Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Zain ul Abidin*
Received: July 01, 2022; Published: July 15, 2022
*Corresponding author: Zain ul Abidin, Senior Registrar Plastic Surgery, Jinnah Burn & Reconstructive Surgery Center, Lahore, Pakistan
DOI: 10.26717/BJSTR.2022.45.007163
Objectives: To have an understanding of isolated cases of tuberculosis (TB) in upper limb.
Study Design: Case series.
Place and Duration of Study: Jinnah burn and reconstructive surgery Centre, Lahore from June 2018 to June 2021.
Materials & Methods: This is a case series including nineteen patients, in collaboration with the department of infectious diseases. All cases in which tuberculosis in upper limb was diagnosed were included.
Results: Ten patients were male and nine were females. Tuberculosis of nerves was found in one patient, of tendon sheath in two patients and of bones in four. Compound ganglion with tuberculosis was present in two patients. Most of the patients improved with anti-tuberculous therapy and physiotherapy. Debridement had to be done in three cases. No systemic source of tuberculosis was found in any of these patients.
Conclusion: Isolated tuberculosis is a significant entity and it should be considered when diagnosing unexplained presentations of upper limb.
Keywords: Tuberculosis; Upper Limb; Jinnah Burn & Reconstructive Surgery Centre Lahore
Pakistan is a diverse country with a population of 220 million in four provinces. Tuberculosis is a major public health issue, with an estimated 570,000 new cases in 2019 and 43,900 deaths [1]. Pakistan was among the eight countries that make up two thirds of the total global number of incident cases worldwide in 2019. Underdiagnosis and under-reporting of cases are main obstacles to end the disease. Pakistan also accounts for more than half of the people with tuberculosis who are missed globally, as difference between the number of incident cases and the number of people registered for treatment in 2019 [2]. Tuberculosis primarily involves lungs however, every organ system in the body can be involved. Extra pulmonary tuberculosis accounts for 19.3% in European Union and 18.7% in America [3]. The process of spread to extra-pulmonary organs is not completely understood, but three theories have been agreed. Firstly, bacterial spread as a late complication of lung disease; secondly reactivation of latent foci in an organ after hematogenous or lymphatic spread; thirdly extension from mediastinal lymph nodes [4].
Extra pulmonary tuberculosis makes up 20% of the cases. The most common extra pulmonary locations include lymph nodes, genitourinary tract, bone marrow, central nervous system and musculoskeletal system. In turn including bones, joint, bursas, tendons and synovium [5]. Tenosynovitis is the most common form of the disease in the hand. Advanced HIV patients are likely to have such as musculoskeletal manifestations [6]. Additional risk factors include traumatic conditions of joints and bones, immunosuppressive drug users (corticosteroids), rheumatoid arthritis, systemic lupus erythematosus, smoking, alcoholism and individuals with implants [7]. Tuberculosis in the upper limb presents as osteomyelitis in small bones or as infection of the digits additionally pain, swelling, stiffness joint effusion or carpel tunnel syndrome [8]. Classical symptoms such as fever, night sweats, loss of weight and anorexia are rarely seen [9]. Features are more frequent in the arms when compared to the lower limbs, and it more frequently involves the dominant limb. The volar side is found to be more affected than the dorsal, as well as the ulnar side compared to the radial. Late presentation may result in tendon rupture. Muscles and nerves resist infection [10]. After this brief introduction we found a series of atypical features in patients in our upper limb outdoors. Patients had unexplained swellings, numbness or joint pains. None of the patients had typical features of fever or cough.
After obtaining institutional Ethical Committee approval, data of all the diagnosed cases was analyzed for over a period of last 2 years (2018-2020). The study was conducted at Jinnah Burn & Reconstructive Surgery Centre Lahore and was conducted in collaboration with the department of infectious diseases and department of Microbiology, Jinnah hospital Lahore. All cases in which tuberculosis in upper limb was diagnosed were included. Record was maintained in proformas. Patients presenting in OPD were clinically assessed, after taking detailed history. Radiographs of the affected region were taken, blood counts, liver function, renal function were performed. After taking all differential diagnoses into account, patients were admitted. Initially the suspicion for isolated tuberculosis of upper limb was so low that diagnosis of tuberculosis was kept as one of exclusion. But once the trend was noted in two patients with isolated swelling of hand and upper limb which turned out being tuberculosis on histology and microbiology, the thresh hold for suspicion was kept low and any case with an unexplained swelling, pain or ulcer in hand and upper limb was worked up in terms of tuberculosis.
Cases were discussed with the infectious disease department for starting pharmacological treatment. After the diagnosis of tuberculosis was confirmed, all patients were worked up for foci of disease elsewhere in the body by Chest x-ray, bone scans, additionally ESR, PCR and mountoux test was done. On monthly bases blood counts, ESR and PCR were serially repeated to assess the response of disease to medical therapy as well. The duration of therapy was decided by mutual understanding of infectious disease and microbiology department and was recorded in each case, roughly it was 6-8 months for soft tissue involvement and for bony involvement 12 month. Surgical debridement and debulking was only performed in cases in which the microbiologists and infectious disease physicians believed that reducing the disease burden will help in getting a better control of disease by medicines. Physiotherapy was carried out by the in-house Physiotherapy department. It was started on the day next to surgery, that was either tissue biopsy or debulking, as per our hand rehab protocol and also on the nature of symptoms. The therapy was continued till the patient felt he or she had enough return of function our enough relief of symptoms to carry out every day activities of life. Most of the patients improved with anti-tuberculous therapy and physiotherapy postoperatively. All the patients were kept in follow up till they were declared disease free by physicians and their hand function was returned to normal. All patients were advised physiotherapy depending upon the area of upper limb involved and the nature of procedure performed, postoperatively. Functional improvement was evaluated in follow ups.
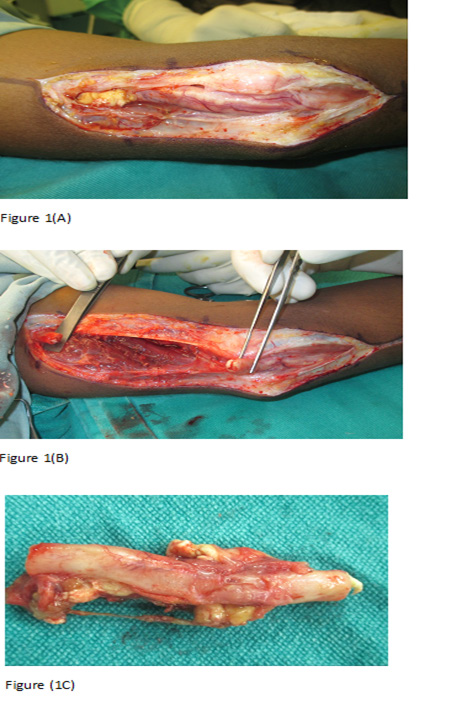
The mean age of patients presented was 35.8 years ranging from 21 -52 years. Males were 5 while 4 were females. Tuberculosis of soft tissue, nerves was found in one patient. Infected tendons were found in two patients. One patient had extensor tendons repaired (zone VI) previously. It was re-explored, debrided and ATT started afterwards (Figures 1 & 2). Another patient had swelling and decreased function of her right ring finger which she developed in her pregnancy. It was suspected to be tendinitis upon ultrasound and radiographs. Exploration and debridement of the finger was performed and ATT started after fluid cytology and histopathology reports were discussed with infectious disease department Two females were found to have compound ganglion with tuberculosis. One of those presented with swelling and decreased range of motion in her left wrist, palm and index finger. Compound ganglion was suggested on MRI which was confirmed by tissue biopsy. Antituberculous regime was started but when no improvement was observed, it was explored. ‘Rice bodies’ were found per operatively (Figure 3). The region was debulked and ATT continued for 1 year (Table 1).
Figure 1:
A. Inflamed ulnar nerve in distal arm, elbow and proximal forearm region.
B. Distal and proximal Ulnar nerve ends after excision showing caseation.
C. Excised ulnar nerve showing inflammation and caseous material at ends.
Tuberculosis of bones were found in four patients. Lesions were found in carpal bones in one case and in metacarpals in another. Distal radius was found to be involved in one patient, and was a patient with lesion of mid shaft humerus. One patient had previously taken anti-tuberculous therapy for pulmonary TB and later developed the lesion in distal radius. Another patient was later found to have TB in spine on bone scan who later developed lesion in metacarpal bones. None of the other 7 patients showed any systemic disease. In 6 out of 9 cases, the disease involved the dominant upper limb showing a preponderance for the dominant side.
Infection of mycobacterium tuberculosis occurs via inhalation into the respiratory tract. If the mycobacterium escapes expulsion function of mucocilliary system, or the subject is immunocompromised acquired, the mycobacteria reach the alveoli where they are phagocytosed by macrophages. Equilibrium between the inoculum and the quality of the host’s immune response results in formation of granuloma. Granuloma is an organized structure of different inflammatory cells, which encapsulates the bacteria in a hypoxic and highly acidic environment. Ultimately, the granuloma undergoes caseous necrosis. This caseous necrotic mass then undergoes gradual calcification. When granuloma formation is incomplete, liquefaction occurs, allowing the mycobacterium to spread contiguously to surrounding tissues. Sometimes the liquefying granuloma erodes into a blood vessel resulting in blood borne spread of the bacillus, with seeding in sites outside the lungs. This is the mode of spread by which extra-pulmonary TB occurs [11].
In relevance to upper limb, tubercular tenosynovitis most commonly involves the flexor tendons of the dominant hand. Hand involvement is seen in 10% of patients with musculoskeletal disease, and dominant hand of the male population is affected common. Local findings at the time of exploration includes graunolomas, areas of fibrosis and classical ‘Rice Bodies’. The pathophysiology of ‘rice bodies’ associated with TB synovitis is interesting. Pimm and Waugh revised the history of rice bodies initially thought to be detachments of the synovial membrane or collection of fibrin exudates. In 1927, Rogers proved they are composed of tubercular material. The bodies are formed from synovial tubercle and are attached to the wall of the tubercular sac. Later, they seperate from the wall and appear similar to polished white rice. They contain an inner vague core of acidophilic material and an outer layer composed of collagen and fibrin. Rice bodies can be seen in other synovial disorders such as rheumatoid arthritis, and fungal infections, seronegative inflammatory arthritis and synovial chondromatosis [12]. Radiograph of local lesion is more or less normal, unless in an advanced stage when the chronic mass effect causes bony erosion. Ultrasound is affordable, easy and early non-invasive diagnostic modality which shows an increased volume of synovial tendon sheath and a fluid collection. MRI is gold standard investigation because of excellent soft tissue demarcation. T2-weighted images gives an outline of fluid content inside synovium with a mixed solid cystic appearance. Gadoliniumenhanced imaging can also be done. Histopathology of synovial tissue shows granulomatous lesions with caseation surrounded by multiple giant and epithelioid cells [13].
Management of such cases involves multi-disciplinary approach. It involves input from infectious disease specialists, radiologists and reconstructive surgeons. Surgical treatment is done where it is thought that alone medical treatment would improve the condition of the patient. Additionally, it is done in cases of neuropathies [14]. Additionally, surgery avoids complications such as spontaneous tendon rupture and possible functional limitations. Synovectomy with removal of all rice bodies was the treatment of choice in the cases reported by us, followed a three-month interval for definitive reconstruction. A study suggested surgical debridement with excision of involved synovium and irrigation along with anti TB medication regimen for 12 months [15]. In case when there is joint involvement, tuberculous arthritis is generally a monoarticular disease that typically involves the spine or large and medium-sized joints. Moreover it must be differentiated with rheumatoid arthritis On the other side, rheumatoid arthritis (RA) is usually a symmetric polyarticular disease with commonly involves peripheral joints [16].
Along with conventional tests for detection of mycobacterium tuberculosis rapid molecular tests are also available. These are GeneXpert MTB/ RIF (Cepheid, Sunnyvale, CA, USA) and the Reverse Hybridization Test on strips Geno Type MTBDR plus (HAIN Life Sciences, Nehren, Germany). GeneXpert MTB/RIF is the only rapid molecular test recommended by WHO for the rapid diagnosis of tuberculosis. It detects presence of the Mycobacterium tuberculosis complex gene in specimens and the genomic sequences of the main mutations causing Rifampicin resistance. The reporting time is 2h. Extra pulmonary samples reveal the high sensitivity and the specificity of GeneXpert MTB/RIF for the diagnosis of extrapulmonary tuberculosis as compared to those found for pulmonary specimens. The sensitivity of the GeneXpert MTB/RIF vary in a series between 64.3% in pus samples and 100% in osteoarticular samples. The specificity was 64% in ganglion samples and 100% in osteoarticular samples. The sensitivity is low for soft tissue samples, they best show up on histological analysis [17,18]. Besides advances in the treatment of TB, the emergence of multidrug-resistant tuberculosis (MDR-TB) is a global concern. Pakistan is ranked 5th position in terms of a high burden of MDRTB in the world [19,20]. With this literature review we stress upon managing this entity in a multi-disciplinary setting.
Isolated tuberculosis is a significant entity. It is considered when diagnosing unexplained presentations in limbs. A prompt diagnosis of exclusion and treatment makes patient disease free.
Authors have no financial and personal relationships with any organization that could influence this work.


