Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Zhipeng Chen1+, Fan Lin2+, Yuanling Huang2, Chun Yan1, Jianbing He1, Chao Hu1, Chaohui Wu1, Zhe Li1, Xiong Lin1, Hongbing Duan1* and Sunkui Ke1*
Received: December 19, 2022; Published: January 04, 2023
*Corresponding author: Sunkui Ke and Hongbing Duan Department of Thoracic Surgery, Zhongshan Hospital of Xiamen University, Xiamen, Fujian, China
+These authors have contributed equally to this work and share first authorship
DOI: 10.26717/BJSTR.2023.47.007565
Migration of the peripherally inserted central catheter (PICC) into the azygos vein (AV) occurs only infrequently. It is even rarer for the PICC to be severed during severance of the AV in the course of esophageal cancer surgery, and currently there are almost no reports on the treatment of this complication. Here, we present two cases in which PICC was accidentally broken off during the operation. But both patients recovered smoothly after being treated with proper strategies.
Esophageal cancer is one of the most common malignancies, ranking seventh in terms of incidence and sixth in mortality out of all malignant tumors worldwide. It has a poor prognosis due to its high invasiveness [1]. Patients with esophageal cancer are often found to be locally advanced. Neoadjuvant therapy followed by esophageal cancer surgery has been proven to be associated with overall survival benefits. PICC is widely used in patients undergoing preoperative chemotherapy for esophageal cancer since it can greatly alleviate the pain of repeated punctures in treatment and prevent chemical phlebitis and tissue necrosis caused by extravasation of chemotherapeutic drugs. However, PICC is also correlated with some significant complications, including venous perforation, hemorrhage, thrombosis, malposition, and especially migration, and they all get a great deal of attention [2]. The optimal position of the initial tip of PICC is currently under debate. However, in most instances, the desired location is usually the superior vena cava (SVC), which is located advantageously near the Cavo atrial junction [2]. Presently, it has been rarely reported in the literature that the PICC tip may migrate spontaneously from the SVC in the late stage to the azygos arch. We here report two successfully discharged cases in our department, attempt to explore the causes of migration, and share the countermeasures to prevent PICC from being accidentally cut off during surgery, which may provide a clinically valuable insight for thoracic surgeons.
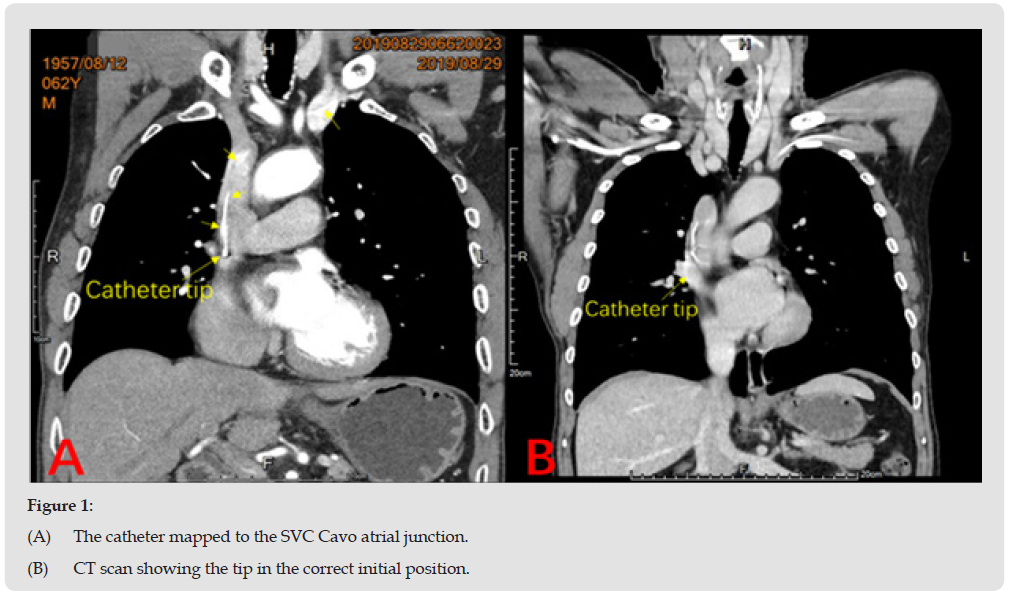
We here report two surgical cases in which the late spontaneous migration of PICC occurred in esophageal cancer patients. The two male patients, aged 62 and 57 years, respectively, and diagnosed with local advanced esophageal cancer, were admitted for surgery in 2019 and 2020, respectively. PICC was required for neoadjuvant chemotherapy before surgery. The time from first PICC catheterization to surgical operation was 62 days on average for the patient admitted in 2019 and 45 days on average for the other admitted in 2020. Two catheters (polyurethane, 7 Fr) were inserted via the left basal vein with ultrasound guidance, and both tips were proceeded through the axillary vein and the left subclavian vein to the left brachiocephalic vein and eventually placed in the SVC close to the Cavoatrial junction. The position of both tips was confirmed as satisfactory by a chest X-ray and a guide wire at the time of insertion. Initially, both catheters appeared static at the site of implantation. Then, infusion and aspiration, such as chemotherapeutic infusion, blood sampling, and contrast medium infusion, were unimpeded. Thoracic enhancement computed tomography (CT) was performed four and seven days before the operation, and it confirmed that the two PICC tips did not migrate (Figure 1). As soon as the PICC was surgically removed in both cases, the thoracic surgeons noticed that part of the catheter remained in the patients. Specifically, in patient A, when the azygos arch was severed after intraoperative double clamping with a Hem-o-Lok ligating clip.
Figure 1 (A) The catheter mapped to the SVC Cavo atrial junction. (B) CT scan showing the tip in the correct initial position.
we found that the catheter migrated into the AV as the arch was simultaneously severed (Figure 2A). This was because the Hemo- Lok was too close to the root of the AV and forced removal by thoracoscopic-assisted surgery may damage the SVC and cause massive bleeding. For safety reasons, thoracotomy was performed instead. The broken ends on both sides were temporarily clamped with vascular forceps to remove the Hem-o-Lok, and the AV was double-ligated with silk thread. Finally, the PICC was completely removed. In patient B, when the azygos arch was severed with a thoracoscopic linear cutting stapler, we discovered that the catheter had split (Figure2B). The proximal broken end of the AV was sutured with 4-0 Prolene thread in a purse-string manner. The urethral catheter was used to briefly block the blood vessels, and the PICC broken end was exposed by cutting the vascular anastomosis nail. The residual PICC was removed via the upper arm. The perivascular tissue was cleared, the sutures were loosened, and the proximal AV was reclosed with an endoscopic linear cutting stapler. The broken distal end of the AV was ligated with silk thread in a manner similar to that described for patient A, and the broken PICC end was exposed by detaching the vascular nail. The PICC stump was completely removed, and then the gap was sutured with 4-0 Prolene thread, thereby preventing any bleeding complications. Postoperative reexaminations, including chest radiograph and color ultrasound of the subclavian vein, confirmed the position of PICC tip and the absence of thrombosis.
Both patients had smooth operations without any serious complications such as postoperative hemorrhage or venous thrombosis. Finally, they were successfully discharged from our hospital.
Spontaneous migration of PICC tips into the AV is rare, and the migration mechanism is still unknown at present. According to previous work, it seems that flexible silicone catheters, increased intrathoracic pressure produced by vomiting and intense cough, vigorous movement of the upper extremities, left-sided PICC, and high-pressure infusions into the catheter may all contribute to PICC misplacement [3]. By reviewing two cases in our department, we analyzed and suggested possible reasons for spontaneous migration of PICC. First, rigid polyurethane rather than flexible silicone catheters were used in the two cases to reduce the risk of PICC migration. Second, strong catheter flushing and injection were strictly limited, because Lauren Lambeth, et al. [4] reported the cases in which PICC tips migrated into the right internal jugular vein or the right brachiocephalic vein during strong injection [4]. Third, the two patients did not show severe cough or vomiting during hospitalization, thus reducing the transient reversal of the blood flow inside the SVC induced by increased intrathoracic pressure and making it difficult for flexible catheters to dislodge from the SVC. We speculate that migration may be associated with violent arm movement. Forauer, et al. predicted that there was a tendency for PICC tips to move in a caudal direction as the position of the arm changed from abduction to adduction, with more than 2 cm PICC displacement in 58% of cases [5].
During surgery in our department, the two patients were able to change their position considerably. For example, raising the arms to allow better dissociation and resection of the tumor, which, however, also increased the possibility of spontaneous PICC dislodgment. Another risk factor is PICC placement from the left side. This may be related to the anatomical location. The AV enters the posterior aspect of the SVC facing the left brachiocephalic vein at the level of thoracic vertebrae T2-T5. The left brachiocephalic vein opens at the left anterior aspect of the SVC at the level of thoracic vertebrae T2-T3. There is a relatively shallow angle between the openings of the left brachiocephalic vein and the AV into the SVC. It may be better to break with conventional methods and choose a right-sided approach for PICC insertion.
In conclusion, we recommend that routine checks should be carried out before cutting the AV during surgical intervention for esophageal cancer patients with left-sided PICC, chest radiograph should be performed one day before surgery, and significant upper limb movement must be avoided during the perioperative period. Moreover, intraoperative confirmation that PICC does not enter the AV can be obtained using thoracoscopic non-invasive grasping forceps. Even if the PICC is accidentally severed during the operation, there are two recommended treatment approaches available to surgeons. Through these measures, the complication rate of PICC migration into the AV may be significantly reduced.
The authors have no conflicts of interest.
This work was supported by the Fujian Provincial Natural Science Foundation Projects (2018J01397) and the projects of Xiamen Science and Technology Commission (3502Z20184032).


