Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Nasha Yu1, Xing Zhong1, Yong Wan2, Weiming Zhang1 and Wuping Li1*
Received: August 25, 2022; Published: September 02, 2022
*Corresponding author: Wuping Li, Departments of Lymphatic and Hematological Oncology, Jiangxi Cancer Hospital 519 Beijingdong Road, Nanchang, Jiangxi 330006, People’s Republic of China
DOI: 10.26717/BJSTR.2022.45.007279
Rationale: Primary breast lymphoma (PBL) is an uncommon and aggressive hematologic malignancy. PBL typically presents with isolated and painless breast mass with or without involvement of lymph nodes. PBL is mainly found in female patients. However, male breast involvement is rare and there has been no report describing primary peripheral T-cell lymphoma of breast in male patient. Patient concerns: We report a case of a 43-year-old male who presented with a 3-months history of a painless mass in the left breast.
Diagnoses: Breast ultrasonography was performed to evaluate the breast lesion. The lesion was depicted as irregular heterogeneous echoic mass of 30mm in diameter within the mammary zone of the left upper outer breast. Lumpectomy was performed for the breast lesion. Histologic diagnosis of the lesion was peripheral T cell lymphoma, not otherwise specified (PTCL-NOS).
Interventions: The patient was treated with 6 cycles of CHOPE induction chemotherapy and prophylactic intrathecal injection.
Outcomes: The patient remains in complete remission state without relapse at 36months since first complete remission.
Lessons: This is the first case of PTCL-NOS of the male primary breast. This case report is significant for the diagnosis of male breast lymphoma.
Keywords: Peripheral T Cell Lymphoma; Breast; Male; Therapy
Abbrevations: PBL: Primary Breast Lymphoma; PTCL: Peripheral T Cell Lymphoma
Primary breast lymphoma (PBL) is a rare Extra nodal lymphoma, accounts for about 0.04%-0.5% of all malignant breast tumors, and for 1.7-2.2% of extra nodal non-Hodgkin’s lymphoma (NHL) [1]. Almost 70-90% PBLs is non-Hodgkin’s lymphoma, and 40%-70% of breast lymphomas are diffuse large B-cell lymphoma (DLBCL) [2]. The typical clinical characteristic of PBL is an isolated and painless breast mass, rarely as multiple mass, or diffused breast enlargement. The mass is softer than breast cancer, and it is hard to be distinguished from that of breast cancer [2,3]. PBL is mainly found in female patients, accounting for 95%-100% of all the PBL patients. Few cases of PBL in male have been reported in the literature. However, to the best of our knowledge, there has been no report describing PTCL-NOS of the male primary breast. Herein, we report a case of rare PBL that presented as a breast parenchymal lesion in a 43-year-old man diagnosed with PTCLNOS of the left breast. A review of the previous literatures and the clinicopathologic features and treatment of PBL are also presented.
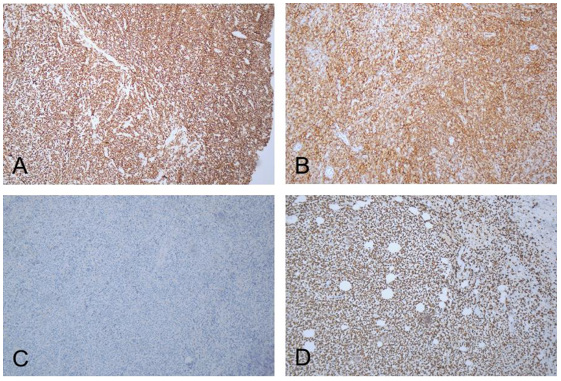
A 43-year-old previously well man presented with a 3-months history of a painless mass in the left breast, the mass without night’s fever, weat and weight loss (Figure 1). On palpation, a tumor with moderate hardness and 30mm in diameter was detected in the upper inner quadrant of the left breast, without enlarged lymph nodes. Ultrasound revealed irregular heterogeneous echoic mass of 30mm in diameter in the left breast. Whole body CT scan reveal a 2.5cm tumor that enhanced with contrast. Serum levels of tumor markers were within normal limits. Tests of EBV/ CMV-DNA and HIV, HBV, HCV were negative. The patient received lumpectomy. A tumor with irregular border measuring 30mm was found in the postoperative specimen and further immunostaining was performed. The results were positive for CD3 (Figure 2A), CD43(Figure 2B), CD45RO, and Ki-67(90%) (Figure 2D), otherwise negative for CK (Figure 2C), Pax-5, CD20, CD79α, CD21, Bcl-6, CD56, P63, MPO, CD34, ER and PR. Confirm a final diagnosis as of peripheral T cell lymphoma, not otherwise specified (PTCLNOS). Based on several laboratory and imaging examinations, the Ann Arbor stage was IAE, and IPI score was 0 (low risk group). The patient achieved complete remission after 6 cycles of CHOPE chemotherapy (cyclophosphamide, epirubicin, vincristine, prednisolone, and etoposide) and prophylactic intrathecal injection (methotrexate 12mg and cytarabine 50mg). Didn’t have given maintenance therapy. The patient is progress free survival for 36 months.
Figure 2: Immunohistochemical detection of breast tissue: A: CD3 positive B: CD43 positive C: CK negative D: Ki-67 positive.
Primary breast lymphoma is a relatively uncommon hematologic neoplasm that originates in the breast lymphoid tissue [4]. The incidence of PBL in the United States was 1.35 cases per million people, with an average age of 67.1 years and a median age of 69 years [5]. PBL is often found as a mass of unilateral breast which characterized by rapid growth and a relatively short ill duration [6,7]. As compared with breast cancer, the mass of PBL tend to be larger and softer at diagnosis, however the other characteristics such as skin retraction, erythema, peau d’orange appearance and nipple discharge are rare [8,9]. The common B symptoms in lymphoma, such as fever, night sweats and weight loss, are also rare in PBL [3]. Though mechanism of PBL were controversial, most researchers supported that PBL is closely related with hormone disorder, especially estrogen [10]. This view may explain the fact that PBL is mainly found in female and rare in male [1]. The risk factor of male PBL remains unclear, hormone disorder is also considered to be the most closely related factor of it [11]. Two reported cases of male PBL were diagnosed with the secondary sexual hormone disorder of liver cirrhosis [12] and prostate cancer patients [13], respectively. However, the case in our report is a young male patient without hormone disorder risk, suggesting other potential mechanism besides of sex hormones may involve in male PBL. The diagnosis of PBL is more difficult than that of breast cancer or breast fibroadenoma, we always give a diagnosis based on pathological and clinical finding [14]. The diagnostic criteria of PBL firstly been reported by Wiseman and Liao in 1972 [15] which was still in use today.
The criteria including:
1. The mammary gland tissue and tumor tissue have a close relationship;
2. An appropriate histopathological evaluation has been performed;
3. No malignant lymphoma is found at sites other than the mammary gland at the first visit, although ipsilateral axillary lymph node metastases may be present. Therefore, this case met these criteria and was diagnosed as malignant lymphoma of the mammary gland.
From the histopathology aspect, most all PBLs have a B-cell lineage, and 40%-70% of breast lymphomas are diffuse large B-cell lymphoma (DLBCL) [9], followed by follicular and MALT (mucosa associated lymphoid tissue) lymphoma. Peripheral T-cell lymphoma was uncommon, except of the anaplastic larger cell lymphoma (ALCL) which caused by the breast implant capsules used for reconstruction [16]. Therefore, a young male of PBL with T-cell lymphoma subtype was an extremely interested case. Several treatment options are available for primary breast lymphoma, such as chemotherapy as the first preference of treatment of primary- BL, and radiation as a second preference, followed by surgery. At present, PBL first-line chemotherapy needs at least 4 cycles of anthracycline-based therapy, and cyclophosphamide, adriamycin, vincristine and prednisone (CHOP) are the most accepted regimens [1]. Yhim, et al. [17] found that less than 4 cycles of chemotherapy are an independent prognostic factor to reduce PFS and OS. Most researchers believe that chemotherapy combined with local radiotherapy can achieve better results [18]. The mastectomy could not improve the survival of patients or prevent recurrence, while lymph node status could guide radiotherapy or chemotherapy [19]. Stage I patients with negative lymph nodes could benefit from radiotherapy, while stage II patients with positive lymph nodes could benefit from chemotherapy. Surgical intervention other than biopsy for definite diagnosis should be avoided. Recurrence of central nervous system (CNS) is one of the factors that affect the prognosis of PBL. Domestic scholars [7] have observed that a rate of CNS relapse of 10% with an estimated 10-year cumulative risk of 28.3% in primary Diffuse large B-cell lymphoma of breast. Aviv, et al. [20] believe that preventive intrathecal injection is recommended to reduce the risk of CNS recurrence when there are high risk factors (high IPI score, elevated LDH, bilateral breast involvement, etc.). However, Hossein, et al. [21] have found that patients with stage IIE and high IPI may be more prone to CNS recurrence, but its occurrence is not correlated with preventive lumbar puncture and intrathecal injection. Therefore, how to prevent PBL central recurrence needs further research.
This middle-aged male patient, whose left breast mass was diagnosed as Peripheral T-cell lymphoma by surgery and pathology, received 6 courses of CHOP chemotherapy and intrathecal injection prevention treatment. Due to complete surgical resection without local radiotherapy, comprehensive treatment achieved complete remission, and the disease was stable after follow-up. Our experience is that it is difficult to draw definitive conclusions about the treatment of primary breast lymphoma due to its rarity and widely reported differences in histopathology, staging, and clinical features. However, Peripheral T-cell lymphoma of primary breast is even rarer, and individualized treatment should be selected based on individual situation. Moreover, the data of male PBL is limited in China. This case provides reference materials for us to discuss the treatment of male PBL.
In conclusion, this is the first case of peripheral T-cell lymphoma of the male primary breast, and breast surgeons and oncologists should be aware of this rare disease.
There are no acknowledgments.
Writing – original draft: Nasha Yu
Writing – review: Xing Zhong, Yong Wang, Weiming Zhang
Writing – review & editing: Wuping Li.


