptoms in combination with deterioration of cognitive functions. Despite the fact that there is currently no causal therapy available for any of these diseases, the possibilities of their symptomatic therapy are still expanding with ongoing clinical studies (Hvízdošová, et al. [3,9,10]).


