Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Khaled Soliman1*, Abdullah Alrushoud1 and Rani Al Senan2
Received: September 22, 2022; Published: September 29, 2022
*Corresponding author: Khaled Soliman, Medical Physics Department, Prince Sultan Military Medical City, Riyadh, Saudi Arabia
DOI: 10.26717/BJSTR.2022.46.007359
The goal of this project was to investigate the feasibility of using radiochromic films (Gafchromic: XR-QA2) to estimate the peak skin dose (PSD) during Computed Tomography (CT) examination of the head. Implementation of the film dosimetry method described in this work allowed direct measurement of the axial radiation dose distribution without affecting the conduct of the imaging procedure. The measured peak entrance dose (Dpk) using films was associated with the volumetric computed tomography dose index (CTDIvol) by calculating a conversion factor (Cpk). The calculated Cpk conversion coefficient was 1.16 the average CTDIvol from 102 patients included in this study was 20.9 ± 9.1mGy, the Dpk was 24.3 ± 10.6 mGy and the PSD was 28.1 ± 12.2 mGy. There are no undesirable effects associated with the use of films as in-vivo dosimeters on the normal conduct of the CT head examinations. The main utility of the presented film dosimetry method is, it can be used during the conduct of any other CT examinations using protocols that include the use of large beam width and variable pitch factors of different than one. The method is scanner and protocol specific and can estimate the PSD of large number of studies by simple calculation.
Keywords: Radiochromic Films; In-Vivo Dosimetry; CTDI; Computed Tomography; Peak Skin Dose; CT Head
Abbreviations: AAPM: American Association of Physicists in Medicine; QA: Quality Assurance; CT: Computed Tomography; DPI: Dots Per Inch; IC: Ionization Chamber; PSD: Peak Skin Doses
There are more than 67 million CT examinations conducted in the United States; the contribution from CT imaging is almost forty nine percent from the total collective effective dose [1]. Medical imaging quality management programs require annual testing including patient dose measurements to be conducted annually [2]. CT scanners are part of the medical imaging equipment in the hospital and performing annual testing is thereby required. The American Association of Physicists in Medicine (AAPM), has recently published practice guidelines describing the importance of regular review of clinical protocols and such review constitute an important activity ensuring patient safety in diagnostic radiology. The review should also be part of the routinely performed quality assurance (QA) program for CT scanners. It is recommended to monitor radiation doses from most common CT examinations performed in the medical facility [3]. Computed tomography (CT) of the head helps to assess head injuries in the emergency department, severe headaches, dizziness, and other symptoms of aneurysm, bleeding, stroke, and brain tumors. It also helps to evaluate the face bones and injuries, sinuses, and the skull. Measuring entrance surface dose during CT examination has its place in clinical dosimetry today considering the current position of disagreement in the scientific community on which CT dose metric should be used to estimate the patient radiation dose [4-6]. The use of radiochromic films while performing Patient’s dose measurements have been extensively used in clinical dosimetry studies to monitor radiation exposure from imaging examinations including CT. [De Denaro, et al. [7]) showed that, the technique of using radiochromic film as in vivo dosimetry tool while performing radiation dose measurements seems encouraging in the direction of refining the assessment of the radiation effective dose received by the patients during scanning [7]. High levels of skin dose have been reported during CT brain perfusion studies. Therefore, careful examination of the skin dose is warranted during neurological CT examinations. Therefore, we have calculated the PSD during routine CT head examinations performed in tertiary care medical center. We have derived Conversion factor relating the scanner measured CTDIvol values and the PSD for one hundred and two patients in this study. PSD was calculated based on real measurements using films strips placed on the patient head rest over the CT couch and directly under the patients’ heads.
The hospital’s research ethics committee has approved this study.
Figure 1: Digitized XR-QA2 films in pixel values as function of the measured radiation Dose in [mGy].
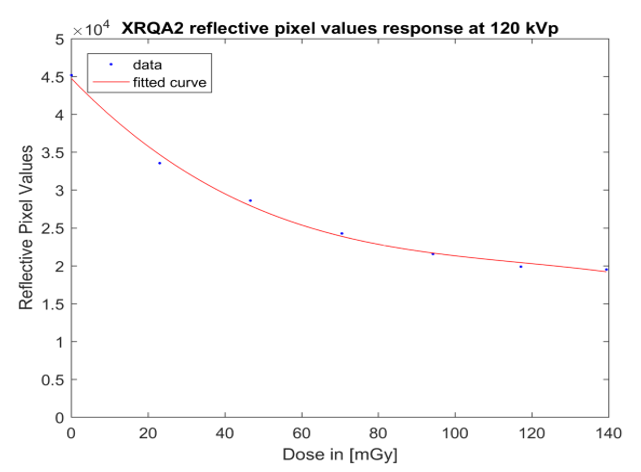
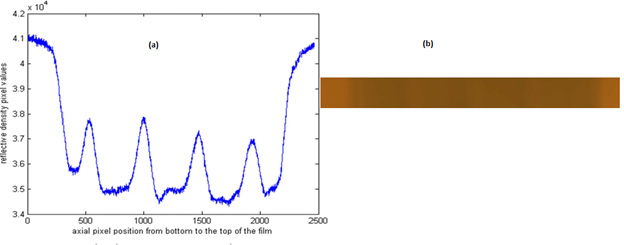
As described in our previous work, the XR-QA2 films (Lot Number: 07311401) were calibrated for air kerma free in air against the reading from PTW pancake calibrated ionization chamber (IC): PTW (SFD-type 34060 with calibration for the relevant X-ray energies and traceable to German National Laboratory (PTB). The electrometer used was the PTW UNIDOS E REF T10008 (S/N 081096) calibrated according to DIN EN ISO 9001:2008 [8]. The films were scanned 24 hours post irradiation Film digitization process was done using a flatbed high resolution scanner Epson 10000XL (Figure 1) shows the XR-QA2 films digitized pixel values as function of the radiation dose in [mGy] [9-10]. The film resolution was 48 bits for 3 colors mode, 16 bits for each color, red, green and blue (RGB). The film spatial resolution was 72 dots per inch (DPI), the films’ digital images were saved in TIFF format with no color correction [11-12]. The images were then exported to MATLAB software for analysis using in-house written program in Matlab R2016b (Natick, Massachusetts, US). The radiation Dose as a function of the films net reflective optical density (NRD) was then obtained as shown in (Figure 2). Few Pieces of film were placed at the center and on the top surface of PMMA block measuring around 30 by 30 cm; the thickness of each block was 15 cm. the calibrated Ionization Chamber was placed beside the films in the same radiation field. In order to avoid the heel effect of the bowtie filter the films were placed in the center of the field away from the edges. The films exposure was carried out using the X-ray tube in stationary position using the service mode operation of the CT scanner. The uncertainties were estimated using the method described in [9]. The average uncertainty value was estimated to be 8%. The irradiated film reflective optical density as a function of the scan axial (Z) positions is shown in (Figure 3a), along with a picture of the irradiated film in (Figure 3b).
Figure 2: Graph showing the relationship between the measured radiation dose in [mGy] and the XRQA2 film Net Reflective optical Density (NRD).
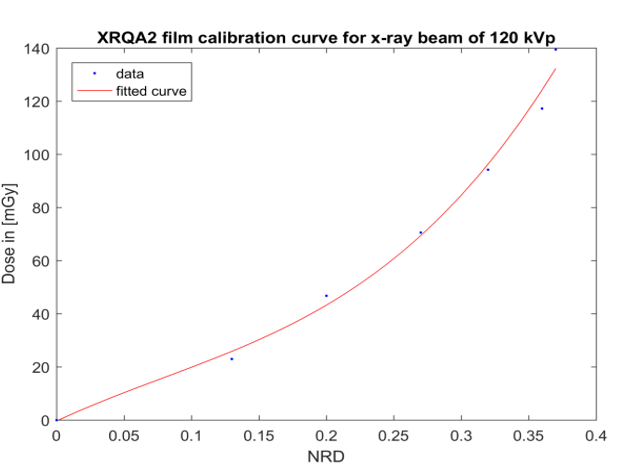
Figure 3:
a) The beam profile in the axial direction (Z) expressed as optical density values of the scanned film in reflective mode. We notice the sinusoidal shape of the profile which is a characteristic of the helical mode of acquisition with pitch factor of less than one.
b) XR-QA2 film slice placed under the patient head.
In order to check the uniformity of the dose distribution on the skin surface of patients undergoing head CT scans, heterogeneous anthropomorphic cross-sectional dosimetry phantom (CIRS ATOM, model 702-C) was used to simulate adult female head. Four pieces of film were placed in the following locations AP, PA, right lateral and left lateral. The phantom was scanned under the same clinical conditions as a patient. There was a slight difference between the radiation surface doses measured at the four locations the most important one was that the film at the PA location, the place where the clinical films will be placed during the in-vivo patient dose measurements were lower than the one in the AP location by 8% due to the patient table attenuation effect. Therefore, a correction factor fAP/PA = 1.08 will be applied to film measured dose in the results section.
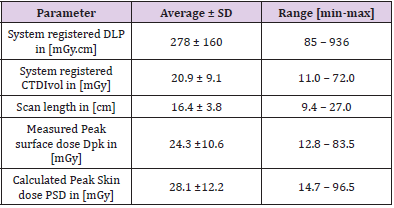
A piece of film about 25 cm long and 5 cm large was positioned on the patient head support, in order to measure the axial surface x-ray beam profile in the course of CT scanning of the head. This procedure was performed on 102 patients included in this study (Table 1) has the details of the head scanning protocol that will differ according to the clinical indication on the imaging request. The one in the table is the most probable one. We have calculated a conversion factor that relates the peak value of the measured Surface dose (DPK) using radiochromic films and the scanner registered CTDIvol as follows:
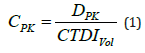
And the peak skin dose (PSD) as:
Where fAP/PA is a correction factor that corrects for the beam
orientation during the measurements. The DS was measured
with the radiochromic films positioned under the patients’ head
in the PA direction of the x-ray beam and if the beam is directed in the AP direction the results would be higher since the DS measured
using the anthropomorphic female phantom was lower
in the PA direction by 8% therefore we applied fAP/PA of 1.08 here  correction
factor to correct for the mass attention coefficient difference
between air and tissue. The hospitals research ethics review committee
has approved this research project. Since the placement of
films did not interfere with the conduct of the individual patient
scanning procedure no consent form was necessary for this research.
correction
factor to correct for the mass attention coefficient difference
between air and tissue. The hospitals research ethics review committee
has approved this research project. Since the placement of
films did not interfere with the conduct of the individual patient
scanning procedure no consent form was necessary for this research.
The results were as follows:
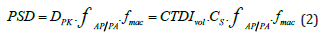
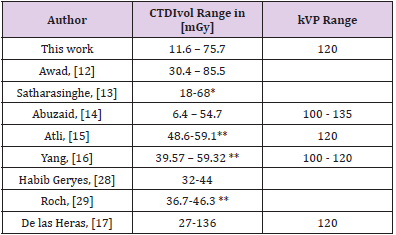
DPK=1.16 ∙ CTDIvol this seems to indicate that the peak entrance surface dose is 16% higher than the scanner reported CTDIvol (Table 2) has the summary of the results. The XRQA2 film calibration curve was fitted using a polynomial function of degree 3 (R2 = 0.9917) as follows:
Table 2: DLP, CTDIvol, scan length, Dpk and PSD and values obtained for the CT head examination for 102 patients included in this study.
With: p1 = 2484, p2 = -588.7, p3 = 236.5, p4 = -0.417. x is the NRD and y = the measured dose in [mGy].
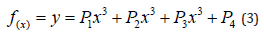
The above results shall enable the clinical medical physicist to perform accurate estimations of the actual peak skin doses (PSD) encountered during head CT imaging studies in general. The reported values are scanner specific and subject to change with scanner model, vendor and imaging protocol. The general conclusions presented here are considered as typical characteristics of the CT head scanning protocols customarily used in clinics (Table 3) has the results of other reported work on patients’ doses during head CT examination for comparison purposes [13-18,19,20]. One of the advantages of using the radiochromic films dosimetry is its ability to show beam profile, allowing the medical physicist to verify that the entire radiation dose has been captured eliminating the need for applying additional correction factors to correct for the loss of the radiation beam tail extension like what happens when using the classical 10 cm long ionization chamber routinely used for measuring the CTDIvol. In this work, measured conversion factor are driven relating system registered CTDIvol to the patient PSD measured at the surface free in air. Conversion factors will allow dose auditing by examining a large number of patient head CT dose reports available on the hospital PACS system from the same scanner and the same imaging protocol.
Table 3: DLP, CTDIvol, scan length, Dpk and PSD and values obtained for the CT head examination for 102 patients included in this study.
Radiochromic films have been used as direct measurement dosimeter during interventional radiology procedures [21,22]. It has been used to evaluate radiation beam profile in CT procedures [23- 25]. The films do not cause any interference with the patient imaging procedure [26,27]. XR-QA films were used to perform measurements of patient skin doses during CT examinations in-vivo using Rando Phantom [28]. The measured dose range was from 0 to 200 mGy. The measured ESD was by including a maximum of eight film strips fixed on each patient’ skin surface and also by using a Rando phantom. Optical reflectance of the unexposed films was subtracted from the exposed ones in order to calculate the net reflectance gain. They detected a sinusoidal shape along the scanning axis due to the helical movement of the x-ray tube. In another study, CTDIvol was found to overestimates the PSD and eye lens doses in brain perfusion CT scans in a simulation study [27]. The surface dose distribution was found to be affected by the CT scanning protocol parameters like pitch factor, tube starting angle and beam collimation [28]. The most suitable application of the method presented here is perhaps during clinical dose audits including measurements of surface dose distribution and to evaluation of PSD in CT protocols using large beam width and pitch factors different than one. The disadvantage of using radiochromic films is it is consumable and there are associated costs to purchase newly manufactured film batches. The shelf life of the films is one year to perform accurate dosimetry. The presented method is protocol and scanner and dependent, calibration must be repeated for each film batch used in the dosimetry study [29,30].
In this work, radiochromic films were successfully applied as In-vivo dosimeters used during the conduct of CT head examinations. The main benefit for using the film is its capability of capturing the spatial distribution of the radiation dose taken at the entrance body surface of the patient, therefore radiation dose profiles can be visually generated and it can be cross calibrated to measure radiation dose at the same time. The film does not obstruct the conduct of the actual patient scanning and does not produce imaging artifacts. The method maybe used to study other CT investigations routinely performed in radiology department. Simple estimate of the PSD using the data available in the structured radiation dose reports archived in the PACS systems is possible using the derived conversion factors. Imaging Medical physicists can use the presented method to investigate skin doses from CT scanning during their annual QA testing.


