Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Valda Šližytė*
Received: July 14, 2022; Published: July 20, 2022
*Corresponding author: Valda Šližytė, Occupational therapist LSMUL KK Psychiatric Clinic, Lithuania and Assistant LSMUL KK Rehabilitation Clinic, Lithuania and Head public institution Independent Children, Lithuania
DOI: 10.26717/BJSTR.2022.45.007171
The Aim of the Research: To compare the change in independence during individual and group occupational therapy for children who have autism and excessive responses to tactual stimuli.
The Tasks of the Research:
1. To assess the responses of children with autism to tactual stimuli.
2. To evaluate individual occupational therapy for personal hygiene and upper/ lower body dressing in children with autism and excessive responses to tactual stimuli.
3. To evaluate group occupational therapy for personal hygiene and upper/lower body dressing in children with autism and excessive responses to tactual stimuli.
4. To investigate the parents’ opinion about the change of children’s independence by applying occupational therapy to children who have autism and excessive responses to tactual stimuli.
Methodology:</p>
1. Children’s functional independence test “Wee FIM test”
2. Touch Disorder Assessment Test.
3. Questionnaire for parents created by the author.
4. Statistical data analysis was performed using the data collection and analysis “SPSS 27” program package.
Participants: The study included 16 children aged 4-6 years with autism and excessive responses to tactual stimuli. Two groups were formed in which individual and group occupational therapy were applied.
Conclusion:
1. In children with autism, the responses to tactile stimuli before occupational therapy were increased, causing inadequate behavioral complications, after occupational therapy, negative reactions decreased and independence skills were statistically significantly improved (p <0,05).
2. For children with autism and excessive reactions to tactile stimuli, after individual occupational therapy together with the sensory-based interventions the hygiene and upper/lower body dressing skills improved significantly (p<0,05).
3. In children with autism and excessive reactions to tactile stimuli, after the group occupational therapy together with the sensory-based interventions, the hygiene and upper/lower body dressing skills improved significantly (p<0,05).
4. The parents of the children (87,5 pct.) who participated in the study were positive about occupational therapy sessions and noticed a change in independence when comparing children’s independence skills before and after occupational therapy, as well as a decrease in excessive reactions to tactile stimuli.
Every person wants to live independently, to be able to take care of himself and to freely engage in social life, to be a part of society. It is more difficult for children to do this because it takes time and effort to acquire the necessary skills. Every child is different, so their development and growth are also different. They observe the environment, explore it, create social roles during the game, and imitate the activities of those around them. In this way, more and more necessary skills are improved and acquired, the ultimate goal of which is independent performance of activities. Unfortunately, the development of independence can be limited by unfavorable factors. Most often it is related to health problems. More and more children in the world are diagnosed with autism, which disrupts the perception of the environment and self-service. Autism is a neurodevelopmental disorder that can manifest itself in early childhood with impaired social communication and repetitive abnormal sensorimotor behavior. Not only does it become more difficult for children to communicate, establish social relationships, but also to play and perceive the environment, therefore, without performing these activities, independence skills do not improve at the same time [1-3].
In the conducted scientific studies, it is increasingly observed that children who have autism also have sensory integration disorders. With these disorders, it is difficult for children to systematize, process and form the correct response from the information received from the environment. The inability to generate the correct response to the received sensation leads to cognitive impairments, as children learn through touch and exploration. Sensory integration disorders can manifest as sensory modulation, motor function and sensory discrimination disorders. In the presence of at least one of the listed types of disorder, the development of fine motor skills, the formation of appropriate behavior, the ability to communicate one’s feelings and thoughts, and therefore the development of independence skills are slowed down.
1. Assessment of children’s independence - Children’s Functional Independence Theta (Wee FIM). The WeeFIM instrument is intended for children from 6 months to 7 years of age. It consists of 18 items, which are evaluated on a seven-level scale. Out of 18 tasks, 7 tasks are classified as independent. Areas of activity include eating, dressing the upper and lower body, grooming, using the toilet and bath. The performance of each activity is evaluated with points: 7 – complete independence; 6 - modified independence; 5 - supervision is required (the child performs 100% of the tasks by himself); 4 – minimal assistance (performs 75% or more of the tasks); 3 – average assistance (performs from 50% to 75% of tasks independently); 2 – maximum assistance (performs from 25% to 49% of tasks independently); 1 – full help (no tasks).
2. Assessment of reactions to tactile stimuli - questionnaire for the assessment of tactile disorders. The questionnaire is based on C.B. Royeen’s Sensory Impairment Evaluation Test. Assessment 24 designed to assess tactile disorders. The questionnaire consists of 26 questions. Answers are scored. No - 1, a little - 2, a lot - 3. The options for each answer are added up separately and multiplied accordingly: the sum of “no” answers from 1, the sum of “a little” answers - from 2, the sum of “very” answers - from 3. The 4th touch is excluded impairment levels: slight (up to 35 points), moderate (from 36 to 50 points), marked (from 51 to 60 points), very marked (more than 60 points).
3. A questionnaire for parents created by the author. The purpose of the questionnaire is to assess parents’ opinions about the change in children’s independence after occupational therapy [4-7].
The study included 16 children aged 4-6 years with autism and excessive responses to tactual stimuli. Two groups were formed in which individual and group occupational therapy were applied.
16 children participated in the study, who were randomly divided into two groups of 8 children each. After calculating the criterion of independence (homogeneity) of characteristics, the groups are homogeneous. One group received individual occupational therapy combined with sensory intervention (group I, n=8), and the other group received occupational therapy combined with sensory intervention (group II, n=8). During the classes, children’s independence in the areas of personal hygiene and dressing of the upper and lower body was improved. A total of 12 boys and 4 girls participated in the study. There were 7 boys and 1 girl in the first group, and 5 boys and 3 girls in the second (Table 1). The average age of the children in the first group was 4.67±0.5 years, and in the second - 4.9±0.6 years. All subjects were diagnosed with autism.
Table 1: Compound annual growth rates in production and consumption of meat in the countries of West Asia region from 2000 to 2017.
Note: * and **indicate significant at 1 and 5per cent probability levels, while NS indicates non significant coefficient.
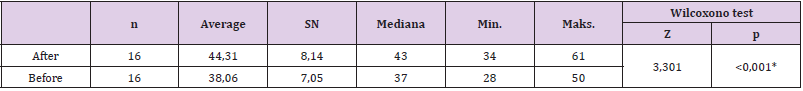
After conducting the assessment of touch disorders at the beginning of the study, the overall average of the assessment was 44.31±8.14, and at the end 38.06±7.05. As we can see, the evaluation score decreased by 6.25 points on average. This shows that unwanted reactions have decreased, the child is more involved and willing to perform activities that previously caused unwanted behavior. The median change was 6 points (pre-exposure was 43 points and post-exposure was 37 points). The obtained results were compared with each other using the Wilcoxon test, which calculated that the change was significant. (p<0.05). This shows that the children who participated in the study had a statistically significant reduction in adverse reactions to tactile stimuli with both individual and group occupational therapy combined with sensory intervention (Table 1). The obtained Touch Impairment Assessment scores were divided into 4 groups: slight tactile impairment (0-35), moderate (36-50), marked (51-60), very marked (more than 60). According to the evaluation results, at the beginning of the study, one subject in the first group had a very marked tactile disorder, two marked, moderate - four, and slight - one. In the second group, two subjects had significant tactile impairment, six had moderate, and one had mild. At the end of the study, in both groups we can see that the tactile disturbances have decreased. In the first group, five children had a moderate tactile disorder, three - insignificant. In the second group, moderate tactile impairment occurred in six subjects, and slight impairment in two. At the beginning of the study, the subjects usually had unwanted and too strong reactions during the following activities: dressing in fluffy clothes, drawing with fingers, playing with toys of different textures, getting dirty.
At the end of the study, the performance of activities improved, too strong and adverse reactions occurred less, from very marked and marked impairment, the subjects moved to moderate and slight impairment (Figure 1). The obtained functional independence WeeFIM assessment scores were divided into 4 groups. If the subject scores more than 90 points, he is classified as almost independent, and if he scores 0 points- totally addicting. In the first group, one subject required high to moderate assistance with activities and six subjects required moderate to low assistance before occupational therapy sessions. One subject was almost selfsufficient. After the occupational therapy sessions, three subjects were almost independent, and five subjects required moderate to little assistance with activities. In the second group, before exposure, two subjects were almost independent, and six required moderate to little assistance. After the occupational therapy sessions, the subjects in the second group were equally divided - four needed moderate to little assistance with activities, and the other four were almost independent (Figure 2).
Based on the received research data, fourteen parents (87.5%) said that the children’s independence increased after the applied occupational therapy. Two parents (12.5%) said that they did not notice a change in independence. None of the parents answered that independence did not increase. Thus, it can be assumed that occupational therapy improved the independence of children. In summary, we can say that after the applied ergotherapy, the independence of the subjects increased, involvement in activities and their performance improved, adverse reactions to tactile stimuli decreased. A significant change was observed before and after the exposure, but there was no significant change when comparing the groups. So, it means that both individual and group occupational therapy together with sensory intervention was effect [8-11].
1. In children with autism, the responses to tactile stimuli before occupational therapy were increased, causing inadequate behavioral complications, after occupational therapy, negative reactions decreased and independence skills were statistically significantly improved (p <0,05).
2. For children with autism and excessive reactions to tactile stimuli, after individual occupational therapy together with the sensory-based interventions the hygiene and upper/lower body dressing skills improved significantly (p<0,05). 3. In children with autism and excessive reactions to tactile stimuli, after the group occupational therapy together with the sensory-based interventions, the hygiene and upper/ lower body dressing skills improved significantly (p<0,05). 4. The parents of the children (87,5 pct.) who participated in the study were positive about occupational therapy sessions and noticed a change in independence when comparing children’s independence skills before and after occupational therapy, as well as a decrease in excessive reactions to tactile stimuli.


