Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Rama Musa, Raghad Laham, Rama Kam Nakach, Maram Askar and Ahmad Shoujaa*
Received: June 24, 2022; Published: July 08, 2022
*Corresponding author: Ahmad Shoujaa, Department of Biochemistry and Microbiology, Faculty of Pharmacy, Al-Sham Private University, Damascus, Syria, Email: a.s.foph@aspu.edu.sy
DOI: 10.26717/BJSTR.2022.45.007141
Diabetic retinopathy (DR) is one of the most common microvascular complication of diabetes mellitus, which leads to blindness in working-age individuals. Prolactin (PRL) is a peptide hormone mainly responsible for the function of lactation in mammals, but several studies have suggested that PRL has an important role in the prevention of DR. The target of our study is to investigate the potential role of prolactin in retinopathy. The study was conducted on 41 people and they were divided into 20 people as a control group and 21 people with type 2 diabetes (T2DM) as a case group, who were also divided based on retinopathy into two groups, the first 11 patients with diabetic retinopathy and the second group 10 without retinopathy. Serum PRL was measured by Enzyme-Linked Immunosorbent Assay (ELISA), HbA1c was measured by Fluorescence immunoassay. target Statistical analysis was carried out using version 20 of the Statistical Package for the Social Sciences (SPSS), and the result was expressed as mean and percentage. The quantitative results were statistically analyzed using the T-test and the ANOVA test to compare between groups. In addition, Pearson’s correlation was used link between the study parameters and its variables. A probability value less than 0.05 was considered statistically significant at the 95% confidence level. The results showed the lack of statistical differences between groups for prolactin. This study concluded that serum prolactin does not play a protective role in DR.
Keywords: Diabetic Retinopathy; Prolactin; Vasoinhibin; VEGF
Abbreviations:: ELISA: Enzyme-Linked Immunosorbent Assay; PRL: Prolactin; DR: Diabetic Retinopathy; DMO: Diabetic Macular Oedema; MMP: Matrix Metalloproteinases
Noninsulin-dependent diabetes or adult-onset diabetes which is currently known as T2DM occurs as a result of peripheral resistance to the hormone insulin or insufficient amount of insulin produced by the pancreas (relative rather than absolute deficiency), it represents 90-95% of all diabetes [1]. Diabetic retinopathy (DR) is a diabetes complication that affects eyes. It’s caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (retina) [2] and primarily leads to visual loss through proliferative DR (PDR) and diabetic macular oedema (DMO) [3,4]. hyperglycemia leads to damage to the endothelial cells of the retinal capillary, which leads to an increase in the permeability of the blood vessels of the retina, and this causes exudates, intraretinal hemorrhages and capillary closure, which leads to hypoxia, and as a result, the vascular endothelial cell growth factor) VEGF) is produced, which stimulates the formation of new blood vessels that extend into the vitreous, which causes fibrosis, vitreous haemorrhage and finally loss of vision on account of retinal detachment [5]. PRL (The pituitary hormone Prolactin) has several functions in immune response, reproduction, growth, osmoregulation, brain function, energy metabolism, and behavior. But current studies are interested in PRL, which is likely to have a prevention role against DR [6]. The studies have revealed that vasoinhibins caused by the proteolysis of PRL is a multi-function peptide, which was vasoconstrictive, antivasopermeability and antiangiogenic actions which gives vasoinhibins a role in protection from the complications of diabetes on the eye [7]. Proteolytic cleavage of PRL by several endogenous proteolytic enzymes, namely bone morphogenetic protein-1 (BMP- 1), cathepsin D and matrix metalloproteinases (MMP) [8]. The retinal vasoinhibins likely derives from PRL synthesized in the retina and from systemic PRL that reaches the eye via its receptors in the ciliary body [6].
This descriptive analytical case-control study was carried out in Syria from November 2021 to January 2022 at Al Zahera Medical Center. The sample size was calculated on the basis of a review article by Charan J and Biswas T. [9] using the formula for case-control studies, quantitative variables. Forty-one subjects were included in this study, classified as 20 healthy males or control and 21 T2DM male as cases. The case group included diabetic patients with DR (11) and diabetic patients without DR (10). The proportion of patients with T2DM treated with insulin is 9.52%, oral hypoglycemics 66.66%, combination between insulin and oral hypoglycemics 9.52% and untreated 14.28%. Patients with prolactinoma, chronic kidney disease, thyroid disorders, liver disease and female subject were excluded from the study. The study had been approved by the local ethics committee of AL- Sham private University. Data was collected using a structural interviewing questionnaire, which was designed to collect and maintain all valuable information concerning each case examined. A 6 ml of venous blood was collected by safe aseptic procedures. For HbA1c, 3 ml of blood was collected in EDTA anticoagulant container and stored at 6oC until the analysis; for prolactin 3 ml of blood was placed in plain containers; blood was allowed to clot at room temperature, then the sample was centrifuged for 3 min at 4000 rpm and the serum separated. Serum samples were stored below -20oC. At the time of analysis, samples were thawed and mixed before assay.
Serum PRL was measured by Enzyme-Linked Immunosorbent Assay (ELISA) (Pioway Medical), HbA1c was measured by Fluorescence immunoassay (Finecare).
Statistical analysis was performed using Software Statistical Package for Social Sciences (SPSS) version 20. The result is expressed as mean, SD and percentage. Quantitative results were analyzed statistically using independent samples T-test and One-Way ANOVA test for comparison between groups, Pearson’s correlation was used to correlate between the study parameter and study variables. p-value less than 0.05 was considered as statistically significant at 95% confidence interval.
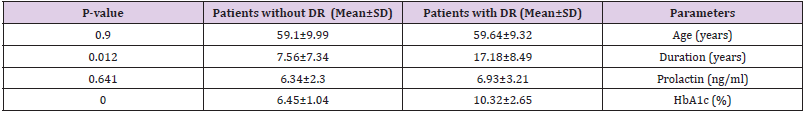
The age of the patients in the research sample ranged between 40 and 71 years. Samples taken from the research sample were analyzed to measure the average level of PRL (ng/ml) and the average level of HbA1c (%). The results were also statistically analyzed and the data were represented in the form of an arithmetic mean (standard deviation, percentage). Table 1 contains a descriptive summary of the study variables (age (years), duration (years), HbA1c (%), PRL (ng/ml) and the highest and lowest value of these variables. Table 2 about comparison between the case groups (patients with DR and patients without DR), there is nonsignificant increase in the mean level of PRL in patients without DR in comparison to patients with DR (p-value 0.641) where the mean level of PRL is 6.93± 3.21 in patients with DR and 6.34 ± 2.3 in patients without DR. Table 3 explains the correlation between PRL level and variables of study in patients with DR, there is no correlation observed between patients age and PRL levels (R =-0.181134, p =0.594), there is no correlation observed among HbA1c and PRL levels (%) (R =0.380935, p =0.248), the correlation analysis also indicated no correlation between duration of diabetes and PRL levels (R -0.317125, p = 0.342).
Table 2: Shows a comparison between Age, HbA1c, Duration and Prolactin level among the DR and without DR patients within the case group.
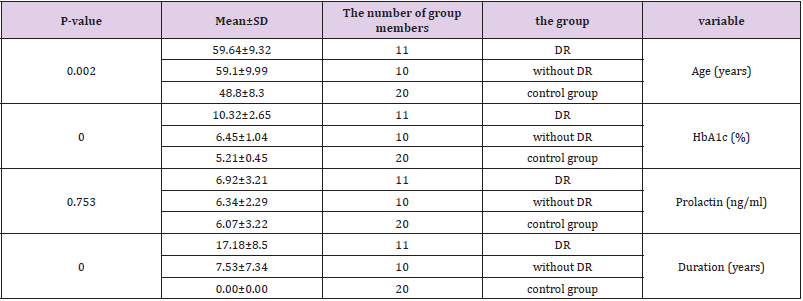
In addition, PRL was compared with other study variables in patients without DR as shown in Table 4 and there is no correlation observed between patients age and PRL levels (R =-0.395138, p = 0.258), no correlation between duration of diabetes and PRL levels (R = 0.096493, p = 0.791). The analysis of correlation also indicated no correlation between HbA1c (%) and PRL levels (R = 0.211691, p = 0.557). Table 5 shows the results of ANOVA test for the three groups (patients without DR, patients with DR and control group) , There was a non-significant difference between the three groups in prolactin level (P-value= 0.753). There was a significant difference between the three groups in terms of age (P-value=0.002) and Duration (P-value=0.000) and HbA1c (%) (P-value=0.000).
Table 5: The results of the analysis of the ANOVA test for the three groups (control group, patients with DR and patients without DR.
There is no relationship between the level of serum prolactin and diabetic retinopathy in Syrian patients with T2DM, this may be due to that the effect of prolactin differs from vasoinhibins (derived from prolactin hormone), which has properties antivasopermeability and antiangiogenic. The present study found that there is no relationship between duration and prolactin, and this agree with the study done by Malaz S, et al. [10], who concluded that there was no relationship between the duration and the level of prolactin. Also, the current study resulted that there is no relationship between HbA1c and prolactin, and this is in agreement with Malaz S, et al. [10], who reported no correlation between PRL levels and HbA1c, this is probably because the role of prolactin in regulating blood sugar is not proven in humans, due to the lack of knowledge of the roles of prolactin that are really relevant to humans.
The study concluded that there is no relationship between age and prolactin level, and this agree with Malaz Salah, et al. [10], who concluded that there was no relationship between age and PRL level, this may be because PRL is primarily regulated by dopamine and a negative feedback mechanism which not related to age. In addition, the study found that There is no difference in the level of PRL in the case group (between patients with and without DR), and this disagree with Malaz Salah, et al. [10], who reported that PRL has a protective role against DR, Perhaps because we conducted the study on a smaller number of samples. Also agrees with Medhat AbdelMoneim, et al. [11], and Bonakdaran Shoko, et al. [12], who reported that the PRL does not have a protective role against diabetic retinopathy. Finally, disagrees with Jakob Triebel, et al. [13], who developed a new technique to measure vasoinhibins levels in the serum samples of DR patients and compared it with a control group and reported that an inverse relationship between systemic PRL and development of DR, the reason may be that they analyzed vasoinhibins while we analyzed PRL. We conclude that Serum PRL does not seem to have protective role in DR in syrian population. In the further we need to assess the levels of vasoinhibins in syrian, and conducting clinical trials to evaluate the role of vasoinhibins as a preventive treatment against DR.
We thank Dr. Alaa Halima for her assistance in completing this study. We thank Prof. Sharif Al Ashkar, the president of Al-Sham Private University. We thank Dr. Khaled Alhomsi, Vice president of Al-Sham Private University. We thank Dr. Bassel Hussein, Scientific Vice Dean and Dr. Wael Alaghawani, Administrative Vice Dean of faculty of Pharmacy in Al-Sham Private University for their help and guidance.
No potential conflict of interest was reported by the authors.
This study was not funded by any institution.
The names and personal details of the participants were blinded to ensure privacy.


