Abstract
Several studies have been reported an association between celiac disease and other auto-immune disorders. However, very few reports in the literature showed the correlation between these disorders in pediatric age. In this observational study we selected a large case series of pediatric patients on which the serological analysis of anti-tissue transglutaminase (anti-tTGA) and concomitantly serological analysis of the antithyroid (anti-TPO) autoantibodies has been performed. We showed that the subjects positive to both tests have a significant female gender prevalence and a temporal difference between anti-tTGA positivity and anti-TPO positivity with a median of anti-tTGA positivity lower than that of anti-TPO positivity. Our data could suggest the importance of the dosage for both autoantibodies, in order to evaluate the possible appearance of autoimmune thyroid disease, for a careful monitoring of pediatric patients.
Keywords: Anti-tTGA; Anti-TPO; Pediatric Patients
Abbreviations:Anti-tTGA: Anti-Tissue Transglutaminase; Anti-TPO: Antithyroid; CD: Celiac Disease; ATD: Auto-Immune Thyroid Disease; TAI: Thyroid Autoimmunity; ELISA: Enzyme-Linked Immunosorbent Assay; ECLIA: Electro-Chemiluminescence Immunoassay
Introduction
Celiac Disease (CD) is an autoimmune disorder characterized
by inflammation, villous atrophy, and crypt hyperplasia of small
bowel mucosa after ingestion of dietary gluten and recovery when
gluten-containing cereals are withdrawn from diet [1]. Patients
with celiac disease are at high risk of having other autoimmune
disorder. In fact, CD has frequently linked to type 1 diabetes,
Addison’s disease, IgA nephropathy, pernicious anemia and autoimmune
thyroid disease (ATD) [2]. In 2008, Elfstrom, et al. reported
a two-to fourfold in-creased risk of ATD in patients with CD and
similarly that CD was more common in patients with ATD. A number
of studies also report that thyroid-related antibodies are more
frequent in CD [3]. Anyhow, the prevalence of other autoimmune
disease appeared to be closely related to age at diagnosis, or to
the duration of gluten exposure. Very few observations in the
literature report the correlation between Celiac disease and other
autoimmune disorders in pediatric age.
A large Italian multicenter study enrolled 343 consecutive
pediatric patients, 230 girls and 113 boys (median age, 8.5 years),
highlighted that ATD was found in 90 of 343 (26.2%) patients with
CD, even those on a gluten-free diet. In particular, 37 celiac patient
reported positivity to the antithyroid autoantibodies (anti-TPO)
[4]. Among the clinical investigations necessary for the diagnosis
of both diseases there is the measurement of serological levels by
luminescence methods: the immunometric evaluation of anti-tissue
transglutaminase IgA (anti-tTGA) and IgG (anti-tTGG) antibodies
indicative of a possible celiac disease, anti-thyroperoxidase (anti-
TPO) antibodies evaluation, indicative of thyroid autoimmunity
(TAI).
In this observational study we selected a large case series of
pediatric patients on which the serological analysis of anti-tTGA
and concomitantly serological analysis of the anti-TPO has been
performed.
Case Series
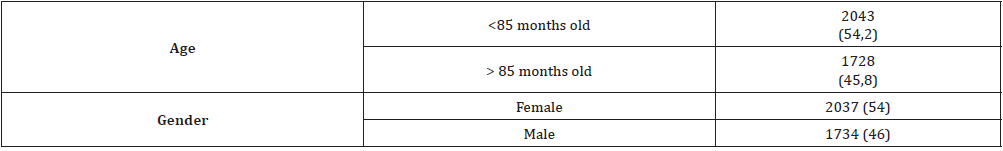
This is a retrospective observational study of pediatric patients from Campania Region in southern Italy admitted at the Santobono- Pausilipon Hospital of Naples. From June 2011 to December 2019 a cohort of 3771 children subjected to the anti-tTGA and anti-TPO tests have been selected. This study was approved by the Research Ethics Committee of the institution, and informed consent was obtained from the patients’ parents. Clinical analyses were performed using commercial kits. Immunoglobulin A anti-tTG antibodies were screened through time-resolved enzyme-linked immunosorbent assay (ELISA) technique and values lower than 16 U/ml were considered negative and positive those >16 U/ml. Anti-TPO antibodies were detected by electro-chemiluminescence immunoassay (ECLIA) and values lower than 10 U/ml were considered negative and positive those >10 U/ml. Selected patients were aged between 0 to 16 years with an median age of 84 months (Table 1).
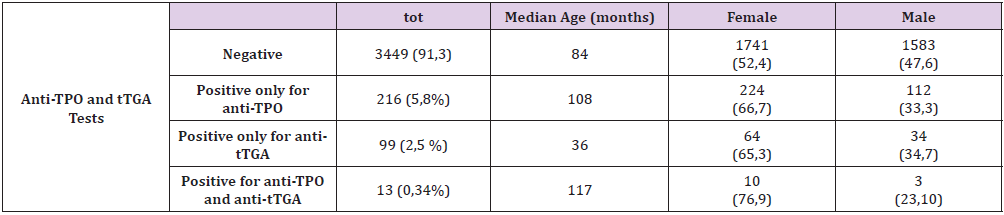
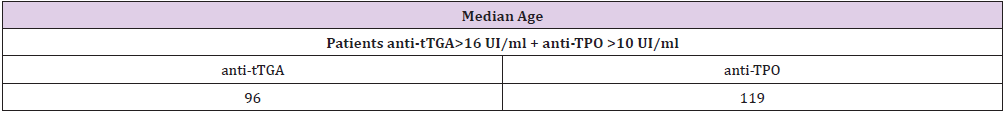
In our series 99 (2.5%) patients were positive for the anti-tTGA test ( > 16 U/ml) and negative for anti TPO-test, 216 (5.8%) patients were positive for the anti-TPO test ( > 10 U/ml) and negative for anti-tTGA test. Instead, both tests were negative in 3449 (91.3%) and positive in 13 (0.34%) patients (Table 2). Considering the 13 positive patients to both autoantibodies 10 (76.9%) children were female highlighting a gender prevalence (Table 2). Furthermore, a temporal difference be-tween anti-tTGA positivity and anti-TPO positivity has been detected, confirmed by the calculation of the median age in months, with a median of anti-tTGA positivity lower than that of anti-TPO positivity (Table 3). In addition, the median in months of anti-tTGA positivity of patients positive to both autoantibodies (96 months) is higher than the patients positive only for anti-tTGA (36 months) (Table 3).
Table 3: Median in months of anti-tTGA positivity of patients positive to both autoantibodies and for patients positive only for antitTGA.
Since our case series has been selected analyzing data contained in the archive of a pediatric hospital, as results of routine diagnostics, the patients are not subjected to the two measurements in the same chronological order.
Discussion
In order to analyze the potential relation between celiac disease
and autoimmune thyroid disease in pediatric age, we selected a total
of 3771 pediatric patients subjected to the measurement of the antitTGA
and anti-TPO auto-antibodies, over a period of approximately
8 years. Once we extrapolated the data from our hospital archive,
we identified the total patients positive for anti-tTGA and those
positive for anti-TPO auto-antibodies, and following a cross-check,
13 subjects positive for both tests were selected. Many studies have
been reported an association between celiac disease and other
auto-immune disorders, including type 1 diabetes [5] Addison’s
disease [2], IgA nephropathy [2], and pernicious anemia [2]. A
large study reported a two- to fourfold increased risk of ATD in
patients with CD [2], and similarly that CD was more common in
patients with ATD. A number of studies also report that thyroid related antibodies are more frequent in CD [2]. Regarding pediatric
population, a large multicenter study was performed on a large
Italian patient population from Torino, Bologna, Foggia, Rome,
Naples, and Bari to establish the prevalence of autoimmune thyroid
involvement in a large group of untreated and treated pediatric
patients with CD [4].
This study showed an increased prevalence of serologic and/
or echographic evidence of thyroid autoimmunity among pediatric
patients with CD. Other studies reported the presence of serum
organ-specific autoantibodies in patients with CD seems related to
the presence of a second autoimmune disease and does not appear
to be gluten-dependent [5]. In addition, in a very large Italian study,
the prevalence of other autoimmune diseases appeared to be closely
related to age at diagnosis and to the duration of gluten exposure
[6]. In our study, the percentage of patients with pathological values
for both autoantibodies is about 0.34%. By focusing on anti-tTGA
positive patients, 11.6% are also positive for anti-TPO. This data are
in line with the scientific literature [3,4,7,8]. Similarly, if we consider
anti-TPO positive subjects, the percentage of patients also positive
for anti-tTGA is 6.05%. This result is also in line with the data from
the literature [9]. The new and interesting data of our study is the
prevalence of the female gender among the tTGA positive subjects,
also found in the 13 patients with positivity to both auto-antibodies.
Furthermore, we have observed, as hypothesized in previous
studies [7], that the appearance of autoantibodies directed against
thyroperoxidase is closely associated with the age of diagnosis of
CD patients.
In fact, in the 13 subjects with both auto-antibodies, we have shown that the median age in months of positivity for anti- tTGA is higher than positivity only for anti-tTGA. This finding therefore seems to confirm the hypothesis that the delayed diagnosis of CD and therefore the prolonged exposure to gluten is probably co-responsible for the subsequent production of anti-TPO. The coexistence of CD and the diseases of autoimmune thyroid has been highlighted twenty years ago in a study in which it was performed the evaluation of antithyroid anti-bodies in children with CD. Data showed that elevated titles of anti-TPO antibodies TPO have been detected in children with coeliac disease (11.7%) in comparison to control group, suggesting the need for performing the screening tests for antithyroid antibodies in children with CD [8]. Moreover, several studies in the literature reported a correlation be-tween CD and ATD also supported by a genetic pattern screening [9,10]. Hadithi, et al. analyzed 104 patients with Hashimoto’s thyroiditis and five patients positive for celiac serology, with documented villous atrophy, were diagnosed. Genetic pattern HLA-DQ2 (and/ or -DQ8) was present in all the five patients [9]. Furthermore, the clinical significance of the presence of these autoantibodies is still un-clear, and long-term follow-up of a larger series in controlled studies would be needed to better describe the phenomenon.
Conclusion
In the future it would be interesting to conduct further studies
on screening of genetic pat-tern of pediatric patients that report
pathological values of both auto-antibodies, focusing on the HLA
complex characterization.
It would also be appropriate to suggest careful monitoring
of pediatric patients by suggesting the antibody dosage for both
anti-tissue transglutaminase and antithyroid autoantibodies in
order to avoid future immune decompensation, avoiding a delayed
diagnosis of celiac disease and over time the possible appearance of
autoimmune thyroid disease.
Consent
Our patients signed informed consent form for the material presented to appear in the publication above and in related publications, prior to submission.
Funding
None
Conflicts of Interest
None
Acknowledgements
We would like to thank Eurospital Diagnostics for support monitoring of the study.
References
- Makharia GK, Verma AK, Amarchand R, Bhatnagar S, Das P, et al. (2011) Prevalence of celiac disease in the northern part of India: A community based study. J Gastroenterol Hepatol 26(5): 894-900.
- Abhik Roy, Laszkowska M, Sundström J, Lebwohl B, Green PHR , et al. (2016) Prevalence of Celiac Disease in Patients with Autoimmune Thyroid Disease: A Meta-Analysis. Thyroid 26(7): 880-890.
- Venturi A, Neri E, Ughi C, Leopaldi A, Città A (2000) Gluten-dependent diabetes-related and thyroid-related autoantibodies in patients with celiac disease. J Pediatr 137(2): 263-265.
- Ansaldi N, Palmas T, Corrias A, Barbato M, D'Altiglia M, et al. (2003) Autoimmune Thyroid Disease and CeliacDisease in Children J Pedriat Gastroenterol Nutr 37(1): 63-66.
- Elfstrom P, Sundstrom J, Ludvigsson JF (2014) Systematic review with meta-analysis: associations between coeliac disease and type 1 diabetes. Aliment Pharmocol Ther 40(10): 1123-1132.
- Ventura A, Magazzù G, Greco G (1999) Autoimmune disorders in coeliac disease: relationship with duration of gluten exposure. Gastroenterology 117(2): 303-310.
- Kowalska E, Wasowska Królikowska K, Toporowska Kowalska E (2000) Estimation of antithyroid antibodies occurrence in children with coeliac disease. Med Sci Monit 6(4): 719-721.
- Spadaccino AC, Basso D, Chiarelli S, Albergoni MP, D'Odorico A, et al. (2008) Celiac disease in North Italian patients with autoimmune thyroid diseases. Autoimmunity 41(1): 116-121.
- Hadithi M, Boer H, Meijer JWR, Willekens F, Kerckhaert JA, et al. (2007) Coeliac disease in Dutch patients with Hashimoto's thyroiditis and vice versa. World J Gastroenterol 13(11): 1715-1722.
- Kahaly GJ, Frommer L, Schuppan D (2018) Celiac disease and endocrine auto-immunity - the genetic link. Autoimmun Rev 17(12): 1169-1175.

 Case Report
Case Report