Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Atsushi Ochiai1,2*
Received: December 21, 2022; Published: January 11, 2023
*Corresponding author: Atsushi Ochiai, Department of Otolaryngology - Head and Neck Surgery, Kitasato University School of Medicine, 1-15-1 Kitasato, Minami-ku, Sagamihara, Kanagawa 252-0374, Japan
DOI: 10.26717/BJSTR.2023.48.007590
Objectives: Undiagnosed cases are not simply diagnosed as vertigo or dizziness in my clinic; instead, they are classified according to their symptoms, including the mode of attack occurrence, their recurrence, and relative association with a cochlear symptom. The most common of these symptoms are the “recurrent vertigo attacks without a cochlear sign.” Thus, it will be interesting to examine whether these “recurrent vertigo attacks without a cochlear sign” will lead to a definitive diagnosis or remain undiagnosed.
Methods: The subjects were classified into those having “recurrent vertigo attacks without a cochlear sign” and those with signs that could be observed for more than 1 year.
Results: Of the 46 patients with “recurrent vertigo attacks without a cochlear sign,” 36 patients (78.3%) remained with “recurrent vertigo attacks without a cochlear sign,” whereas 10 patients (21.7%) were diagnosed with a definitive diagnosis.
Conclusion: Studies concerning “recurrent vertigo attacks without a cochlear sign” revealed that 36 of 46 cases, constituting 78.3%, had remained in the same group of “recurrent vertigo attacks without a cochlear sign” after more than 1 year. Therefore, it might be necessary to investigate how to properly treat and care for patients with “recurrent vertigo attacks without a cochlear sign” as 1 unit of vertiginous disease.
Keywords: Significance of Symptomatic Classification; Undiagnosed Cases; Vertigo; Dizziness; Recurrent Vertigo Attacks Without a Cochlear Sign
Abbreviations: BPPV: Benign Paroxysmal Positional Vertigo; SDS: Self-Rating Depression Scale
Treatment of patients with vertigo or dizziness requires a broad perspective, as it involves various departments, including otorhinolaryngology, internal medicine, neurosurgery, orthopedics, ophthalmology, obstetrics and gynecology, and psychiatry. For example, otorhinolaryngology involves the treatment of system diseases, dizziness, and balance disorders caused by central nervous system disorders in addition to diseases of the inner ear. Furthermore, many institutions have established specialized vertigo or dizziness outpatient clinics. This is due to the development of equilibrium function testing, which can detect equilibrium disorders in the differential diagnosis and treatment of vertigo or dizziness. In other words, neuro-otological tests, particularly equilibrium function tests, in conjunction with auditory tests, can help clarify lesions in the inner ear and the eighth cranial nerve and the brainstem and cerebellum. However, more than 40% of cases still fail to achieve a diagnosis [1-3], this only demonstrates the difficulty of diagnosing vertigo or dizziness. Furthermore, many patients do not return to the hospital once their vertigo or dizziness has remitted, which may be partially due to insufficient follow-up. Undiagnosed cases are not simply classified as vertigo or dizziness in my clinic; instead, they are classified according to their symptoms, including the mode of attack occurrence, their recurrence, and relative association with a cochlear symptom [4-6]. The most common of these symptoms are the “recurrent vertigo attacks without a cochlear sign.” Thus, it will be interesting to examine whether these “recurrent vertigo attacks without a cochlear sign” will lead to a definitive diagnosis or remain undiagnosed. However, there is yet no report that examines the course of these “recurrent vertigo attacks without a cochlear sign,” as the Japanese Society for Equilibrium Research has not provided its official definition. Therefore, this study aimed at reporting the course of this symptom.
The study subjects included 970 patients who visited Hongo Neurosurgery Clinic, which is a specialized vertigo or dizziness outpatient clinic, for the first time during a 3-year study period between April 2018 and March 2021, of whom, cases that were not able to have a definitive diagnosis were classified into 6 categories (Table 1), and the 46 patients classified into “recurrent vertigo attacks without a cochlear sign”, the most common of these, and who could be observed for more than 1 year were analyzed in detail. In addition to “recurrent vertigo attacks without a cochlear sign,” there are other categories, which include “a single vertigo attack without a cochlear sign,” “a single vertigo attack associated with a cochlear sign,” “recurrent vertigo attacks associated with a cochlear sign,” “provocative vertigo,” and “continuous dizzy state.” In addition, their definitions, including that of “recurrent vertigo attacks without a cochlear sign,” are shown in (Table 1). All procedures were in accordance with the Helsinki declaration and all patients provided written informed consent for review of their records for research purposes.
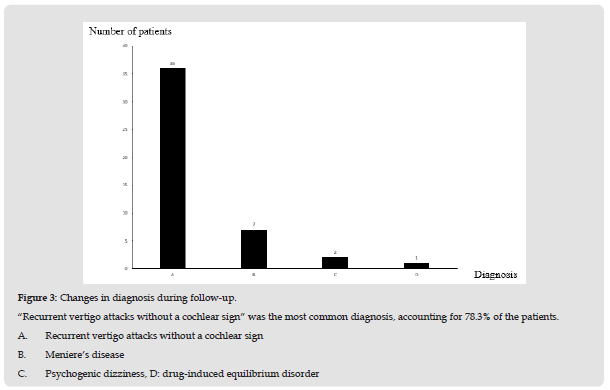
In total, 970 patients were recorded during the 3-year study period. Among these, 260 patients were undiagnosed, which includes 108 (41.5%) with “recurrent vertigo attacks without a cochlear sign,” 33 (12.7%) with “recurrent vertigo attacks associated with a cochlear sign,” 15 (5.8%) with “a single vertigo attack without a cochlear sign,” 10 (3.9%) with “a single vertigo attack associated with a cochlear sign,” 90 (34.6%) with “provocative vertigo,” and 4 (1.5%) with “continuous dizzy state” (Figure 1). Among the 108 patients with “recurrent vertigo attacks without a cochlear sign,” 46 were able to be observed for more than 1 year, including 14 males and 32 females. The age distribution was 23-81 years, with a mean age of 61.4 years (Figure 2). Thirty-six patients (78.3%) remained with “recurrent vertigo attacks without a cochlear sign” during follow-up. In contrast, 10 patients (21.7%) were able to have a definitive diagnosis, which included 7 patients with Meniere’s disease (15.2%), 2 patients with psychogenic dizziness (4.3%), and one with drug-induced equilibrium disorder (2.2%) (Figure 3, Table 2). Below is a case study and summary of the case.
Figure 1 Breakdown of undiagnosed cases. “Recurrent vertigo attacks without a cochlear sign” was the most common, accounting for 41.5% of cases. A. Recurrent vertigo attacks without a cochlear sign B. provocative vertigo C. Recurrent vertigo attacks associated with a cochlear sign D. A single vertigo attack without a cochlear sign E. A single vertigo attack associated with a cochlear sign F. Continuous dizzy state
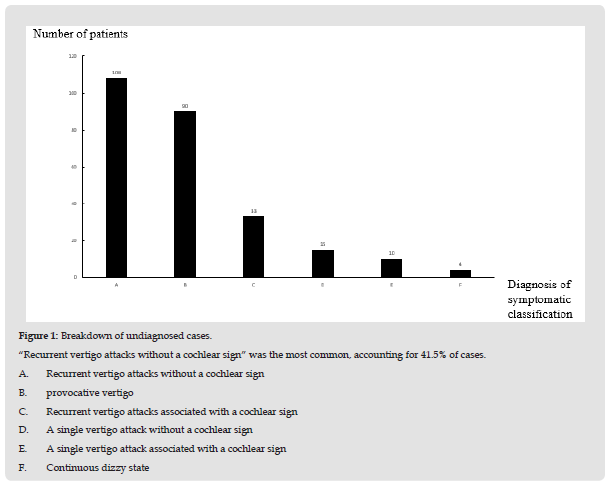
Figure 2 Gender and age distribution of the 108 patients with “recurrent vertigo attacks without a cochlear sign.” Most of the patients were female, with a peak being in their 60s.

Figure 3 Changes in diagnosis during follow-up. “Recurrent vertigo attacks without a cochlear sign” was the most common diagnosis, accounting for 78.3% of the patients. A. Recurrent vertigo attacks without a cochlear sign B. Meniere’s disease C. Psychogenic dizziness, D: drug-induced equilibrium disorder
A Case of Meniere’s Disease
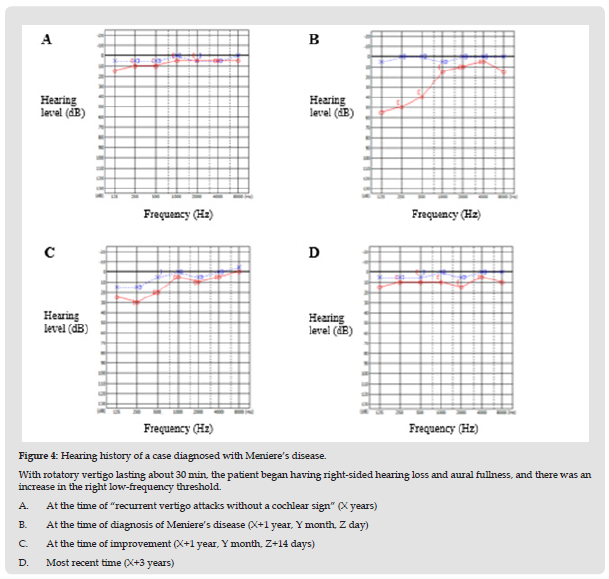
A 48-year-old man came to my clinic, first, because of recurrent episodes of rotatory vertigo without a cochlear sign, which lasted 5-10 min without any specific trigger. At the time of his first visit, he had no body equilibrium disorder or eye movement disorder, and his hearing was normal. Additionally, the patient was not aware of any stress. However, the duration of rotatory vertigo gradually became longer, extending for about 30 min. Right-sided hearing loss and aural fullness also appeared. The patient was diagnosed as having right-sided Meniere’s disease and was further treated with medication, although still under observation. The hearing history is shown in (Figure 4).
Figure 4 Hearing history of a case diagnosed with Meniere’s disease. With rotatory vertigo lasting about 30 min, the patient began having right-sided hearing loss and aural fullness, and there was an increase in the right low-frequency threshold. A. At the time of “recurrent vertigo attacks without a cochlear sign” (X years) B. At the time of diagnosis of Meniere’s disease (X+1 year, Y month, Z day) C. At the time of improvement (X+1 year, Y month, Z+14 days) D. Most recent time (X+3 years)
Summary of Psychogenic Dizziness Cases
Both patients (a 24-year-old woman and a 31-year-old woman) first came to my clinic complaining of recurrent floating dizziness. At the initial examination, no body balance disorder or eye movement disorder was observed. Also, their hearing was observed to be normal. On the Self-rating depression scale (SDS), one patient was normal (37 points), and the other patient was found to be neurotic (50 points). During the follow-up, the complaints gradually became stronger. However, considering that there were still no abnormalities in the examination findings, SDS was performed again despite a discrepancy between the complaints and findings. Additionally, the patients were referred to the psychiatry department of another hospital on suspicion of psychogenic dizziness as the SDS score noted to increase (from 37 to 49 and 50 to 60). Subsequently, subjective symptoms improved after treatment at the same hospital.
Summary of a Case of Drug-Induced Equilibrium Disorder
A 36-year-old woman first came to my clinic complaining of recurrent floating dizziness without any specific trigger. At the time of her first visit, she had no body balance disorder or eye movement disorder, and her hearing was normal. However, during follow-up, findings showed that her medication dosage (sertraline hydrochloride) had increased from 25 to 50 mg, which she had not reported before during her first visit. Additionally, information was provided to the same psychosomatic medicine department, which subsequently reduced the medication dose (from 50 to 25 mg). This resulted in an improvement in subjective symptoms. Among the undiagnosed cases, except for “recurrent vertigo attacks without a cochlear sign,” 19 patients with “recurrent vertigo attacks associated with a cochlear sign,” 8 patients with “a single vertigo attack without a cochlear sign,” 4 patients with “a single vertigo attack associated with a cochlear sign,” 36 patients with “provocative vertigo,” and 4 patients with “continuous dizzy state” were examined for more than 1 year.
The course of the respective diagnoses indicates that among the 19 patients with “recurrent vertigo attacks associated with a cochlear sign,” 15 remained with “recurrent vertigo attacks associated with a cochlear sign” (78.9%), whereas 4 were confirmed to have Meniere’s disease (21.1%). Findings also showed that among the 8 patients with “a single vertigo attack without a cochlear sign,” 5 remained with “a single vertigo attack without a cochlear sign” (62.5%). In contrast, three had recurrent vertigo without a cochlear sign that changed to “recurrent vertigo attacks without a cochlear sign” (37.5%). Furthermore, among the 4 patients with “a single attack of vertigo associated with a cochlear sign,” 3 had recurrent vertigo associated with a cochlear sign and later changed to “recurrent vertigo attacks associated with a cochlear sign” (75.0%), whereas one had a definitive diagnosis of Meniere’s disease (25.0%). Additionally, among the 36 patients with “provocative vertigo,” 32 remained with “provocative vertigo” (88.9%), whereas 4 patients had benign paroxysmal positional nystagmus, thereby leading to the definitive diagnosis of benign paroxysmal positional vertigo (BPPV) (11.1%). Furthermore, all four patients in a “continuous dizzy state” remained (100%) in a “continuous dizzy state” (Table 2).
Correct diagnosis is essential for appropriate treatment, not only for vertigo or dizziness but for all diseases. Arriving at a diagnosis is not very difficult, provided the typical symptoms and findings are present. However, in cases when they are not, treatment may be difficult. Additionally, when a definitive diagnosis cannot be made, notwithstanding various tests and careful followup, the diagnosis of vertigo or dizziness can be undertaken for the time being. Murofushi [7] stated that about 30% of cases do not lead to a definitive diagnosis, which corroborated the findings from my clinic recorded at 26.8% (260 of 970 patients). According to Murofushi [7], the cases that do not lead to a definitive diagnosis are either such that involve (1) no abnormality to begin with, (2) an abnormality but cannot be detected by the current level of medicine, or (3) an existing abnormality at the time of the attack but had already normalized by the time of examination. Furthermore, reports indicate that abnormalities in balance function tests decrease with time from the onset of vertigo [8]. Therefore, in my clinic, patients are classified according to their symptoms rather than vertigo or dizziness to explain this possibility and alert patients to their course. However, none that this symptomatic classification is original and unofficially defined by the Japanese Society for Equilibrium Research.
In total, 36 of 46 patients (78.3%) remained in “recurrent vertigo attacks without a cochlear sign” and reflected no abnormal findings during follow-up. As mentioned above, there are no reports on the course of “recurrent vertigo attacks without a cochlear sign.” Also, the course of so-called vertigo or dizziness remains undefined in a high percentage of the reported cases (70%-90%). This may be an indication of the difficulty of diagnosing vertigo or dizziness. Additionally, many patients do not return to the hospital after the vertigo or dizziness has gone into remission. Consequently, insufficient follow-up may be a factor. Moreover, a balance function test may not reveal any obvious abnormalities when a patient presents with vertigo or dizziness. Here explaining to the patient that «it is normal» or «there is nothing wrong» may cause the patient to become dissatisfied or distrustful of the physician. According to Takeda [9], in this scenario, since the patient is anxious about the cause of his or her vertigo or dizziness, such explanations may lead to doctor shopping. Alternatively, there are many patients whose symptoms do not improve and whose anxiety is not resolved. Therefore, these patients stopped coming to the hospital. Among the 108 patients classified as having repetitive balance disorder, about 46 (42.6%) were seen regularly for follow-up and met the criteria for inclusion. This consisted of less than half of the sample population. However, 10 of 46 patients (21.7%) were diagnosed during the follow-up. The patient presenting with Meniere’s disease reflected a prolonged duration of vertigo. Also, subjective cochlear symptoms began to appear. Additionally, an audiological examination revealed a lowtone sensorineural hearing loss, thereby leading to the diagnosis of Meniere’s disease, which improved with appropriate treatment. However, since the previous vertigo duration was not as prolonged as Meniere’s disease, vestibular Meniere’s disease could not be diagnosed. Hence, the patient was categorized as having “recurrent vertigo attacks without a cochlear sign.” Consequently, it is difficult to determine whether the recurrent vertigo was a precursor of Meniere’s disease or whether it was completely unrelated.
For confirmed cases of psychogenic dizziness, the subjective symptoms did not improve, which is typical of cases involving patients with vertigo or dizziness. This case further leads to depression and a vicious circle of worsening subjective symptoms. Additionally, the patients were referred to the Department of Psychiatry, which specializes in treating depressive disorders. Subsequently, their subjective symptoms improved. Meanwhile, a case was also confirmed to be a definitive diagnosis of druginduced equilibrium disorder; such definitive diagnosis would have been achieved sooner if a more detailed interview during the initial examination was done. This observation substantiates the thoughts of a famous neurologist who once said, «History is everything.» Hence, the need that I should not cut corners in taking the patient’s history was reinforced, notwithstanding the busyness in the outpatient clinic. Eventually, I provided information to the psychosomatic medicine department. The subjective symptoms improved over time by adjusting the oral medication. Given the above case, a definitive diagnosis may be made during follow-up, and appropriate treatment may relieve the suffering of vertigo or dizziness. Therefore, it is important to monitor the patient carefully and not terminate the treatment unilaterally when abnormality is not detected. Additionally, although I focused on “recurrent vertigo attacks without a cochlear sign” in this study, there were cases in which the definitive diagnosis was confirmed in other undiagnosed cases. Furthermore, in the case of BPPV, otolith replacement therapy resulted in the disappearance of vertigo, thereby suggesting that the same observation is true for cases other than “recurrent vertigo attacks without a cochlear sign.”
In conclusion, my clinic’s ratio of undiagnosed vertiginous patients to already known vertiginous disease was approximately 26.8%. Those vertiginous patients lacking diagnoses were classified into six groups based on recurrence, cochlear signs, etc. Among them, the cases of “recurrent vertigo attacks without a cochlear sign” were followed up. It was revealed that 36 of 46 cases, which constituted about 78.3%, had after more than 1 year. Therefore, it might be necessary to investigate how to treat and care for patients with “recurrent vertigo attacks without a cochlear sign” as 1 unit of vertiginous disease.
Studies concerning “recurrent vertigo attacks without a cochlear sign” revealed that 36 of 46 cases, constituting 78.3%, had remained in the same group of “recurrent vertigo attacks without a cochlear sign” after more than 1 year. Therefore, it might be necessary to investigate how to properly treat and care for patients with “recurrent vertigo attacks without a cochlear sign” as 1 unit of vertiginous disease.
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
None.


