Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Gaia Zagolin1, Greta Loss1, Matilde Tasinato1, Roberto Cassino1, Gaia Degli Angeli1 and Rolando Tasinato1*
Received:November 29, 2022; Published:December 08, 2022
*Corresponding author: Rolando Tasinato MD, RSA Korian Sacra Famiglia – Pieve del Cairo (Retorbido (Pavia) Italy
DOI: 10.26717/BJSTR.2022.47.007516
This paper reports a randomized clinical trial about 81 patients with phlebostatic ulcers of the lower limbs who underwent treatment with topical application of Ozoile. The results were compared with a control group which did not receive the treatment. The trial lasted 9 months overall. Over this period of time, patients treated with Ozoile showed a statistically meaningful reduction (P value > 0.007) of mean re-epithelialization time compared to the control group. Biopsies of the floor and margins of the ulcers treated topically with Ozoile were performed and analyzed histologically and demonstrated that topical stable ozonides from biological olive oil application stimulates fibroblasts proliferation and neoangiogenesis. Such mechanisms, combined with debridement and compression therapy, make for an efficient treatment strategy for phlebostatic ulcers, providing treated patients with a reduction of healing time and better quality of life.
Keywords: Wound Care; Venous Ulcers;Ozone Therapy; Ozonized Oil; Bacteria; Neoangiogenesis; Chronic Cardiopathy; Sodium Hypochlorite; Infection; Phlebostatic; Neoangiogenesis
During the latest years, several experiences regarding topical ozone application for the treatment of chronic cutaneous lesions were reported in scientific literature. Ozone’s antiseptic properties have been exploited to reduce bacterial and microbial load mostly in bacteria-infected wounds and at the floor level of chronic cutaneous ulcers, both in acute and chronic phases [1]. In dermatology, ozone is used for the treatment of skin infections, especially those caused by pathogens that have developed resistance to conventional therapeutic approaches with antibiotics or antimycotic medications [2,3]. In addition, ozone stimulates regenerative processes that facilitate re-epithelialization of chronic skin ulcers. When bound to oil-rich substances, it remains firmly in contact with tissues, releasing molecular oxygen which can then exert its bacteriostatic and antiseptic activity on bacteria, anaerobes especially [4]. It was demonstrated that the presence of ozone in cultured tissues induces the production of endothelial growth factors, such as VEGF (Vascular Endothelial Growth Factor), that lead to the formation of new vessels, which improve blood flow to the floor and margins of the lesions. In vitro, ozone was also shown to induce fibroblasts migration towards the floor of the ulcer and facilitate neoangiogenesis. Different mixing techniques suggested in the past, although efficient, were often unable to supply stable preparations with progressive and controlled ozone release. Topical application of ozone-releasing preparations caught.
The interest of many teams working with acute and chronic skin lesions in the field of wound care [5,6]. Recently, we evaluated the use of Ozoile, a biological inducer obtained from a patented mixing process in which ozone is bound to olefinic bonds of fatty acids of a biological olive oil forming stable ozonides. The formula we used for the study is patented, produced and distributed in Italy by Erbagil S.r.l.
Between August 2021 and May 2022, a total of 81 patients was evaluated. These patients (43 men and 38 women aged 64.7 years on average, in a 49-83-year range) presented with chronic skin ulcers of the lower limbs of vascular origin. The ulcers had been active for at least 6 weeks and originated from venous vessels. The venous etiology of the lesions was documented in each case by clinical examination, Color-Doppler imaging and reflection photoplethysmography. Inclusion criteria comprised: being over 18 years of age, suffering from severe chronic venous insufficiency graded C6 on the CEAP classification and absence of other relevant comorbidities (such as NYHA class III or IV chronic cardiopathy, insulin-dependent diabetes mellitus, obesity with a BMI > 40, active neoplasm, COPD, concurrent treatment with corticosteroid or immunosuppressor drugs, legs arteriopathy with an ABI index < 0.7). Patients were subsequently randomized into two groups. Patients in group A (41 patients) were treated following the TIME protocol according to EWMA’s (European Wound Management Association) directions. Besides ulcer debridement, patients in this group underwent both compression therapy and application of Ozoile oil spray and Ozoile cream. Ozoile oil spray was applied to the floor of the ulcer, while the Ozoile-containing emulsion was applied to the perilesional skin. Group B patients were likewise treated with debridement according to the TIME model and cleansing with repeated washes of saline solution.
Followed by application of sodium hypochlorite 0.05% solution for about 3 minutes and compression therapy, but they did not undergo application of the Ozoile products. Medications were performed every 3 days on average. Short-stretch elastic cohesive bandages were applied, using the multi-layer technique, starting from the metatarsal region and proceeding upwards towards the knee, excluding the latter. After being applied the bandage, each patient was asked to walk, being given no functional limitation to his or her motor activity. The two groups of patients were treated by the same team, composed of 2 physicians and 3 nurses. Once the medication which was object of randomization had been performed, elastic bandages were applied following the same technique, with no differences between group A and group B. Patients randomization and data collection was performed independently through the use of a FH VMa Electronic Case Report Form (eCRF). All patients consented to the treatment and the two groups proved to be homogeneous in anthropological features and biographical data at statistical analysis. The patients randomized in the study were subjected to two weekly evaluations on average, every 3-4 days, to check on the status of their lesions scarring process and renew medication and bandages. Every week, ulcers size, depth and exudate entity were measured for each patient, and the acquired data set was reported in the medical records. The results of these periodic measurements were then inserted into an electronic database accompanied by photographic evidence.
The aim of the study was to investigate the presence of statistically significant differences in ulcers healing rate among the two groups.
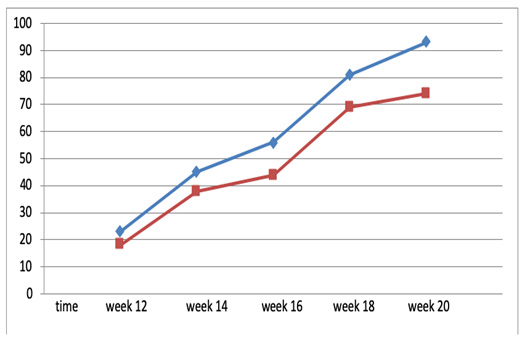
Patients were observed for a period of 10 months overall, during which 2 patients abandoned the study because of intercurrent SARS-CoV-2 infection. Final data refer to 79 patients (40 from group A, 39 from group B) who successfully concluded the therapeutic protocol showing healing of the ulcer. The trend for re-epithelialization time observed in the two groups is reported in (Figure 1). Phlebostatic ulcers healing rate was found to be higher in group A patients (patients treated with Ozoile) than in group B patients (control group). Independent statistical analysis of the data set shows that at 12 weeks past T0 mean healing time was reduced by 24.2%, at 16 weeks from T0 it was reduced by 26.3% and at 18 weeks by 15.1%. Overall, compared to the control group, the group of patients treated with both compression therapy and Ozoile topical application showed a mean reduction of about 23.8%. Mild atopic reaction to the Ozoile-containing cream was observed in group A, but treatment suspension was not necessary. In addition, in group A patients relied on analgesic therapy to a lesser extent than patients in group B and exudate control was more efficient. This aspect led the subjects to a faster return to their working activity and gave both patients and caregivers a better perception of their own quality of life.
Figure 1: Diagram analyzing the trend of the percentage of chronic venous ulcers that healed comparing group A and group B: patients in group A treated with Ozoile and patients in group B treated with standard treatment.
In a first phase, Ozoile application to the floor of the ulcers shows faster debridement of the treated lesions. Ozone release into the cellular medium favors cleansing of the floor from bacterial and fungal populations in the biofilm both via stimulation of autolytic debridement and via antiseptic action of ozone itself [7,8]. In our study, this action characterizes the first 2-3 weeks of treatment (Figure 2). Some patients underwent histological examination with a 5 mm punch biopsy sampling the floor and margins of the lesion. Optical microscope examination then allowed to highlight the efficacy of Ozoile-containing preparations in promoting reparative processes, mostly granulation tissue formation and neoangiogenesis accompanying the process of re-epithelialization [9,10]. Evaluation of the histological images shows that when applied to the ulcer floor and to perilesional skin Ozoile is capable of stimulating activation of cellular lines responsible for tissue repair in chronic ulcerative lesions [11] (Figure 3). Moreover, qualitative and quantitative examinations of the cell populations revealed through microscopy confirm that progressive application of the Ozoile-based preparation has anti-inflammatory effect, followed by a remarkable reduction in the number of inflammatory response-related cells. This effect can be observed starting from the third week of application on average and lasts up until the scarring process is complete [12-14]. By stimulating repair processes, Ozoile application is responsible for a temporary flareup of the lesion.
This temporary transformation of the lesion from chronic to acute paves the way for the initialization of the re-epithelialization process carried out mainly through fibroblasts migration and subsequent formation of newly-vascularized epithelium [15- 19].Stimulation of the repair processes is also noticeable in the histological examinations of patients in group B, who were not treated with Ozoile, but cell populations involved in scar formation and neoangiogenesis appear later and less remarkably than in group A (Figure 4).
Figure 2: Optical microscopy images obtained from incisional biopsies of the perilesional skin of a patient after 4 applications of Ozoile oil Spray to the floor of the lesion and Ozoile cream to the perilesional skin. The biopsies were performed 21 days after application of the medication (Fig. A and B T0 – Fig. C and D T1): After 3 weeks, the epithelium appears more structured and stratified and several newly-formed small vessels appear in the connective tissue under the derma, indicating the presence of active neon angiogenesis.

Figure 3: Histological sample with hematoxylin and eosin stain. The biopsy was obtained from the floor of a chronic ulcerative skin lesion of phlebostatic origin. The patient (male, 63 years old) was treated with sequential applications of Ozoile oil Spray and Ozoile cream to the perilesional skin. Observation at T0 is reported in Fig. A: besides tissue dismantlement, notable bacterial contamination can be seen. In Fig. B, representing a biopsy obtained after 4 weeks of treatment, there appear areas of granulation tissue and neo angiogenesis.
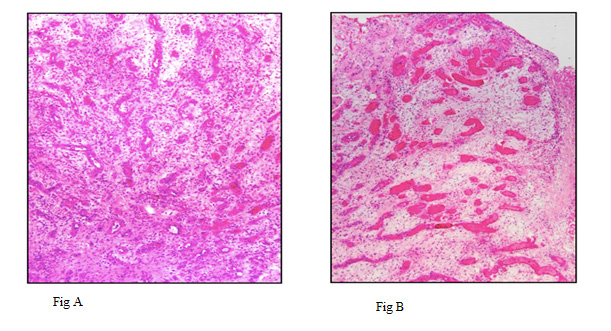
Figure 4: Higher magnification detail. Active fibroblasts proliferation and neoangiogenesis can be observed.

Debridement and compression therapy are regarded as the gold standard treatment for chronic venous ulcers [20,21]. The duration of the treatment is influenced by the quality of the medication. In our experience, the use of stable ozonides from biological olive oil (Ozoile)-containing preparations offers remarkable advantages by means of increasing ulcer re-epithelialization. In addition, Ozoile stimulates epithelial regenerative processes [22,23] and reduces bacterial load at the floor of the ulcer.


