Abstract
The main direction in the dentistry of future should be the prevention of dental diseases, and their treatment with minimal surgical intervention. The Chuiko Institute of Surface Chemistry was among first world developers of filled photopolymer compositions for dental prosthetics and filling [1-3]. All investigations traditionally focused on acrylic monomers and oligomers and went to replace conventional filling masses. Meanwhile, polyepoxides are a unique restorative material both in engineering and medicine (prosthetics, inventory, etc.). The possibilities of epoxy-composites allow expansion of their use on dental devices. In our new popular-science experimental publication, a theoretical substantiation of practical preventive and self-restorative methods in dentistry was carried out, thanks to the use of epoxy-compositions with nano-silica, nano-alumina, and nano-micro-sized mineral fillers. These hypotheses found confirmation in the obtained results of dental repair & follow-up observations on the treated groups of volunteers. All these assumptions and hypotheses found confirmation in the obtained results of observations in the of affected teeth of patients was controlled by visual (photo, x-ray image) and well-being comparative information during test period. As a result, the existence of highly filled epoxy-mineral compositions capable of filling and restoring lesions and mechanical damage to teeth, independently and outside of clinical conditions, is shown. The tooth powders and epoxy-composites from cheap available components, for use by non-specialists in domestic & non-clinical conditions – were developed and proposed. These results will be very useful for people and communities who, for various reasons (wars, out-cities, voyages, poverty, workload), are temporarily or regularly left without access to quality dental services.
Mini Review
We all know this unfortunate situation: the toothache (it chipped, fell out, became hypersensitive) just for the weekend or on a voyage There is no time to treat him in the coming weeks... Your dentist was on vacation, in the next turn for 3 days, and in private dentistry a filling is expensive… In the nearest district clinic, the dentist did not want to treat the “hopeless case”, and wrote out a referral for removal to the surgeon ... Queues, uncertainty, spending money ... These troubles, familiar from childhood, haunt most people all their lives, right up to old age. Subsequently, you have to pay for implants, dento-bridges, crowns ... but they bring new problems - prolapse, gums-inflammation, bad bite ... Is it really supposed to be like this forever, and our teeth will be such a “5th column” for us all our lives, on which we should keep a constant guard familiar dentists and a separate wallet? Or try not to reckon and endure all disorders, caries, gumboils, and irritation of the teeth? This is also not a solution, but a path to tooth loss at 40-45 years old. But it shouldn’t be like this forever. The progress of biomedical and technical research will help to solve this problem, analogically to skin or and bone diseases. From ancient times until the 1940s-60s, people were horrified by any cuts, bites and punctures of the skin. At every step they were threatened then by gangrene, tetanus, malaria, rabies, blood poisoning and other (long forgotten by us) diseases going through the blood. And more recently, in medical institutions one could see posters with recommendations to immediately go to the “emergency room” after the initial treatment with iodine or formalin at the site of a cut or bite. But does anyone do this today - in the era of Panthenol, Iodoform, BF-6, medical cyanoacrylates, and solution of “Brilliant Green”? And now, in the 21st century, does anyone run to the ambulance after being bitten/scratched by a street cat, a tick, or even a dog (not to mention mosquitoes, bees and wasps)? This is a fact - 95% of people have learned to heal skin damage that has recently threatened with terrible consequences – personally by own hands, with the latest and very effective cheap ointments and sprays. So, medicine has solved similar problems in related fields. This applies to biomedicine in general, in almost all of its areas. For half a century, medicine and prophylaxis have taken cardinal steps forward. If back in the 1930s and 1950s epidemics of cholera, measles, diphtheria, malaria, and even typhoid and plague were considered normal, now we don’t even mention them.
However, Dentistry and Dental Diseases are More Conservative
Their methods are still somewhere in the 1930s ... except that the drills are not so painful and noisy, the chairs are more beautiful, the anesthesia is better, and fillings are more durable. But this is not a breakthrough, but only an improvement on traditional methods. Dentistry has also experienced a rebirth, with emergence of new polymeric materials. From the 60’s and 70’s. began the widespread introduction of polymer cements, and from the late 80s - photopolymers. Now, highly filled, fast curing dental polyacrylates have been brought to perfection. And up to now the quality of these materials is constantly improving. Obviously, a typical medical inertia and often political processes have stood in the way of progress in dentistry. In particular, mass practical dentistry remains on the foundation of the methods of the 1940s and 1950s, according to which the treatment of caries remains a nerve-, time-, and money-consuming procedure - and often with side effects and complications. The reforms of medicine in the post-Soviet period led to the curtailment of mass free (and good) polyclinics of the times of the USSR, and their replacement with paid ones (often with a dubious effect) - especially in the field of dentistry. At the same time, such paid private points are a rarity in the regions.
The Chuiko Institute of Surface Chemistry of the National Academy of Sciences was among the first institutions in the world to create its own Laboratory of Biocompatible Materials. It developed some of the first in the USSR and the world photopolymer highly filled compositions for prosthetics and filling, recorded by a number of articles, patents and dissertations [1-3]. Accordingly, the Ukrainian SSR and then Ukraine became the workplace for the first introduction of both innovative brakes of photo-polymerizators (Sakura, Polident) and photopolymer dental pastes (Oxomat, Stomadent, Esta, etc.). All of them focused on acrylic monomers and oligomers and went to replace conventional filling masses. At the same time, in our opinion, the main direction in the development of dentistry of the future should be the prevention of dental diseases, and their treatment with minimal surgical intervention. We already have a positive experience in creating therapeutic prophylactic powders for damaged teeth [4-5]. However, work on the creation of epoxy composites for fillings represents a new special cycle, which has no analogues in the scientific literature so far.
One Drawback of Dental Materials Science Should Be Pointed Out
Since first investigations in 1980-90 s, it has followed the path of using polyacrylates - toxic substances, which however, were allowed for fillings and prosthetics. Many other polymer matrices, in particular polyepoxides, were not considered then, apparently due to their “bad image” as technical and eco-suspicious materials. Indeed - for example, epoxy hardeners are toxic. However, in polyepoxides, they are completely polymerized to an eco-friendly plastic. Acrylic monomers and oligomers do not always harden by 100% (for example, photopolymers), and subsequently the products of underhardening come out of the filling directly into the oral cavity (which sometimes causes sensitivity of the gums and only filled teeth, as well as headaches). The first polyacrylic dentofillings allowed headaches, gum disease and other reactions to the release of uncured components into the mouth. Now the quality of dental polymeric compositions has improved, but…the nature of monomeric acrylates and esters remains unfriendly to health. Even in smell-tests, comparisons of acrylic (pungent bad odor) and epoxy (odorless) resins are in favor of epoxies. Of course, “both they are all unnatural chemical synthetics”, but whoever sniffed acrylic oligomers (resins for dental polymers) - will no longer want to be in the same room with him. Epoxy resins are odorless, and that’s worth something. Of course, technical resins (including those sold in supermarkets) have a poisonous hardener (polyamines, less often anhydrides or sulfur-containing substances). But it’s all polymerizing to plastic mass. Meanwhile, polyepoxides are a unique restorative material both in engineering and medicine (prosthetics, inventory, etc.).
The possibilities and open new properties of epoxy composites are far from being exhausted and are constantly expanding. Finally, polyepoxides (with the right filling and curing technique) turn out to be a unique material for filling and restoring teeth - even without a dentist and outside of clinical conditions! It is necessary to know how and when an epoxy compound becomes an effective «cold weld» for a wet and moving surface. Another “negative” against polyepoxides is that they do not like water and wet surfaces. But acrylates don’t like them either. That is why costly and even painful procedures for drying reamed teeth with compressed air (quite aggressive for dentin irritated). Our experiments have shown that with a special curing epoxy resin is resistant to moisture, and even on the aquatic environment. It’s all about aging - after holding the mixed composition for 2-3 hours until it thickens (if it’s not hot, otherwise you need to act faster), it can be safely used as a «putty» for dental chipping or as glue for gluing a fallen crown or part of a tooth. Of course, before that, you need to rinse well, disinfect and (preferably but not necessary) dry the place of application a little (for example, biting a napkin - like a tampon at a dentist).
The Results of Experiment
The first experiments on non-clinical (including self-tested) filling and gluing of chipped teeth were carried out. For work, an epoxy composition was used: Epoxy520+ resin, fresh PEPA hardener (5:1), filled with 65% gypsum and white cement (gives a nice “dental” color but can be replaced with ordinary grease\black cement). After adding the hardener, the composition was kept for 3+-0.5 h - until a semi-solid consistency with high stickiness. After that, for 30+-10 min the composition was still suitable for strong adhesion (within 1-2 min) with a wet tooth surface. In all cases, priming of the tooth surface was not carried out (since the priming composition of the same composition for the most part turned into a weakening layer). Tooth surface preparation was also simplified to a series of rinses, followed by a soft brush with nano-silica (or another desiccant) and a swab snack. The filling (or crown) was applied immediately after such drying, with a certain pressure and holding for 1-2 minutes. After that, the patient personally selfcorrected the bite and the shape of the filling or the glued part of the tooth. Subsequently, for 3-7 hours (including for a night’s sleep), the operation site remained at rest, and only self-corrections of the bite and shape were carried out (and the separated parts of the glue were also removed).
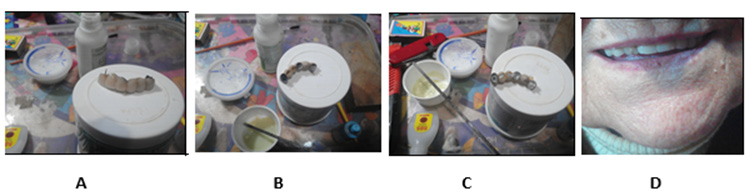
As a result of the tests, it was found that these compositions can effectively glue the fallen fragments of dental crowns, artificial jaws, or teeth (Figure 1). In the future, they hold well in this position and withstand all loads.
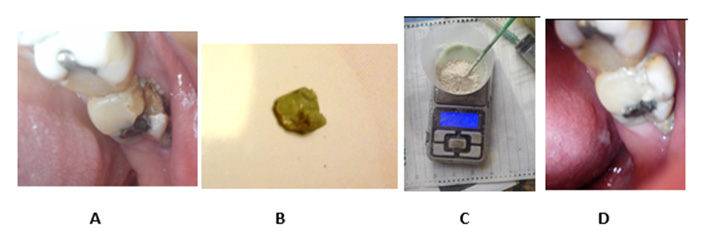
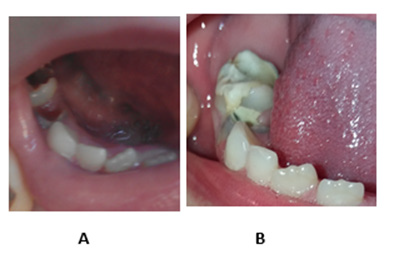
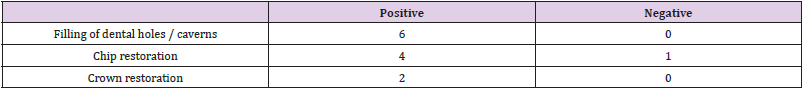
They are no less effective when gluing fallen fragments of living teeth - for example, broken or broken ones (Figure 2). At the same time, the preparation procedure is simplified as much as possible - since it is limited to simple pre-rinsing and wiping the place of gluing (sealing) with a light antiseptic. These restorations may require repeating the gluing procedure (under non-optimal operating conditions or errors in the post-curing process in the mouth), after which the composite is firmly embedded and well withstands dental loads for many years (Figure 2). It is effective to use these compositions in home and family conditions for the restoration of damaged children’s teeth (Figure 3). At the same time, an important problem is solved - the fear (or even panic) of the child in the doctor’s office. (Figure 3) shows an example of a completely destroyed tooth 4 and a severely affected molar 5. They were not accepted for treatment by any doctor and were sent for urgent removal (because they were periodically sick). But after restoration at home (by our parents during our observation), the polyepoxy mass stood firmly on the affected surface. At the same time, the ideal bite-compatibility with the upper teeth was restored, respectively, the problem of chewing on the left side of the jaw was solved. Such an operation (Figure 3) has been successfully performed on the teeth of several patients. The effectiveness of these composites can be seen from (Table 1).
Figure 1:
A. The drop-down “crown” of an old patient, in the states – initial.
B. Prepared.
C. Smeared with the composition and
D. Inserted back.
Figure 2:
A. Damaged.
B. By a marginal chip of enamel.
C. And rejected for further treatment of the 7th tooth of a man; filling composition at the time of mixing the resin with the filler.
D. Restored tooth one month after the chip was glued back.
Figure 3: Shows examples of restorations implemented in 2020-2021 by our epoxy-composites.
A. Extreme milk teeth (molars) of a schoolgirl in a completely degraded (not accepted for treatment) condition.
B. And their appearance after a month of self-filling with our composition.
Table 1: The number of recorded effects according to the results of the first out-of-clinical restorations with epoxy composites.
Conclusion
1. On the basis of well-known analogies with the phenomena of self-rehabilitation in wildlife and in industrial and construction industries, the first foundations for the theory of dental selfhealing, while complying with a number of hygiene rules, and epoxy compositions with nano- and micro-fillers.
2. On the example of specific experimental works, the possibility of the existence of highly filled epoxy-mineral compositions capable of filling and restoring lesions and mechanical damage to teeth, independently and outside of clinical conditions, is shown. The resulting composites are generally available and harden in the conditions of the dental cavity into biocompatible polymer fillings of high strength and resistance. This allows them to serve for a long time on a par with commercial dental ambulances.
3. These results will be very useful for people and communities who, for various reasons (remoteness from cities, business voyages, poverty, workload, war), are temporarily or regularly left without access to quality dental services.
References
- D Starokadomsky, N Shklovskaya, V Makeev (1995) Photopolymer filled compositions for dentistry. Dentistry News (Novosty Stomatologji, In Russian) 1: 40-45.
- DL Starokadomsky Influence of highly dispersed pyrogenic silicas on the processes of photopolymerization of oligoetheracrylates and properties of the obtained stomatologic composites. Thesis of Dissert. for Dr Chem Sci (Kyiv: Chuyko Institute for Surface Chemistry, National Academy of Sciences), pp. 200.
- D Starokadomsky, TN Solov’eva (2002) Effect of silicon oxide fillers on photochemical curing of compounds based on acrylic monomers and oligomers. Russian Journal of Applied Chemistry 75(1): 138-141.
- D Starokadomsky, M Reshetnyk (2021) Restorative Сapabilities of Dental Powders Based on Composiitons Nanosilica Asil A-300 + Herbal \ Mineral Powders in the Prevention or Delay of Caries and Dental Diseases. Biomed J Sci & Tech Res 36(4): 28705-28714.
- D Starokadomsky, M Reshetnyk, V Antipova (2021) Possibilities of compositions pyrogenic nanosilica + nano-Al2O3 + plant/herbal dispersions for prophylaxis, self-restoration and delay in the development of carious & near-dental pathologies. J of Environmental & Earth Sci 7(10): 7-15.

 Mini Review
Mini Review