Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Maria Fernanda Romero Estrada1, Gilberto Cruz Arteaga3, Alma Italia Guerrero Martínez2*, Jose Antonio Zamudio Gonzalez11, Margarita López Quintanar4, Pamela Ivette Guerrero Calva5, Oscar Daniel Bazan Muñoz6, Macedonia Guadalupe Moreno Tovar3, Rebeca Cortés Chamorro9, Fabiola Samara Sánchez Camacho10, Dennice Cebreros Santiago3, Beatriz Cruz Arteaga9, Gloria Garnica Resendiz3, Monica Adriana Pineda Gutierrez3, Daniela Abigail Hernandez Camarillo10, Olivia Guadalupe Villanueva Martinez3, Mariana Irais Guzman Carrera8, Arturo Andrade Sanchez7, Linet Nava Ramirez3, Jorge Ramón Moran Rubio3, Emilio Ramirez Medina3, Claudia Moreno Garcia3, Elsa Susana Nava Aguilar3, Ivette Sanchez Vargas3, Yolanda Salazar Garduño3, Adriana Mejia Utrilla3, Augusto de Jesus Sanchez Arriola3, Karla Daniela Rosiles Fuentes10 and Martha Jael Calva Hernandez10 and Acho Federico Garcia Martínez12
Received: December 22, 2022; Published: January 11, 2023
*Corresponding author: Alma Italia Guerrero Martínez, Hematologist, General Hospital of Zone No. 48, Elpidio Cortez No. 300, Col. San Pedro Xalpa, CP 02750, Azcapotzalco Delegation, Mexico City
DOI: 10.26717/BJSTR.2023.48.007588
Cardiovascular disease is the most frequent cause of mortality in the world. Cardiovascular risk identifies a group of diseases such as atherosclerosis, which disorganizes the architecture and function of the vessels, variably reducing myocardial blood flow, identified as increased thickness of the carotid intima-media layer (cIMT), being an early marker of end-organ damage, which determines the risk of cardiovascular disease and can identify cardiovascular risk factors that require treatment. The objective was to evaluate the correlation between cardiovascular risk and cIMT in a population between 30 and 50 years of age with arterial hypertension in a U.M.F. 13 of the I.M.S.S. Material and methods: cross-sectional, analytical and prospective study in 219 patients with systemic arterial hypertension, determining cardiovascular risk with the Framingham scale as low, moderate or high cardiovascular risk. Using conventional ultrasound with a linear transducer (8 MHz) to identify right and left cIMT (D-L), analyzing the correlation between cardiovascular risk and cIMT-D/L and factors, using Pearson’s correlation test, model of linear regression, with SPSS V.21 and Stata V.14. Results: Of 219 patients, there was a significant correlation between cardiovascular risk and cIMT-R r = 0.260, p = 0.000; cIMT-L r = 0.222, p = 0.000; cholesterol r = 0.202, p = 0.001; LDL r = 0.187, p = 0.003; age r = 0.459, p = 0.000; PAS r = 0.469, p = 0.000; DBP r = 0.311, p = 0.000; MIB r = 0.139, p = 0.020. The R2 of the model was 0.411 with p = 0.000.
Keywords: Cardiovascular Risk; Carotid Intima Media Thickness; Atherosclerosis
Abbreviations: cIMT: Arotid Intima-Media Layer; WHO: World Health Organization; CVRF: Cardiovascular Risk Factor; HDL: High-Density Lipoprotein; LDL: Low-Density Lipoprotein; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; BP: Blood Pressure
According to the World Health Organization (WHO) cardiovascular diseases are responsible for 17 million deaths in the world, and it is estimated that by the year 2020, deaths from these diseases will increase from 15% to 20% [1]. Cardiovascular diseases were the cause of more than 4 million deaths in Europe in 2002. 1.9 million in the European Union, accounting for 43% of all deaths of any age in men and 55% in women [2]. Cardiovascular risk factor (CVRF) is a biological characteristic, habit or lifestyle that increases the probability of suffering or dying from cardiovascular disease, several institutions and scientific societies have based themselves on cohort studies and scales carried out by Framingham [3], which have been used to calculate the risk that a person has of presenting an acute myocardial infarction (AMI) or cerebrovascular event (CVD) in 10 years [4-6].There are non-modifiable (age, sex, genetic factors, family history) and modifiable (arterial hypertension, smoking, hypercholesterolemia, diabetes mellitus and overweight/ obesity) risk factors. Other CVRFs that are associated are highdensity lipoprotein cholesterol (HDL) low, triglycerides high, which represents a greater cardiovascular risk (CVR) and the possibility of developing chronic diseases [7,8]. Atherosclerosis is a generalized disease of the arterial wall. The carotid intima-media thickness (cIMT) has shown an association with cardiovascular risk factors and with the prevalence of cardiovascular disease [9,10].
The cIMT is defined sonographically as the distance between the lumen-intima and media-adventitia interface of the carotid wall [11]. There are variations in the measurement of the cIMT, in Spain the cIMT is reported more in men than in women with values of 0.71 vs. 0.67mm [12]. Positive correlations have been determined between arterial stiffness and cIMT of 0.39 to 0.45 [11]. A study in Cuba shows in patients with valve disease a statistically significant correlation between the intima-media thickness of the internal carotid artery (right) with the presence of coronary lesions of 0.67 [9]. In the Latino population, an increase in the cIMT is reported in 24% with four risk factors (arterial hypertension, diabetes mellitus, dyslipidemia and smoking) [13]. The objective was to evaluate the correlation between cardiovascular risk and cIMT in a population between 30 and 50 years of age with arterial hypertension in a U.M.F. 13 of the I.M.S.S.
Study Design
The present study is a non-experimental, cross-sectional, prospective, analytical.
Scope and Period of Study
This study was carried out in the Family Medicine Unit Number 13 of the Mexican Institute of Social Security in the period between March 2021 and March 2022 in 354 patients, with data obtained from an instrument (questionnaire), with items based on the Framinham scale, socioeconomic level and schooling were added. The following study will be carried out through carotid ultrasound in a group of men and women, aged between 30 and 50 years, with risk factors for presenting cardiovascular risk at an early age, total cholesterol, HDL, LDL will be requested, and triglycerides processed on an ARCHITECT i2000SR Immunoassay Analyzer Kit. A conventional Toshiba brand ultrasound with a linear transducer (8 MHZ) in gray scale was used, performed by a specialist in radiology and imaging, with the prior informed consent of the participant.
Participants
After accepting the informed consent, 354 patients were considered probabilistically, of which 219 were considered within the inclusion criteria: male and female patients between the ages of 30 and 50, with asymptomatic systemic arterial hypertension. 135 patients were excluded by criteria: Patients who do not reach the age of 30 to 50 years, patients who do not have a lipid profile.
Variables
All patients will be identified with cardiovascular risk, through the use of the Framingham scale 3, contemplating the items of: Age (space of years that have passed from one time to another, was categorized in our study into groups of 30-35 years, 36-40 years, 41-45 years and 46-50 years). Sex (biological, anatomical, physiological and chromosomal characteristics of the human species, especially related to procreation functions, was categorized as male or female). Systolic pressure (blood pressure is the force of the blood against the walls of the blood vessels. It is measured in millimeters of mercury (mm Hg). Blood pressure is normal if it is below 120/80 mm Hg. If the pressure is between 120 and 129, and diastolic pressure is less than 80, then there is high blood pressure. High blood pressure will be considered if systolic pressure is 130 or higher or a diastolic pressure of 80 or higher, which remains high over time. In our study, normal systolic blood pressure will be categorized with values between 100 and 120 mmHg) [14]. Total cholesterol (total amount of cholesterol in the blood. Includes both types: low-density lipoprotein (LDL) cholesterol and high-density lipoprotein (HDL) cholesterol, categorized as quantitatively expressed in milligrams/deciliter (mg/dl) [15,16]. Smoking (addiction to tobacco caused, mainly, by one of its active components: nicotine.
The action of this substance ends up conditioning the abuse of its consumption, the patients were categorized qualitatively with the number of cigarettes and qualitatively as if they smoked or not smokes) [17]. Hypertensive treatment (in particular, a group of various drugs used in medicine for the treatment of hypertension are known as antihypertensive agents, patients are categorized into patients taking one, two, three or more antihypertensives). Measurement of the thickness of the intima media (test is used to determine the extent of plaque accumulation on the walls of the arteries that supply blood to the head, an increase of 0.7mm is considered abnormal thickness), it was measured in the radiology and imaging service of UMF 13, the patient lying on a bed in a supine position, a cushion was placed on the shoulders for neck extension, a clear water-based gel is applied to the area being examined. This helps the transducer make secure contact with the body. It also helps eliminate air pockets between the transducer and skin that could block sound waves from entering. The radiologist places the transducer against the skin in several places, moving it over the area of interest. They could also tilt the angle of the sound beam to a different position to better see the area of interest [18,19].
The weight and height measurement technique of the GPCIMSS- 046-18 [20] for the diagnosis and treatment of exogenous overweight and obesity was taken and with the help of a nurse, the measurements were carried out correctly in an office with a clinical scale that has a capacity of 160 kg, measures height from 75 to 193 cm, with a minimum division of 100 g, base of 54 x 20 x 10.5 cm, stadiometer of 2 meters in height, zamak bar with matt chrome, finished in baked enamel paint, made of steel sheet, the weight capacity of the scale: 17 Kg, to calculate the body mass index. The lipid profile was taken, consisting of HDL cholesterol, LDL cholesterol and triglycerides, fasting for 8 hours. The sample was taken by pharmacobiologists and laboratory chemists from the UMF 13 service. The blood pressure of the patients was taken in a doctor’s office, the patient sitting at rest for 5 minutes, the arm resting at the level of the heart, without crossing the legs and feet resting on the floor. The sphygmomanometer is placed on the bare arm, leaving the antecubital fossa free, placing the lower edge of the cuff 2 to 3 cm above the crease of the elbow to be able to palpate the brachial artery, to later place the bell at that level of the heart. First establishing the systolic blood pressure (SBP) by palpating the brachial/radial artery, and while palpating pulse, rapidly inflate the cuff until it disappears, in order to determine the systolic pressure level by palpation.
The cuff will be deflated again, and the stethoscope cap will be placed over the brachial artery. The cuff will be rapidly inflated to 30- or 40-mm Hg above the palpatory level of systolic pressure to start auscultation of it. Deflating at a rate of 2 to 3 mm Hg/second. Using the first Korotkoff sound to identify the SBP number and the fifth sound (disappearance) for the diastolic blood pressure (DBP) number. Adjusting the auscultated figures to even numbers. If noises continue to be auscultated to a level very close to zero, then the fourth Korotkoff sound (quenching) should be taken to determine the PAD figure. Finally, it is necessary to carry out at least two measurements separated by at least one minute; if a difference in blood pressure (BP) is detected between the two, greater than 5 mmHg, a third measurement should be taken, it was categorized quantitatively through a scale based on the American Heart Association into normal, elevated, GI, GII and GIII and qualitatively with the figures of the shots that were made in the office, Ej. 110/80 mm Hg [21,22].
Ethical and Legal Aspects
Data was included in a registry approved by the ethics and health research committee.
Statistical Methods
To calculate the sample size, a probabilistic sampling was used for a finite population with N= 4437 patients with systemic arterial hypertension, with a standard deviation of 0.5, Zα of 1.96 for 95% and error limit of 0.05, with a sample obtained sample obtained is 354 patients. All statistical analyzes were performed using the statistical analysis program (SPSS 21). The correlation figures were used in the Stata V.14 program. Quantitative data are presented using the mean and standard deviation. Comparison of qualitative data (sex, age groups, education, comorbidities, exercise, smokers, antihypertensive treatment, socioeconomic level, systemic blood pressure), Pearson’s Chi-square test was used. Comparison of quantitative data (systolic blood pressure, diastolic blood pressure, cIMT-R, cIMT-L, triglycerides, cholesterol, low-density lipoproteins, high-density lipoproteins, body mass index, age in years) was made using the test test of equality of medians for K independent samples as a nonparametric test. Correlations between quantitative data were determined by the Pearson correlation coefficient. Partial correlation and multiple linear regression analysis to determine the independent predictor of cardiovascular risk. A value of p < 0.05 was interpreted as statistically significant.
In the present study of the 354 patients selected, 135 were excluded because they did not meet the inclusion criteria. Assigning 219 patients categorized according to cardiovascular risk, 33.8% (n=74) were found to be at low risk, 46.6% moderate (n=102), and 19.6% high (n=43). The male sex predominated in moderate and high; the age group from 46 to 50 years (75.5%, 95.3%, respectively); In the number of patients greater than the median, there was a predominance of moderate risk in systolic and diastolic blood pressure, TLML-RCA/LCA, trigliderides, cholesterol, low-density lipoproteins, and age, with a statistically significant difference p < 0.05. (Figure 1 & Table 1). The mean and standard deviation (±) of the patients with systemic arterial hypertension of the UMF 13 of the IMSS was 46 (5.7) years old, systolic blood pressure 131 (± 10.5) mmHg, diastolic blood pressure 84 (±8.1) mmHg, TIML-RCA 0.53 (± 0.12), TIML-LCA 0.54 (± 0.14), cardiovascular risk 14 (± 7.7), cholesterol 311 (± 113.1) mg/dl, body mass index 30.36 (± 5.19) kg/ m2) (Table 2). There was a significant positive correlation between cardiovascular risk and cholesterol (correlation coefficient (r) = 0.202, p = 0.001), low-density lipoproteins (r = 0.187, p=0.003), age (r = 0.459, p = 0.000), systolic blood pressure (r = 0.469, p = 0.000), diastolic blood pressure (r = 0.311, p = 0.000), TIML-RCA (r = 0.260, p = 0.000), TIML-LCA (r = 0.222, p = 0.000), Mass Index Body (r = 0.139, p = 0.020).
Figure 1 Flow of participants by cardiovascular risk in patients with systemic arterial hypertension at the U.M.F.No.13 of the I.M.S.S.
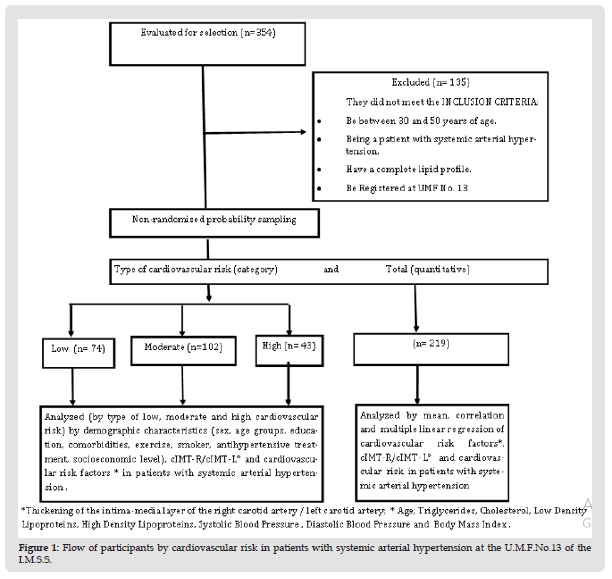
Figure 2 Correlation between Cardiovascular risk and the c IMT-L* in patients with hypertension from the I.M.S.S. r=0.222 p=0.000.
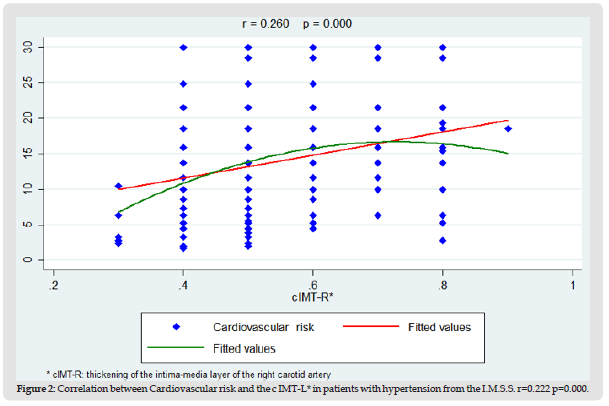
Figure 3 Correlation between Cardiovascular risk and Systolic Blood Risk in patients with hypertension from the I.M.S.S. r=0.469 p=0.000.
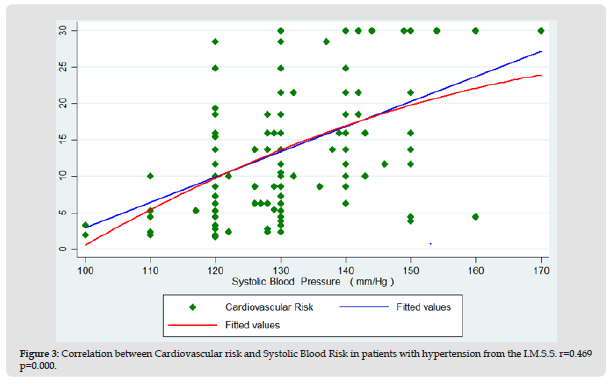
Figure 4 Correlation between Cardiovascular risk and age in patients with hypertension from the I.M.S.S. r=0.459 p=0.000.
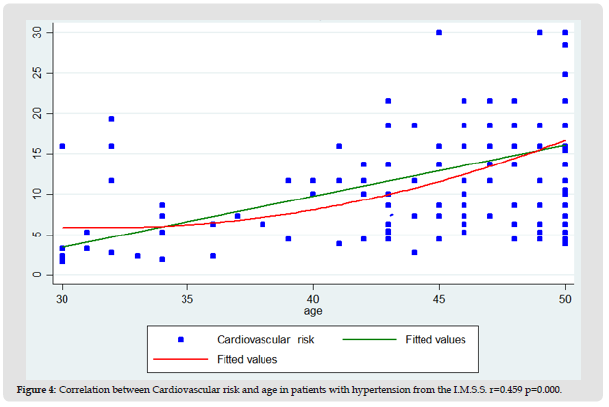
Table 1: Demographic characteristics in patients with systematics arterial hypertension by type of cardiovascular risk at the U.M.F.No.13 of the I.M.S.S.
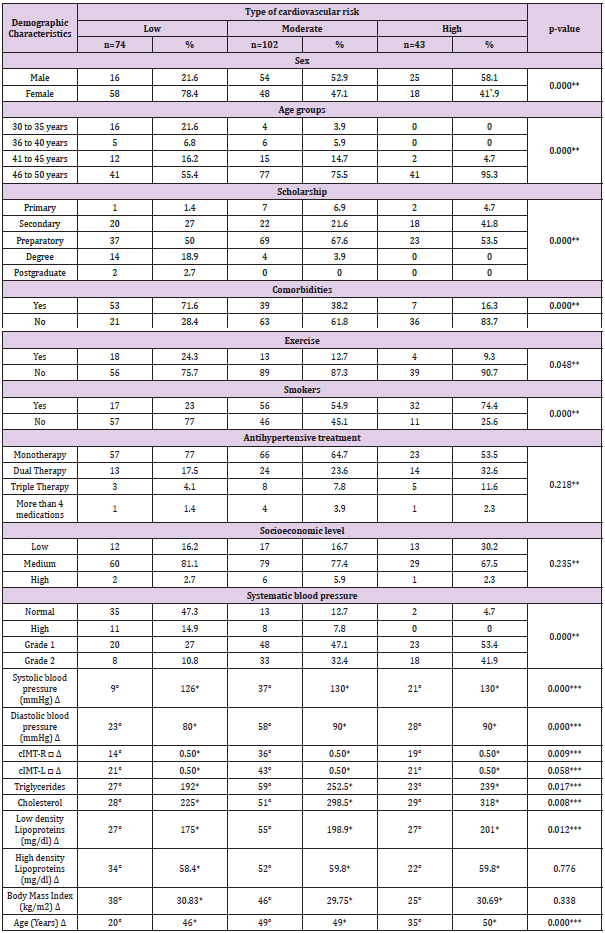
Note: number of patients greater than the median; *median; Δ mmHg milimeters of mercury, **p< 0.05pearsons Chi-square test; ***p < 0.05 Test of equality of medians for K samples; □cIMT-R/cIMT-L; Thickening of the intima-media layer of the right carotid artery/left carotid artery
Table 2: Mean of cardiovascular risk factors and cIMT-R/cIMT-L° in patients with systematic arterial hypertension at the U.M.F. 13of the IMSS.
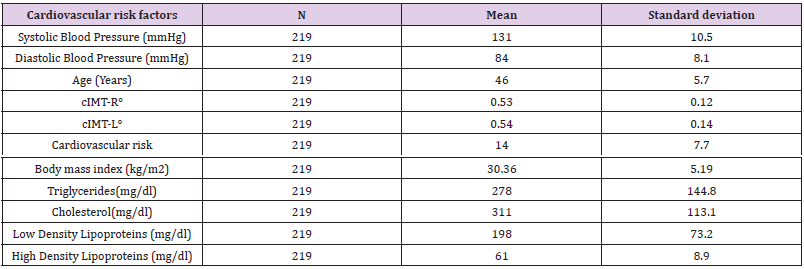
Note: °cIMT-R/cIMT-L: Thickening of the intima-media layer of the right carotid artery/left carotid artery.
Table 3: Correlation of the cIMT-R/cIMT-L°, factors with cardiovascular risk in patients with systematic arterial hypertension at the U.M.F.13 of the IMSS.
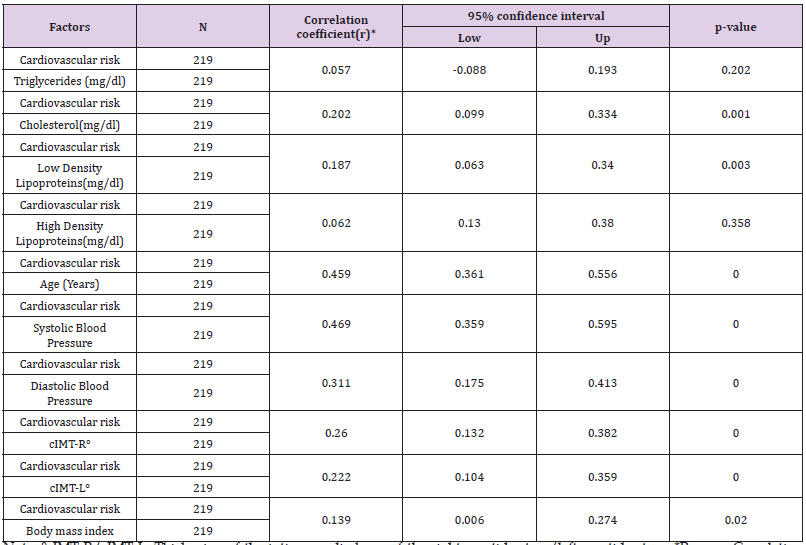
Note: °cIMT-R/cIMT-L: Thickening of the intima-media layer of the right carotid artery/left carotid artery; *Pearson Correlation Test; **p<0.05
Table 4: Multiple linear regression analysis to define the independent determinants of cardiovascular risk in patients with systematic arterial hypertension from the UMF 13 of the IMSS.
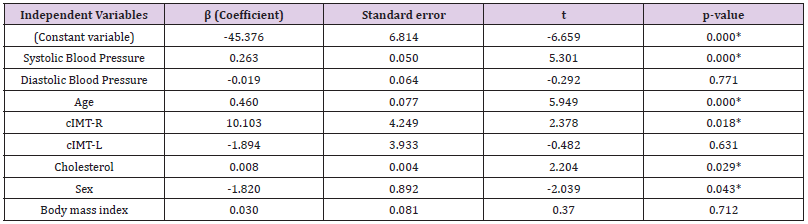
Note: *p<0.05; Abbreviations as in (Table 1),
There were no significant correlations between cardiovascular risk and high-density lipoproteins and triglycerides (Table 3 & Figures 1-4). A multiple linear regression analysis was used to define the independent determinants of cardiovascular risk in patients with systemic arterial hypertension at UMF 13 of the I.M.S.S. Systolic blood pressure, diastolic blood pressure, age, TIMLRCA, TIML-LCA, cholesterol, sex, and Body Mass Index scores were incorporated into the model as independent variables. The R2 of the model was 0.411 with p = 0.000. The linear regression model revealed that systolic blood pressure, age, TIML-RCA, cholesterol, and sex were independent predictors of cardiovascular risk. Regression coefficients for systolic blood pressure = 0.263 (p = 0.000), age = 0.460 (p = 0.000), TIML-RCA = 10.103 (p = 0.018), cholesterol = 0.008 (p = 0.029) and sex = -1.820 (p = 0.043) (Table 4).
The trend of the European populations in relation to cardiovascular risk and its factors differs considerably compared to our study, with 33.8 vs 63.1, 46.6 vs 21.8, 19.6 vs 5.7: low, high and moderate risk respectively. Observing the influence of highfat alimentary habits in our study population, with significant differences in levels of total cholesterol, triglycerides and cIMT [23]. In the Latin American population there is also a significantly greater difference in the trend of obesity and tobacco consumption [24]. In our study, 53% of the population presented some comorbidity, which according to previous studies, comorbidities represent 2.19 times more cardiovascular risk [25]. It is interesting to mention how an R2 of 41% was achieved in the linear regression model with the involvement of 5 independent variables (systolic blood pressure, cIMT-right, age, cholesterol and sex), statistically significant. Another study reports an R2 of 11% of the cIMT with 3 statistically significant variables such as sex, age and ambulatory pulse pressure in 24 hours [26]. Our study presented a significant difference by age and sex groups with the thickness of the intima media layer of the carotid artery and its cardiovascular risk.
However, we also consider obtaining the record of the cIMT thickness that diverges from other study cohorts, however the objective of the study did not involve evidence of reproducibility for this measurement, however as a secondary analysis we found a median value of 0.50 mm (both right and left of the cIMT, age 49 years for women and 45 years for men, predominantly males with moderate cardiovascular risk), different from the European and American cohort in the median of the cIMT for gender [19]. In relation to cardiovascular risk, in our study compared with the European population in men, there is 27.8% and 40% less high and moderate cardiovascular risk, respectively [27].
Of the 219 patients analyzed, despite finding significant differences in some of the cardiovascular risk factors and cIMT, the correlation, although positive, is not close to 1. The linear regression model had to consider more independent variables that were not contemplated; however, a significant value was obtained.
The objective of the correlation between cardiovascular risk and the thickness of the carotid intima layer in hypertensive patients between 30 and 50 years of age was achieved, further delimiting the greater correlation of the thickening of the intima layer of the right carotid artery, as well as the risk of presenting arteriosclerotic plaques with the type of cardiovascular risk, allowing future research to corroborate these details.
To the staff of the Family Medicine Unit No.13 of the North Delegation of the Mexican Social Security Institute who contributed to making this article a reality and to the team of researchers who successfully completed this research study.
The researchers of this article declare that there is no economic conflict or conflict of interest.
Study carried out at the Obstetrics and Gynecology Hospital/ Unit for Family Medicine (U.M.F.) No.13 of the Decentralized Administrative Operation Organ (O.O.A.D.) of the Northern Delegation of the Federal District (North D.F.) of the Mexican Institute of Social Security (I.M.S.S.). Tel: 55 55 61 16 87 Ext. 21301.


