Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Svetlan Dermendzhiev1-3, Mihail Maznev1,3* and Eva Dimitrova4
Received: December 13, 2022; Published: December 22, 2022
*Corresponding author: Mihail Maznev, Department of Occupational Diseases and Toxicology, Second Department of Internal Medicine, Faculty of Medicine, Medical University-Plovdiv, 15-A Vassil Aprilov Blvd., 4000 Plovdiv, Bulgaria
DOI: 10.26717/BJSTR.2022.47.007555
The angioedema is one of the most common conditions in emergency medicine, and some particular forms, such as the hereditary angioedema, are associated with high risk of a fatal outcome, the reason for that being the localization of the angioedema near the larynx (in 40% of the cases). Studying the etiology and the intimate pathophysiological mechanisms of the angioedema contribute more and more for its phenotyping, which allows for more precise diagnostics of the disease, as well as its exact definition. This is prerequisite for a successful treatment of the angioedema and improved quality of life of the patients.
Aim: The aim of this mini review is to summarize the contemporary position of the world and the European scientific communities of Immunology and Allergology on angioneurotic swelling.
Materials and Methods: To accomplish the set goal, a database of the published current consensuses and guidelines of the World Allergology Organization (WAO), the European Academy of Allergology and Clinical Immunology (EAACI), the Global Allergy and Asthma European Network (GA²LEN), the European Dermatology Forum (EDF), the American Association of Allergology and Immunology (AAAI), the British Society for Allergology and Clinical Immunology (BSACI), as well as publications on the subject by a number of leading specialists was studied, analyzed and systematized.
Keywords: Angioedema; Definition; Epidemiology; Etiology; Pathogenesis
Keywords: WAO: World Allergology Organization; EAACI: European Academy of Allergology and Clinical Immunology; GA²LEN: Global Allergy and Asthma European Network; EDF: European Dermatology Forum; AAAI: American Association of Allergology and Immunology; HAE: Hereditary angioedema; HANE: Hereditary Angioneurotic Edema
The great Greek physician Hippocrates (377-460 BC), considered one of the most outstanding figures in the history of medicine and “Father of the Western Medicine,” already used the term oídēma to describe swelling of organs. It took many centuries until the first description of angioedema as a distinct medical entity was minted by Quinke in 1882, suspecting neurogenic factors [1]. Angiodema was first described in 1586 [2]. It is usually defined as a pronounced swelling of the deep dermis, subcutaneous or submucosal tissue, or mucosal membranes as a result of vascular leakage. Other terms such as giant urticaria [3], Quincke’s edema [4], angioneurotic edema [5], were also used in the past as a description of the condition. Angiodema can be described as a rapid and severe swelling of the deep dermis and subcutaneous tissue or mucosal membranes, it is accompanied by painful sensation, mild itching and slower evolution than in urticaria - up to 72 hours. This is the position of World Allergy Organization (WAO - World Allergy Organization) in 2012, ratified by members with the right to vote - Associations and Organizations under Allergology and Immunology from 54 countries, incl. and Bulgaria (out of a total of 84 members organizations) [6].
Modern Definitions
In most consensuses on the issue, angioedema is defined as a vascular reaction of deep skin/subcutaneous tissues or mucosal/ submucosal tissues with localized increased permeability of blood vessels, resulting in tissue edema. According to the British definition, angioedema is defined as a condition of transient swelling of the skin or submucosal surface, as a result of an increased vascular permeability of small blood vessels. The underlying skin can be normal or slighty erythematous [7]. Angiodema and chronic urticaria usually are present together, however they can also occur separately. Angioedama is a result of local increase in vascular permeability, often seen in the face, oropharynx, genitalia, and less commonly in the GI tract. The swellings can be painful rather than itchy. The disease involves the submucosa, deeper reticular dermis, and subcutaneous tissues [8]. The World and European Scientific Communities of Immunopathology and Allergology define angioedema as a vascular reaction of deep skin/subcutaneous tissues or mucosal/ submucosal tissues with localized increased permeability of blood vessels, leading to tissue edema. Angioedema can be bradykinin mediated or mast-cell mediated angioedema, including histamine. Primarily bradykinin-mediated angioedema can be hereditary or acquired, due to C1 inhibitor deficiency (C1-INH) or other mecha nisms [9]. Since angioedema is often combined with urticaria, the two conditions have a number of common triggers, triggering factors and similar pathophysiological mechanisms, it is necessary to pay attention to the modern definitions of the two diseases:
• Urticaria is a condition characterized by the development of hives, angioedema or both. Hives are characterized by a sharply limited superficial central edema, varying in size and shape, almost always surrounded by reflex erythema, itching or sometimes burning sensation; rapit transitory nature with restoration of the normal appearance of the skin after 30 minutes to 24 hours.
• Angioedema is characterized by sudden, marked erythematous or skin-colored, deep edema in the lower dermis and subcutaneous tissue or mucous membranes; tingling, burning, tension and sometimes pain, not so much itching; better reverse development compared to hives (up to 72 hours) [10].
Epidemiology
Data regarading the epidemiology of angioedema are limited, although it affects both adults and children and is not a rare disorder. In the USA is it considered, that angioedema is the second most common “allergic” disease over 13 years to necessitate hospitalization, exceeded only by asthma [11]. A large scale-study in Denmark found that 7,4% of the general population reported episodes of rapid swelling of the lips, tongue and skin. Few epidemiological studies have been published for non-HAE. Vazquez et al. found a lower prevalence of angioedema compared to the Danish observations (5% vs. 7.4%), however their analysis excluded acute angioedema. Zuberbier et al. reported a 19% prevalence of urticaria or angioedema. Non-hereditary angioedema often persists throughout life and becomes chronic in approximately 50% of affected patients [12].
Hereditary Angioedema
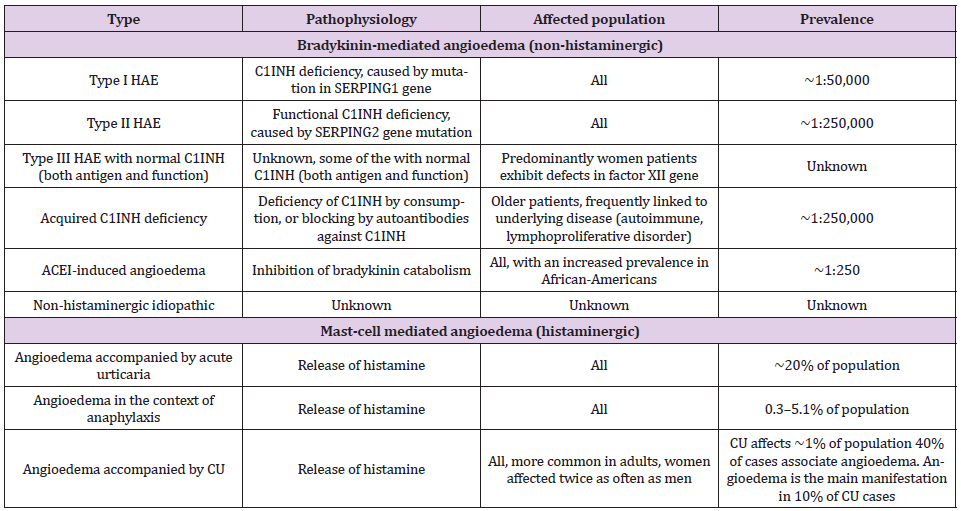
Hereditary angioedema (HAE) was first described clinically and genetically by William Osler in 1888 who originally named it” hereditary angioneurotic edema (HANE)”. It took 75 years from Osler’s report until Donaldson and Evans identified the central role of C1 inhibitor (C1-INH) in the pathophysiology of HANE. The modern definition of hereditary angioedema defines it as a hereditary disease characterized by recurrent episodes of non-pruritic swelling of the skin and submucosal tissues, which are associated with attacks of abdominal pain and life-threatening edema of the respiratory tract [13,14] (Table 1).
Table 1: Types of angioedema.Types of angioedema depending on pathophysiological mechanisms, affected population and prevalence rate [14].
Classification of Angioedema
Enrichment of knowledge on the etiology and pathogenesis of angioedema in recent years has led to the publication of various classifications. We consider the classification presented below to be the one of the most appropriate, given the fact that it systematizes modern concepts of the pathophysiology of the disease. In this classification, the three forms of angioedema being:
• Bradykinin-Mediated Angioedema:
- C1 inhibitor deficiency/defect – inharited (НАЕ-1 и НАЕ- 2) and acquiared (AAE-C1-INH)
- with normal C1 inhibitor (HAE-nC1-INH) – inherited (HAE-FXII, HAE-PLG, HAE-KNG1, HAE-HS3ST6, HAE-ANGPT1, HAE-MYOF, HAE-UNK due to mutations of respective factor XII, plasminogen, kininogen, heparan sulfate glucosamine 3-o-sulfotransferase 6, angiopoetin-1,myoferlin or unknown reasons) and acquiared (ACEI-AE, Angiotensin-converting enzyme inhibitor associated angioedema and other drug-induced angioedema such as ACE inhibitors, gliptine, neprilysin inhibitor or tissue plasminogen activators)
• Mast-Cell Mediated Angioedema:
- IgE mediated angioedema – angioedema associated with anaphylaxis, angioedema with urticaria/without urticaria
- non IgE mediated – angioedema with urticaria/without urticaria
• With an unknown mediator – idiopathic angioedema [15].
Pathogenesis of Angioedema:
Angioedema can develop through three main mechanisms:
• Mast-cell mediated angioedema (most common and associated with utricaria):
Mast-cell activation can occur by IgE antibody activation to specific antigens, physical stumuli or medication (non-IgE mediated mast-cell activation/direct activation of the mast -cell).
Once activated, mast cells release inflammatory mediators, such as: histamine, leukotrienes, prostaglandins and heparin.
• Bradykinin-mediated angioedema (non-associative with urticaria):
Bradykinin is an inflammatory mediator that leads to vasodilation and increased vascular permeability. Its amount increases either as a result of C1-inhibitor lowering and reduced inhibition of kinin production or as a result of increased ACE (angiotensin-converting enzyme) inhibition and reduced bradykinin degradation.
• Idiopathic angioedema with unknow mechanism.
Inflammatory mediators lead to an increase in vascular perme-ability and dilation of capillaries and venules. Extravasation of fluid from blood vessels occurs, causing asymmetric edema in the subcutaneous tissue and deep dermis. This edema occurs in the areas of the affected blood vessels and is not gravity dependent [16,17].
Knowledge about the etiology and pathophysiology of angioedema is constantly expanding and deepening.
This enables a more precise definition of the disease, identification of the triggering factor and determination of the leading pathophysiological mechanism in the specific patient.
Determination of the endotype and phenotype of angioedema allows its precise diagnosis.
Updating knowledge about the definition, etiology, pathogenesis and classification of angioedema is the key to accurate diagnosis and successful treatment of the disease.


