Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Grethel Cisneros Domínguez1*, Carmen María Cisneros Domínguez2 and María Fernanda Fonseca Cisneros3
Received: September 08, 2022; Published: September 23, 2022
*Corresponding author: Grethel Cisneros Domínguez, University of Medical Sciences. Santiago de Cuba, Cuba
DOI: 10.26717/BJSTR.2022.46.007339
Within the dental practice, complications can occur due to the accidental ingestion of foreign bodies, causing medical emergencies. We present the case of a 23-year-old male patient in the General Surgery service of “Saturnino Lora” Provincial Clinical Surgical Teaching Hospital, who was admitted with a presumptive diagnosis of accidental ingestion of a foreign body, and the complementary tests carried out confirmed the presence of said foreign body in the digestive tract. Given the appearance of enterorrhagia by the patient, surgery was indicated, which was performed under general anesthesia, making a median infraumbilical incision, exploring the cavity and locating the foreign body at the level of the cecum. As operative findings were found: a Meckel’s diverticulum in its usual location and without complications; and a punctiform and reddened area located in the ileum that could explain the patient’s intestinal bleeding. Postoperative evolution was adequate, and the patient was discharged satisfactorily.
Keywords: Stomatological Practice; Foreign Body Ingestion; Meckel’s Diverticulum; Surgical Treatment; Surgery
A foreign body (Latin: corpus alienum) is any object coming from outside the body. It is a body or particle of biological or inert origin, introduced voluntarily or involuntarily in a place of the organism that does not correspond to it. The most common foreign bodies lodge in the eyes, ears, nose, respiratory tract, digestive tract, vagina, and wounds. [1] Within the dental practice, complications can occur due to the accidental ingestion of foreign bodies, caused by physical damage due to falling instruments, ingestion of foreign bodies and aspiration of foreign bodies and constitute a medical emergency [2]. The University of North Carolina concluded in 2015 that 5.5% of foreign bodies in the airways and digestive tract have a dental origin. Limper and Prakash, after 33 years of research, determined that the second most common cause of foreign body aspiration has the same origin. The ingestion or aspiration of a foreign body is an adverse event of great relevance due to its frequency and the commitment life that it entails. The most alarming thing, according to the literature consulted, is that the incidence of these events has not decreased over time, despite the fact that they are totally preventable accidents that carry high morbidity [2,3]. Ingestion is much more frequent than aspiration, due to the swallowing reflex that the patient has when a foreign object falls into the oral cavity, and its complications are less serious than in the case of aspiration [2,3]. Some authors establish that there are certain factors that increase the possibility of these accidents:
1. Age (due to decreased reflexes in older patients).
2. Medical conditions (Parkinson’s, dementia or cerebrovascular accident).
3. Use of general anesthetics, as well as states of consciousness altered by them [4]
4. The foreign bodies that can be aspirated or ingested during dental treatment are of a very varied nature: teeth, restorations, restoration materials, instruments, implant parts, gauzes, impression materials, drills, files, dentures [4] Most of the reports on the management of foreign bodies refer to infants and children where they are more frequent. Children can swallow a wide variety of objects that normally pass through the gastrointestinal tract without complications. Animal studies have shown that the intestine dilates in response to contact between the mucosa and a sharp object. This relaxation, combined with the axial flow in the lumen, tends to rotate sharp objects, which decreases the risk of perforation [1,5] The clinical manifestations are varied, the ingestion of a foreign body of any size can cause coughing and choking, followed by retrosternal pain that gives way with its passage to the stomach. Symptoms suggesting that the foreign body is in the esophagus include chest pain and hypersalivation, sometimes dyspnea due to compression of the larynx. Once in the stomach, 90 to 95% of all ingested foreign bodies pass without causing gastrointestinal symptoms. The presence of abdominal pain, fever, vomiting, hematemesis, melena, or peritoneal signs, poses complications that could be perforations or hemorrhages [1,5] The diagnosis should be suspected when the ingestion of a foreign body is confirmed by the family, so a simple frontal and lateral radiograph of the chest and abdomen should be systematically performed. Upper digestive tract endoscopy confirms the presence of the foreign body and allows the diagnosis of predisposing diseases and secondary mucosal lesions, as well as its removal [5]
When the object reaches the stomach, in most cases it will pass through the gastrointestinal tract without causing injury, so only radiopaque foreign bodies will be removed:
1) If they are caustic,
2) Large (greater than 5 cm),
3) Susceptible to intraperitoneal or intrahepatic migration (needles, for example) and
4) Present for more than 10 days.
When the foreign body is radiolucent, only an endoscopy will allow the object to be located and removed. If a conservative method is decided, a normal diet will be maintained and parents or relatives will be instructed to screen the stool. If after 5 days the object is not found, an abdominal x-ray will be obtained and repeated every 5 days until expulsion is confirmed. Laxatives are contraindicated since they accelerate intestinal motility, increasing the risk of perforation [6] When serial radiographs show progressive movement of the foreign body through the intestinal tract, the course will be uncomplicated. A sharp object that remains in the same place for more than 5 days may have penetrated the intestinal wall or become lodged in a Meckel’s diverticulum or appendix; In these situations, immediate surgical intervention is required because it can be lethal to the life of the patient [6]
This is an OMN male patient, 23 years old, with a history of psychiatric disorder approximately 7 years ago, who is currently compensated, for which he does not receive pharmacological treatment. He was brought to the Emergency Room of the ¨Saturnino Lora¨ Hospital in this city, accompanied by the attending dentist, reporting that during the placement of a fixed prosthesis in the upper central incisors, an instrument type screwdriver accidentally fell on the ground. From the mouth and despite the maneuvers carried out by the professional, the patient swallowed the Stomatological instrument. Upon receiving the patient in the Surgical Guard Unit, he reported slight discomfort due to swallowing the object. It is then decided to interrogate and examine him.
a. Personal medical history: psychiatric disorders.
b. Family pathological history: Does not refer
c. Adverse drug reaction: Does not refer
d. Toxic habits: drink coffee.
e. Transfusions: does not refer.
f. Previous operations: videoendoscopic cholecystectomy.
g. Injuries: Does not refer
i. Mucous membranes: normal colored and moist.
ii. Subcutaneous Cellular Tissue: not infiltrated.
iii. Neck: normally configured, there is no crepitus when examining the subcutaneous cellular tissue, nor pain on superficial and deep palpation.
iv. Respiratory system: normal chest expandability, polypnea of 27 breaths per minute, normal vocal vibrations, no crackles.
v. Cardiovascular system: Rhythmic heart sounds, tachycardia. Peripheral pulses present and synchronous. Heart rate: 107/min. Blood pressure: 120/80 mmHg.
vi. Abdomen: soft, depressible, following respiratory movements, not painful on superficial and deep palpation, without peritoneal reaction. Normal hydro-air noises of 9 RHA/ min.
vii. Nervous system: Patient oriented in time, space and person, who responds to questioning with clear language and anxiety. No signs of neurological focalization.
i. Complete blood count: hemoglobin 13.8 g/L, leukogram 5.9x109/L, segmented 63c/mm3, lymphocytes 28 c/mm3, eosinophils 3 c/mm3, basophils 1 c/mm3, monocytes 5 c/ mm3.
ii. Coagulogram: platelet count 250 x109 /L, retractable clot, bleeding time: 1 min.
Figure 2: Plain X-ray of the abdomen in postero-anterior view, where a radiopaque object is observed at the level of the gastric chamber that corresponds to the foreign body.

It is decided to perform a simple chest X-ray study in posteroanterior view (Figure 1) trying to locate the foreign body or any injury that it could have caused, but the foreign body cannot be visualized and there is no clinical evidence either. As radiological subcutaneous emphysema in the neck region (to rule out perforation of the upper portion of the esophagus). It was decided to perform a simple X-ray of the abdomen in postero-anterior view (Figure 2), observing the foreign body in the projection of the gastric chamber. explaining that the foreign body can be expelled in the next few hours, and that he returns to the center before any new symptom. Approximately 6 hours later, the patient returned to the emergency room reporting that he had diffuse abdominal pain, discomfort, and had not defecated. In addition to showing anxiety, both him and his family, for which reason the simple abdominal X-ray was repeated (Figure 3), observing a progression of the foreign body that ‘’impressed’’ to be in the left colon (for which it is decided to admit the patient for better follow-up in the room). explaining that the foreign body can be expelled in the next few hours, and that he returns to the center before any new symptom. Approximately 6 hours later, the patient returned to the emergency room reporting that he had diffuse abdominal pain, discomfort, and had not defecated. In addition to showing anxiety, both him and his family, for which reason the simple abdominal X-ray was repeated (Figure 3), observing a progression of the foreign body that ‘’impressed’’ to be in the left colon (for which it is decided to admit the patient for better follow-up in the room). The patient undergoes a normal postoperative period, after 48 hours the Levine catheter is removed, after 72 hours he begins a normal diet and after 4 days he is discharged and is followed up by outpatient surgery (Figures 4 & 5).
Figure 3: Plain X-ray of the abdomen in postero-anterior view, where the foreign body is observed that ‘’impressed to be in the left colon’’ and was actually in the ileum.

Figure 4: Meckel’s diverticulum of approximately 5 cm in length and 2 cm in diameter that turned out to be a finding during laparotomy.
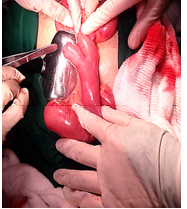
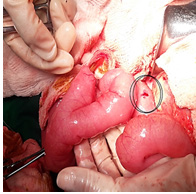
Figure 5: Within the circle, a reddened and punctate area is observed that explains the patient’s enterorrhagia and to the left the Meckel’s diverticulum found can be seen.
Various foreign bodies can enter the digestive tract intentionally or accidentally, which according to their location can be esophageal, gastric, intestinal or rectal. Many foreign bodies pass through the digestive tract spontaneously, but some become impacted and cause obstructive symptoms and sometimes complications. Almost all impacted objects can be removed endoscopically, but surgical intervention is occasionally necessary. The timing of endoscopy varies depending on the type of foreign body ingested. The most common complications of foreign body ingestion include ulceration, lacerations, perforation, GI obstruction, fistula formation, and bacteremia. Fortunately, between 80 and 90% of foreign bodies that reach the stomach are expelled spontaneously, although 10% to 20% require endoscopic removal and 1% surgical intervention [1,6] Deliberate and recurrent ingestion of a foreign body is described more frequently among inmates and psychiatric patients, with the main port of entry being the anal canal, with 53% of all cases of foreign bodies reported in patients over 18 years of age. Those who wear dental prostheses, the elderly, drunk people are prone to accidentally swallowing foreign bodies. [1,6] Of every 4 patients with ingestion of foreign bodies, 1 is hospitalized, and the observation of those who are not admitted is carried out on an outpatient basis, in coordination with the primary care physician, who is also the one who guides and diagnoses most cases. the patients [7] In many patients, the behavior that is followed is expectant, but in others, the behavior depends on its clinical manifestations and the physical-chemical characteristics of the object because it can pass without difficulty and be defecated. Sometimes the foreign body causes injuries to the hollow viscera, especially when trying to overcome valves and anatomical structures such as: The 3 physiological narrowings of the esophagus: below the cricopharyngeal muscle, at the level of the aortic arch and above the diaphragm; C-loop of the duodenum, ligament of Treitz, terminal ileus, ileocecal valve, and sigmoid colon (sites most frequently damaged and injured). When this occurs, the patient goes to the emergency room with severe peritonitis, which overshadows the evolution and prognosis of these patients [7]
Indications for endoscopic removal of foreign bodies in the gastrointestinal tract:
1. All esophageal.
2. Gastric and duodenal:
a) If they are sharp or pointed.
b) If they are more than 4 cm long.
c) If they are more than 2 cm wide.
d) If they contain caustic substances.
3. If they are stationary:
a. After 3 weeks of observation in the stomach.
b. After one week of observation in the duodenum [7]
Meckel’s diverticulum is the most frequent anomaly of the gastrointestinal tract, it occurs in 2% to 3% of the population. It was originally described by GuilhelmusFabriciusHildanus.9 It is clinically evident when complications such as ulceration and hemorrhage, diverticulitis, intestinal obstruction, among others, arise. Diagnosis is usually made in childhood, between 50% and 60% of patients who develop symptoms are under 2 years of age or there are occasions in which it is perforated, bleeds or inflames and makes the picture confuse with that of appendicitis acute [8,9] The diagnosis should be considered in any patient with unexplained abdominal discomfort, nausea and vomiting, or gastrointestinal bleeding. The most accurate diagnostic method for detecting Meckel’s diverticulum is the study with technetium-99m pertechnetate. Treatment is surgical [9,10]
Meckel’s diverticulum is commonly referred to as the rule of 23:
1. Occurs in 2% of the population.
2. Male/female ratio 2:1.
3. It is frequently located within 2 feet (60 cm) of the ileocecal valve, on the antimesenteric border.
4. It usually measures 2 cm in diameter.
5. Consistently measures 2 inches (5 cm) in length.
6. May contain 2 types of ectopic tissue (commonly gastric and pancreatic) [10].
Prognosis, treatment and management of complications.
The surgical approach to Meckel’s diverticulum depends on its diagnosis, whether it was a finding or whether the patient presented symptoms. Ileal resection allows removal of all affected tissue and ectopic tissue. There is great controversy about removing the diverticulum when it has been found incidentally [11,12].
The stomatologist must be prepared for complications of this type and apply established protocols in emergency situations, as well as maintain an ethical responsibility towards the patient regarding the event that has occurred and the possible behaviors to be followed outside the scope of the stomatology.
1. The therapeutic approach to a foreign body in the digestive tract depends on its shape, size, toxicity, location, clinical manifestations and time of evolution.
2. Endoscopic extraction techniques are ideal if there is easy access to it while maintaining conservative treatment based on patient surveillance for those who are in regions of easy expulsion.
3. Surgical treatment will be performed when there is no progression with intestinal peristalsis or when complications appear.


