Abstract
The commonest sites of distal colorectal cancer spread are the liver and the lungs. Metastesis to the skin, breast and axilla are very rare. Very little data exists regarding the optimal treatment methods and its long-term outcomes. We present a unique case of colorectal cancer patient who initially presented with solitary hepatic metastesis, subsequently underwent low anterior resection with synchronous resection of the hepatic mets after neoadjuvant chemotherapy. At one year followup, she developed a cutaneous, mets to right lateral chest wall and treated with wide local excision and adjuvant therapy. At four years of follow up she again develops metastasis to the right breast and axillary lymph node. Wide local excision of the breast lump and axillary lymph node dissection were performed. Despite recurrent metastesis the patient has maintained a good functional status. A literature review was done to highlight the best treatment options in these rare cases.
Keywords: Colorectal Cancer; Rare Site Metastasis; Mets To Breast; Axilla and Skin
Introduction
Hellman and Weichsel Baum first proposed the theory of oligometastasis in 1995. This concept recognizes that in some cancer patients, a limited number of metastases may suggest improved patient outcomes with local removal [1]. Thus, the traditional view of metastatic disease has changed, with treatment now aimed at cure, instead of prolonged survival or palliative care in some cases of metastatic disease. Perhaps the most common malignancy to undergo such a significant alteration in treatment is that of colorectal cancer. Metastases to the liver and lung can now be considered amenable to local resection or ablative therapies. Colorectal carcinoma is globally the third most common malignancy diagnosed each year. In the united states, 15-20% of patients have metastatic disease at the time of diagnosis. Modern systemic therapies have helped to improve the survival for such patients with nearly 20% surviving up to five years beyond diagnosis [2]. Published data has demonstrated that surgery can provide a cure in cases of isolated metastases and, when combined with systemic therapies, can also improve long-term survival in cases where metastases involve more than organs [3]. However, much of this data is centered around metastases involving the liver and lung, as these are the commonest sites of distant colorectal cancer spread. Metastesis to the skin, breast and axilla, however, are far rarer and there is very little data regarding the optimal treatment strategy and long-term outcomes, even in cases of isolated lesions. The case presented here describes the clinical history of a lady diagnosed with primary colorectal carcinoma with a solitary hepatic metastasis. One year after undergoing intended curative treatment, she developed cutaneous, right breast and axillary metastases, each of which were treated with aggressive local resection. Despite this, she has maintained a good functional status with isolated recurrences at four years from her initial diagnosis. The discussion is based on the approach to best treatment in such rare cases: whether aggressive surgical resection should be sought in favour of limiting options to systemic palliative therapy alone.
The Case
A 55-year-old female, presented to the outpatient breast clinic
for evaluation of right sided breast and axillary lumps which she
noticed nine months prior and were increasing in size. She reported
no breast pain, skin or nipple/areolar complex changes or nipple
discharge over this period. She experienced menarche at 14 years
old and was nulliparous, still experiencing regular menstrual
cycles. She had never used oral contraception or hormone
replacement and had no significant family history of breast or
other malignancies. The patient had a complex past medical history,
which included hypothyroidism treated with levothyroxine and
Hodgkin’s lymphoma treated with chest wall radiation 25 years ago.
At that time, complications of treatment for her lymphoma included
a frozen right shoulder as well as a right upper limb deep vein
thrombosis. More recently (4 years prior to this presentation), she
was diagnosed with an adenocarcinoma of the rectosigmoid colon
with a solitary hepatic metastasis at segment 6. She underwent
neoadjuvant chemoradiation followed by a low anterior resection
and synchronous resection of her liver metastasis. She completed
adjuvant chemotherapy but subsequently developed a solitary
metastatic skin lesion at the site of her previous liver marker
placement at the right lateral abdominal wall. This was treated with
wide local excision and further systemic chemotherapy. Surveillance
colonoscopy and computed tomography imaging showed no
evidence of disease recurrence up to the time of presentation. The
patient was a non-smoker and was functionally independent, but
had limited right shoulder mobility.
At examination, the patient’s vital signs were within normal
limits with no signs of dehydration, anaemia, malnutrition
or jaundice. Abdominal and rectal examinations showed no
abnormalities. Breast and axillary examinations revealed a 3 cm
firm, mobile mass in the axillary tail of the right breast with an
associated 2 cm firm palpable right axillary lymph node (Figure 1).
Complete blood count, renal, liver and thyroid function tests were
within normal limits. Ultrasound imaging confirmed the presence
of a 2.2 cm solid, heterogenous mass at the upper outer aspect
of the right breast, along with a 2 cm right axillary lymph node.
Mammogram reported the presence of two enlarged, hyper dense
right axillary lymph nodes, classed as BIRADS 5 lesions (Figure 2).
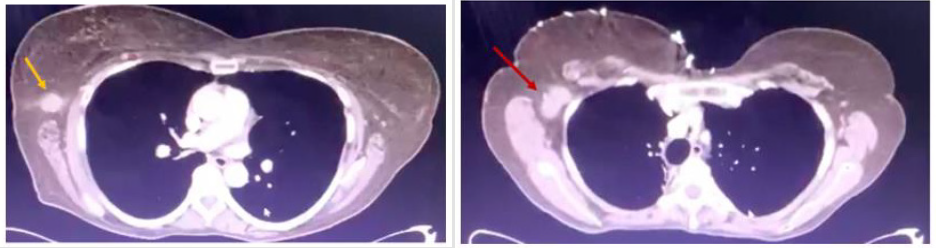
CT confirmed the presence of a 2.6 cm spiculated lesion in the right
upper outer breast with associated level I axillary lymphadenopathy
(Figure 3). No other metastatic lesions were identified on CT.
Positron Emission Tomography (PET) scan was not accessible to
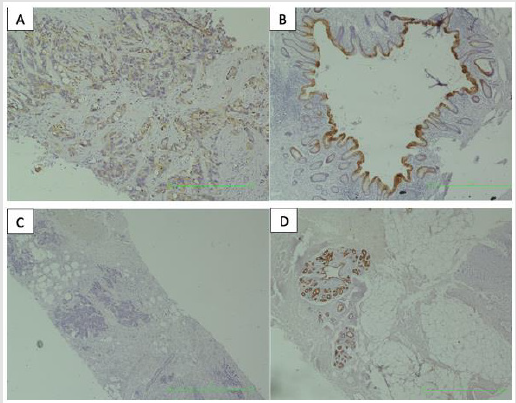
assess for other possible metastases. Core needle biopsy confirmed
the presence of a metastatic colon adenocarcinoma within the
breast and axillary lymph nodes, with tumour cells staining
positive for cytokeratin CK20 (Figure 4). A joint decision with the
patient was made to perform a wide local excision with axillary
lymph node dissection. Under general anaesthesia, the patient was
placed supine with the right shoulder abducted to ninety degrees.
A cutaneous nodular lesion on the axillary skin was noticed at the
time of surgery and this was excised under suspicion of a possible
cutaneous metastasis (Figure 5). Through the same incision, a
wide local excision of the breast lesion was performed with gross
margins at least 1-2 cm and axillary lymph node dissection was
completed to include levels I and II nodes. The thoracodorsal and
long thoracic nerves were identified and preserved. A drain was
inserted and the wound was closed in two layers. The patient had
an uneventful recovery with no significant change in her shoulder
mobility immediately after surgery. She was discharged home on
post-operative day one with subsequent follow up at the clinic.
Figure 1: Image showing right axillary tail mass and associated axillary lymphadenopathy (encircled).
Figure 2: Craniocaudal (left) and mediolateral oblique (right) mammogram images demonstrating suspicious, enlarged right axillary lymph nodes (yellow arrows).
Figure 3: Axial CT images identifying a suspicious lesion within the axillary tail of the right breast (yellow arrow) and a suspicious, enlarged right axillary lymph node (red arrow).
Figure 4: Microscopic appearance of the patient’s breast biopsy, staining positive for CK20 (A) with control (B) and negative for CK7 (C) with control (D).
Figure 5: Pre-operative image showing right breast lesion (yellow arrow), cutaneous nodule (red arrow) and site of excision of previous abdominal cutaneous metastasis (white arrow).
Discussion
Colorectal carcinoma is the third most common malignancy
diagnosed around the world with a lifetime risk in developed
countries as high as 4% [2]. In the Caribbean, this disease ranks
among the top five leading cancers diagnosed annually in both
males and females. Warner et al reported incidence rates of almost
11% and 3% for colon and rectal cancers respectively in Trinidad
and Tobago between 1995 and 2009. They also reported that over
10% of most cancers in Trinidad and Tobago (including colorectal)
were diagnosed at advanced stages, which highlights that tumour
biology in this region may be particularly aggressive or that cancers
are not diagnosed early enough [4]. Cancer metastasis is a complex
multi-step process by which cancer cells acquire certain properties
that allow them to move from the primary tumour and invade a
distant organ. They do this while maintaining the ability to survive
and travel within the body (directly entering the bloodstream or
indirectly via lymphatic’s) . Some circulating tumour cells are
postulated to remain dormant while maintaining the ability to grow
and this is thought to be one of the contributing factors responsible
for the development of metastases after a primary tumour is
removed [5]. The patient in the case presented here developed
rare distant metastases three years after undergoing treatment
with curative intent for colorectal carcinoma with a solitary hepatic
metastasis. Unlike skin metastases occurring in 24% of metastatic
breast carcinomas, data suggests that cutaneous metastases occur
in just 4% (2.3-6%) of colorectal carcinomas. They are mostly found
on the skin of the abdominal wall, especially at the sites of surgical
scars related to treatment of the primary tumour, as occurred in
this case [6].
Kauffman and Sina suggested that the pathogenesis of
cutaneous metastases in colorectal cancer occurs due to lymphatic
or haematogenous spread, spread along embryonic ligaments or, as
postulated in this case, by direct seeding of tumour cells during a
surgical procedure. Published data suggests cutaneous spread tends
to be identified within two years of undergoing cancer treatment.
It is usually thought to signify widely disseminated disease and
generally a poorer prognosis, with patient survival documented to be
an average of 18 months (1-34 months) [7]. Based on a small number
of case reports of this entity, recommendations suggest that single
cutaneous metastases should undergo wide excision with margins
at least 1 cm, as was performed in this case. This is in contrast to
cases of diffuse cutaneous metastases which are generally treated
by palliative systemic therapies [8]. Despite statistics suggesting
relatively poor survival outcomes, this patient has now survived up
to four years since her initial diagnosis. Although she has developed
rare distant organ metastases, they continue to be isolated to single
organs only. This has contributed to the decision to continue local
excisions in combination with systemic therapy with the intention
to improve her survival. Furthermore, the question of whether
this approach to her treatment may actually provide a cure is yet
unknown. Perhaps cure may not be possible in her case, as she has
continued to develop distant metastases despite being on systemic
chemotherapy. PET/CT, in our opinion, would have been beneficial
in identifying occult metastases not detected by CT and may have
helped to determine whether this patient was a candidate for
surgery or not. The use of PET scanning is currently recommended
by the National Comprehensive Cancer Network (NCCN) guidelines
in patients who appear to have potentially resectable or curable
metastatic colorectal carcinoma [9].
The most common primary tumours associated with breast
metastases include cancers of the contralateral breast, leukaemia,
melanoma, lung, ovary and stomach [10]. Distant metastasis of
colorectal carcinoma to the breast, however, is extremely rare,
with a handful of cases reported in the literature. Even rarer, is
the involvement of axillary lymph nodes as described by Perin et
al [11]. An analysis of 32 cases of this entity by Zhang et al found
that the majority (94%) occur in females at an average age of 51 years and at a time ranging from 1 to 10 years after initial diagnosis
of the primary tumour [12]. In the case presented here, for cancer
cells to reach the breast and axilla having had previous involvement
of the liver and skin, suggests that this patient’s disseminated
disease is particularly aggressive, with travel specifically along the
haematogenous and lymphatic’s. Imaizumi et al described possible
lymphatic spread via the thoracic duct or superficial lymphatic’s.
However, Kawamura et al demonstrated that the superficial
system may be more pertinent in the evolution of axillary lymph
node involvement as the abdominal wall superior to the umbilicus
drains upwards into the axillary nodes [13]. Unlike published
reports of involvement of the left breast in 55% of cases, this
patient’s metastatic lesion occurred on the right breast, but similar
to documented cases, her breast lesion was superficial, located in
the upper outer quadrant, was mobile and fell within the reported
size range (between 1 and 10 cm) [3] [12]. Shah et al described
certain clinical or radiological features that may distinguish
metastatic colorectal carcinoma of the breast from primary breast
carcinoma: location within the subcutaneous fat and not the breast
gland, rapid increase in size and lack of micro calcifications on
breast imaging. Features like nipple retraction and skin tethering
that are commonly seen in primary breast carcinoma are virtually
non-existent in metastases to the breast. Such distant metastases
of colorectal origin typically show mucinous or signet-ring features
with the presence of lymphovascular invasion and a lack of elastosis
or an in-situ component [14].
Immuno-histochemical analysis confirms the final diagnosis:
cells at these sites stain positive for colorectal markers including
cytokeratin 20 (CK20) and carcinoembryonic antigen (CEA)
and are negative for markers of breast origin (CK7, oestrogen/
progesterone receptor) [3]. The documented prognosis in cases
of metastatic colorectal carcinoma to the breast is generally poor,
with average survival rates less than 12 months from the time of
diagnosis [3] [12]. However, individual case reports suggest that
some patients may potentially achieve long-term survival. A case
report by Imaizumi et al documented a nine-year survival between
the time of initial diagnosis of colon cancer and axillary lymph
node recurrence, suggesting that tumour biology may influence the
metastatic potential in such cases [13]. Traditionally, the treatment
of metastatic disease is based on the pathogenesis and biology of
the primary tumour. From as early as 1894 Halstead proposed that
breast cancer spread via a contiguous pattern along lymph nodes
from the primary tumour ultimately to distant sites. More recently,
the systemic theory suggested cancer is a systemic disease process:
meaning that if a tumour is going to metastasise, it has already
done so. This theory remarks that cancer spread does not occur
in a contiguous fashion as Halstead proposed, but rather clinically
apparent lymph nodes are manifestations of already distant
metastasis. However, both these theories are limited in their ability
to fully describe cancer behaviour.
The systemic theory does not account for the existence of
intermediate disease states between localized and metastatic and
while the contiguous theory may cover this, it does not account for
the ability of cancer to spread through the bloodstream. Intensive
study of tumour biology since then has led to the understanding of
cancer behaviour, which lies on a spectrum ranging from localized
to distant metastatic disease. During the evolution of invasive
malignancy, tumour cells are now understood to acquire several
features which enable metastatic spread to occur in a multistep
fashion. This knowledge formulated the basis for Hellman’s and
Weichselbaum’s concept of oligometastases, which proposes that
the biology of a tumour predicts if its metastatic potential is limited
to specific regions. Tumour size and pathological grade are perhaps
the two most frequently used characteristics that may help guide
knowledge on a cancer’s oligometastatic potential. On the contrary,
this is vastly different from the term micro metastases, which
describes very small but extensive cancer metastases. Colorectal
carcinoma is one of the most commonly described malignancies
that can exist in an oligometastatic state. Successful treatment with
good survival outcomes is well documented, particularly in the
treatment of hepatic or pulmonary metastases [1].
An oligometastatic state theoretically puts forward the
possibility that malignant disease can be amenable to cure, with
therapies targeted towards treating both the primary tumour and
the limited extent of metastatic lesions. But, for treatment to be
effective, all metastatic sites must be identified and targeted. This
concept may be applicable to the case presented here, but still, the
existence of a true oligometastatic state remains controversial and
this view point is not shared by all clinicians. In metastatic colorectal
carcinoma, 40-70% of cases spread to the lymph nodes first but the
liver is often the first distant site of spread, due to drainage of the
intestine via the portal venous system [12]. Spread to the lungs can
occur via direct drainage of rectal carcinoma through the inferior
vena cava and thereafter other sites like the bones and brain may
become involved [2]. However, involvement of sites like the skin,
breast and axilla is extremely rare and may be associated with
particularly aggressive subtypes of colorectal carcinoma (BRAFmutant
cases for example) [15]. Therefore, the majority of the data
guiding the optimal approach to treatment in these cases is limited
to information provided by published case reports.
The successful treatment of colorectal cancer with liver or
pulmonary metastases is extensively described in the surgical
literature. With liver-only metastases, approximately 20-25% of
patients can achieve disease-free survival of over ten years [1]. The
role of a multidisciplinary team approach is crucial here to determine
the ideal treatment strategy for these patients, especially when
surgery can be combined with ablative therapies including systemic
chemotherapy, radiofrequency or microwave ablation or intraarterial
chemotherapy among others. The National Comprehensive
Cancer Network (NCCN) recommends that patients with resectable synchronous liver and/ or lung metastases can undergo resection
and/ or local ablative therapies, although resection is preferred [9].
In colorectal cancer with isolated pulmonary metastases amenable
to treatment with curative intent, surgical resection can lead to fiveyear
survival of 45-65% [1]. However, the treatment of metastases
to the breast and axilla is complicated and the selection of the
optimal strategy depends on the primary tumour, involvement of
other sites and the overall condition of the patient. Barthelmes
et al suggested against surgical excision in these cases due to the
underlying disseminated state of disease, predicted short life
expectancy and the risk of tumour seeding onto the skin [10,16].
Others, like Fernandez de Bobadilla, suggest that excision can
help to achieve local control of disease and prolong survival when
combined with systemic chemotherapy [17].
Because of the rarity of this phenomenon, however, there is no
high level evidence supporting an ideal approach and this decision
is often made on a case-based approach [12]. In the case described
here, the decision to proceed with surgical excision of isolated rare
distant metastases was influenced by the fact that the patient had
approached four-year survival with isolated metastases only and
maintained a good quality of life despite this. She will continue to
be surveyed for future metastases as well as her overall outcome.
Conclusion
Systemic therapies are standard aspects of treatment of various metastatic malignancies and traditionally were the only options for treating metastatic colorectal carcinoma. However, modern advances in science and technology have allowed improved survival and in some cases, cure, for select patients with metastatic colorectal cancer. This has been clearly demonstrated in cases of metastases to the liver and lungs, but metastases to the skin, breast or axilla are so uncommon that there is currently no general consensus regarding the best treatment options for these patients. Treatment decisions here are often made based on multidisciplinary discussions and information derived from published case reports or series. A decision to perform excision or provide systemic treatment of isolated metastases to these areas is also derived from the concept of an oligometastatic versus micrometastatic disease state. In the oligometastatic state, the presence of small diffuse metastases (micro metastases) is inherently denied and theoretically, local excision or ablative therapies should be sufficient to control the extent of disease and possibly provide a cure. However, success in treating cases like this relies on the fact that primary tumour biology influences its metastatic potential. This explains why some patients can achieve cure of their disease even if initially considered unresectable at diagnosis. But it also explains why overall cure rates have not significantly improved although several advances in treatment have occurred over the years. Colorectal cancer metastases to the skin, breast and axilla are extremely rare and based on the published literature generally signify a poor prognosis. However, limited metastatic potential, as perhaps described in this case, may show that local therapeutic options, including surgical excision, may improve quality of life and survival.
References
- Massaut E, Ali Bohlok, Valerio Lucidi, Alain Hendlisz, Jean A Klastersky, et al. (2018) The concept of oligometastases in colorectal cancer. Current Opinion in Oncology 30(4): 1-7.
- Rodriguez-Bigas M, (2020) Locoregional methods for management and palliation in patients who present with stage IV colorectal cancer.
- Shah M, Umang Mithal, Sandeep Agarwal, Sweety Gupta, Disha Tiwari, et al. (2016) Isolated breast metastasis mimicking as second primary cancer- a case report. J Cancer Metastasis Treat 2: 391-395.
- Warner W, Tammy Y. Lee, Kimberly Badal, Tanisha M. Williams, Smriti Bajracharya, et al. (2018) Cancer incidence and mortality rates and trends in Trinidad and Tobago. BMC Cancer 18: 712.
- Micalizzi D, Maheswaran S, Haber D (2017) A conduit to metastasis: circulating tumor cell biology. Genes & Dev 31(18): 1827-1840.
- Bittencourt M, GiuseppeDel Torto, Pasquale Di Costanzo, Gorizio Pieretti, Rossella Lamberti, et al. (2018) Cutaneous metastasis of colorectal cancer. An Bras Dermatol 93(6): 884-886.
- Faenza M et al. (2019) Large single cutaneous metastasis of colon adenocarcinoma mimicking a squamous cell carcinoma of the skin: A case report. IJSCR 56: 96-100.
- Liao L, Lianggong Cheng, Qian Zhu, Guangsheng Pei, Feng, et al. (2020) Cutaneous metastasis of ascending colon cancer harboring a BRAF V600E mutation A rare case report. Medicine 99(21):1-5.
- National Comprehensive Cancer Network. Colon Cancer (Version 4.2020).
- Cheng H, Chien-JenChang, Pu-Tsui Wang, Pei-Wen Hung, Kwok-MingChang, et al. (2015) Breast Metastasis and Ovary Metastasis of Primary Colon Cancer. J Cancer Res Pract 2(4): 330-334.
- Perin T, Vincenzo Canzonieri, Lorenzo Memeo, Samuele Massarut (2011) Breast metastasis of primary colon cancer with micrometastasis in the axillary sentinel node: A metastasis that metastasized? Diagnostic Pathology 6(45): 1-3.
- Zhang S, Tao Du, Xiaohua Jiang, Chun Songet (2016) Breast metastasis of primary colorectal cancer: a case report. Int J Clin Exp Med 9(11): 22517-22523.
- Imaizumi K, Shigenori Homma, Tadashi Yoshida, Tatsushi Shimokuni, Hideyasu Sakihama, et al. (2016) Solitary left axillary lymph node metastasis after curative resection of carcinoma at the colostomy site: a case report. Surgical Case Reports 2:99.
- Kothadia J, Rezina Arju, Monica Kaminski, Arvind Ankireddypalli, Sushil Duddempudi, et al. (2015) Metastatic Colonic Adenocarcinoma in Breast: Report of Two Cases and Review of the Literature. Case Reports in Oncological Medicine.
- Lipsyc M, Rona Yaeger, Lynn T Dengel, Leonard Saltz (2015) Axillary lymph node involvement is a unique pattern of metastaqsus in BRAF-mutant colorectal cancer. JAMA Oncol 1(5): 686-687.
- Vakili SM, Majid Sharbatdaran, Askari Noorbaran, Sepideh Siadati, D Moslemi, et al. (2014) A Case of Colon Cancer with Breast Metastasis and Krukenberg Tumor. Int J Hematol Oncol Stem Cell Res 8(1): 46-50.
- Ahmad S, Kaleem Khalilullah, Katherine McGowan, Katrina Dillon (2019) Unexpected destination! Rectal carcinoma metastasis to breast. Journal of Surgical Case Reports 3: 1-6.

 Case Report
Case Report