Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Ramy Amirah1* and Dolores Petrovic2
Received: November 28, 2022; Published: December 07, 2022
*Corresponding author: Ramy Amirah, Department of Neurosurgery, Medical Center, University of Freiburg, Freiburg, Germany. Breisacher Str. 64, 79106, Freiburg, Germany
DOI: 10.26717/BJSTR.2022.47.007508
The spontaneous intracranial hypotension (SIH) is one of the most underestimated causes of chronic posture-dependent headache. Although the manifestation of SIH is primarily cranial, the pathology is most often spinal. The diagnosis of SIH is in many cases challenging because of the need of many radiological examinations (MRI of the head, MRI the whole spin, spinal Myelography and possibly post myelography CT. The treatment in many cases can be with blood patch. If a CSF-leak despite all the examinations not identified. If a spinal CSF-leak is identified radiologically, a surgical closure may be appropriate.
Keywords: Spontaneous Intracranial Hypotension; Orthostatic Headache
Abbreviations SIH: Spontaneous Intracranial Hypotension; CSF: Cerebrospinal Fluid
A 26-year-old woman reports postural headaches that have been present for 4 months. Initial therapy with bed rest and NSAIDs did not reduce the symptom. The cCT showed normal findings. Over time, the symptoms worsened further. In addition, there are intermittent dizziness, concentration disorders, sensitivity to light, ringing in the ears and physical weakness. The orthostatic headache was very noticeable that the patient could sit or stand upright for a maximum of 5-10 minutes. When lying flat, the pain was significantly reduced (VAS from 8/10 to 3/10). As a result, the patient was unable to work with a clear impairment of everyday activities, routine sport (like jogging, cycling) was no longer possible. A spontaneous intracranial hypotension (SIH) was clinically suspected, an MRI of the head and spinal axis was performed. The cMRI showed signs of widening of the venous sinus, pachymeningeal enhancement, narrowing of the suprasellar cistern (=4mm), as well as narrowing of the prepontine distance (=5mm) and narrowing of the mammillopontine distance (=6.5mm). The MRI of the spinal column showed evidence of epidural fluid with expansion in 3 segments C7/T1 (2) L2/S2, primarily dorsal. In the supplementary myelography, there was an indication of a definitive lateral CSF leak in LWK 1/2 on the right (type 2 according to Farb).
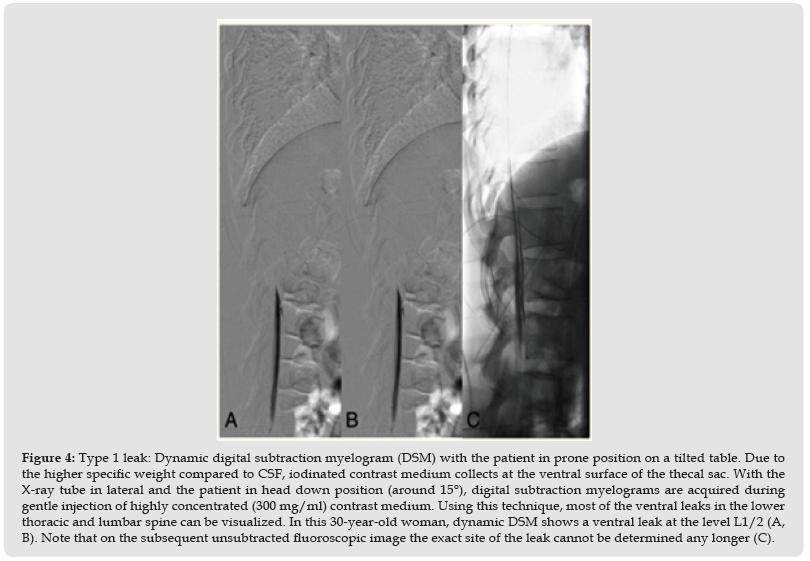
We determined the indication to surgical closure of CSF-leak in segment L1/2 on the right side. The operation was performed using minimally invasive microsurgical technique. A CSF-leak was microscopically viewed in situ. Closure was performed with fibrin glue from extradural as well as subdural. The patient was extubated immediately postoperatively. The next day the patient walked without any problems. New focal neurological deficits did not occur. The patient reported a significant improvement in orthostatic headache; however, there was a new type of headache in terms of pressure pain with slight intraocular pressure, especially when lying flat. After 2 weeks postoperatively, the headaches had completely resolved (Figure 1).
Figure 1 Myelography in the right lateral position showed evidence of leakage of CSF at level L1 on the right (blue arrow).
The clinical presentation SIH often went unrecognized for years. Symptoms vary, and a typical orthostatic headache may appear only at the onset of the disease. Over time, symptoms change and become more diffuse. [1]. The estimated annual incidence of orthostatic headache syndrome by spontaneous intracranial hypotension (SIH) is 5/100,000 [2]. It is etiologically separated from post-puncture headache and postoperative CSF loss [2]. Females are more often affected than males (2:1), the peak incidence is around 40 years of age, and SIH is rare but not absent in children [3,4]. The main symptom is an orthostatic headache, which usually begins or worsens within 15 minutes of sitting upright and tends to increase in severity throughout the day. Most patients can clearly identify the day headaches and other symptoms began [5]. The headache is most pronounced in the back of the head, which can be explained as the result of the following causal sequence: low CSF volume, sagging of the brain, tension on the cranial nerves and dura mater. The dura mater is especially tension-sensitive in the posterior fossa [5]. About half of all patients complain of hearing loss (ringing in the ears, tinnitus, pressure in the ear) possibly by altering the pressure or traction within the labyrinth in VIII cranial nerve, and some patients undergo initial treatment for suspected sudden hearing loss or Meniere’s disease [6].
SIH can present with a variety of symptoms ranging from coma to frank frontotemporal dementia [7]. According to the third edition of the International Classification of Headache Disorders, the criteria required for the diagnosis of headache attributed to low CSF pressure and SIH are
1) Low CSF pressure (<60 mm of H20) and/or evidence of CSF leakage on imaging.
2) A headache developing in temporal relation to and leading to the discovery of low CSF pressure or CSF leakage.
3) The absence of a causative mechanism that was better accounted for by another diagnosis in the International Classification of Headache Disorders, third edition [2].
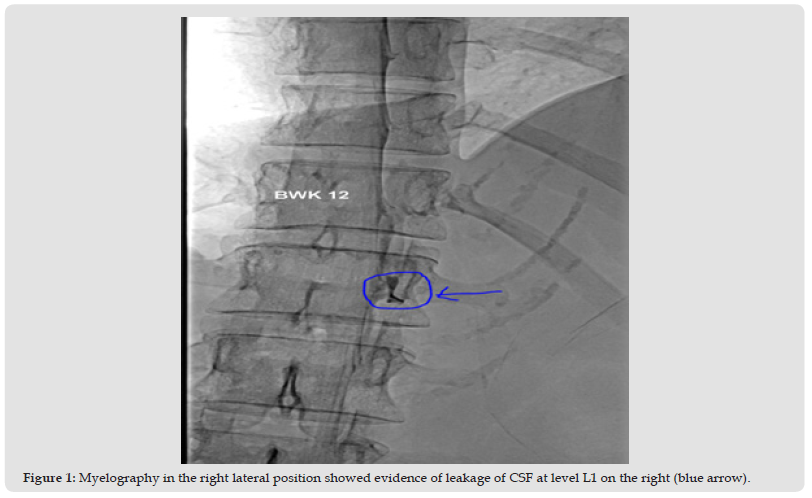
The MRI shows by 80% diffuse thickening of the meninges with contrast uptake due to hyperemia; reduced ventricular size (or ventricular collapse); hygroma; caudal ‘sagging’ of the brain, ‘midbrain elongation’, pontomencephalic angle and decreased Mamirillo pontine distance, caudal displacement of the brainstem with low tonsils like Chiari-I-malformation, hypertrophy of the pituitary gland, meningeal hemosiderosis, rarely vasogenic edema of the thalamus and basal ganglia with subsequent coma, dilation of the sinuses, cerebral veins and spinal venous plexuses, dural ectasia and epidural fluid storage. Doblocky, et al. [8] proposed the most accurate MRI signature score in 2019. This is later called the Bern score [8]. This scoring system integrates the 6 most relevant brain MRI findings and allows stratification of patients with SIH according to the presence of extradural contrast on postmyelographic CT. The score is based on 3 qualitative and 3 quantitative signs and provides high diagnostic accuracy [8] (Figure 2 & Table 1). In the spinal MRI show so-called spinal longitudinal extradural fluid (contrast) (SLEC) in 60% of patients and sometimes an underlying bony spur. Therefore, MRI scans of the head and the spine scans should be performed [9] (Figure 3). Approximately 60% are ventral dural tears, typically with small osteophytes penetrating the longitudinal section of the dura (type 1 leakage = SLEC positive). About 20% have a leaky nerve root sheath.
Figure 2Illustration of typical findings on brain magnetic resonance imaging in intracranial hypertension. A. Coronal illustration of the brain demonstrating normal findings. B. Coronal illustration of the brain with typical findings in a patient with a spinal cerebrospinal fluid leak with venous engorgement of the superior sagittal sinus (arrowhead 1), pachymeningeal enhancement (arrowhead 2), superficial siderosis (arrowhead 3), enlarged pituitary gland (arrowhead 4), prominent intercavernous sinus (arrowhead 5), effaced suprasellar cistern (arrowhead 6), and subdural fluid collection (arrowhead 7). C. Sagittal illustration of the posterior fossa demonstrating normal findings. D. Sagittal illustration of the posterior fossa with typical findings in patients with a spinal cerebrospinal fluid leak with effaced suprasellar cistern (arrowhead 8; pathologic ≤4 mm), effacement of the prepontine cistern (arrowhead 9; pathologic ≤5 mm), decreased mamillopontine distance (arrowhead 10; pathologic ≤6.5 mm), and low-lying cerebellar tonsils (arrowhead 11) [8].
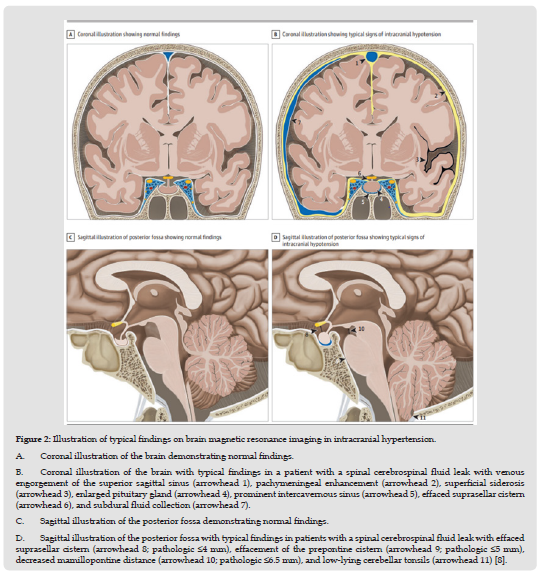
The leak is usually located in the shoulder of the meningeal diverticulum of the nerve root cuff (type 2 leak, mostly his SLECpositive) (10). If the dural tear of the nerve root sleeve is distal, there is no CSF within the epidural space (type 2 leak, SLECnegative or type 4 leak according to Farb, respectively) [10]. If there is a suspicion of ventral leak, the next step is dynamic (digital subtraction) myelography. The patient will lie face down. The head of the table is tilted downward while lateral fluoroscopy or digital subtraction images are acquired during gentle intrathecal contrast injection [11]. The goal is to locate the ventral dural tear by exactly locating the point of egress of iodinated contrast medium into the epidural space [9]. The known initial therapy is bed rest and medication with coffein oder Theophyllin shows sometimes symptom relief [12]. The use of one or more epidural blood patches shows significant improvement in 30-70% of patients with SIH. However, he is less than 10% of patients with Type 1 and Type 2 leaks permanently cured [13]. Surgical closure of the CSF leak is indicated when symptoms persist despite less invasive treatment and the CSF leak is definitely localized [14]. During surgery, the leak can be closed micro surgically using simple stitches or an adhesive patch of the dura [14]. A CSF venous fistula can be closed by surgical ligation (of the nerve root), injection of fibrin glue into the appropriate neural foramen, or liquid embolic endovascular injection into the root vein catheterized through the passageway [15] (Figure 4).
Figure 4 Type 1 leak: Dynamic digital subtraction myelogram (DSM) with the patient in prone position on a tilted table. Due to the higher specific weight compared to CSF, iodinated contrast medium collects at the ventral surface of the thecal sac. With the X-ray tube in lateral and the patient in head down position (around 15°), digital subtraction myelograms are acquired during gentle injection of highly concentrated (300 mg/ml) contrast medium. Using this technique, most of the ventral leaks in the lower thoracic and lumbar spine can be visualized. In this 30-year-old woman, dynamic DSM shows a ventral leak at the level L1/2 (A,B). Note that on the subsequent unsubtracted fluoroscopic image the exact site of the leak cannot be determined any longer (C).