Abstract
Objective: A study was designed to evaluate the incidence, mechanism of injury and treatment outcomes of ophthalmic injuries associated with maxillofacial trauma.
Material and Methods: 3708 patients who sustained maxillofacial trauma during the years from August 2006 to July 2019 and were included in this retrospective study. Patients’ records were reviewed for gender, age, site of injury, aetiology of trauma, concomitant injuries, ophthalmic assessment and method of treatment. Minor and major ophthalmic injuries were recorded.
Results: Of the 103 patients, 81 were male with a median age of 38 years. Road traffic accident was the most common mechanism of injury (72/103, 70%). Common minor ophthalmic injuries included diplopia, enophthalmos, subconjunctival haemorrhage and restriction of the extraocular muscles, while major injuries included subretinal haemorrhage, retrobulbar haemorrhage, ruptured globe and detached retina. Most major ophthalmic injuries occurred in association with orbital fractures. Visual acuity was reduced in 15 patients, four of whom experienced persistent postoperative changes at eight weeks. Lack of vehicle drivability showed a highly significant association with major ophthalmic injury (p=0.001). The incidence of loss of vision was 0.97% (1/103).
Conclusion: Prompt assessment and treatment of ophthalmic injuries is of paramount importance in patients with fractures involving fractures of orbital walls.
Keywords:Ocular injury; Maxillofacial trauma; Blindness; Midface fractures; Ophthalmic injury
Introduction
Ocular injuries very often are associated with maxillofacial
trauma. Injuries to and around the eye may vary in presentation
and severity. Careful ophthalmic examination must be a part of the
initial assessment in all maxillofacial trauma patients [1]. Blindness
is a potential complication from missed ophthalmic injuries, while
certain ophthalmic injuries may be readily evident. In case such
injuries are missed at first observation, the treating surgeon may
face medicolegal consequences [2]. Opthalmic injuries may range
from certain minor ophthalmic injuries such as abrasions or
lacerations to the eyelids or cornea to major injuries which may
be potentially blinding. In all motor vehicular accidents, the injury
tends to be severe, leading to fracture of the orbit or rupture/
penetration of the globe by glass pieces [1].
An ophthalmologist must be a part of the treating team for
ocular injury assessment and management. Maxillofacial surgeons
may not be aware of many types of ocular injuries that may
occur as well as their diagnosis, appropriate therapy or ultimate
prognosis. Some ocular injuries may mandate concomitant surgical
treatment with maxillofacial fracture repair, while in some cases,
presence of an ocular injury may mandate a delay in ophthalmic
injury repair secondary to repair of maxillofacial fractures [3]. The
incidence of visual loss and blindness from maxillofacial fractures
varies from 0.7 to 10.8% [4] and the causes reported in literature
include retrobulbar haemorrhage, ruptured globe and traumatic
optic neuropathy. Preoperative assessment of ophthalmic injuries
is providing a safeguard to the maxillofacial surgeon. Ophthalmic injury management must be given preference over facial fracture
repair, as surgical treatment of the facial fractures in the presence
of an untreated severe ophthalmic injury may exert pressure on the
eye. This may eventually hamper the prognosis for the globe [5].
Recognition of an ophthalmic injury before operative intervention
is important as it guards against a postoperative allegation from
the patient alleging the surgical procedure to be the cause of any
permanent visual disturbance.
The objective of this study was to determine the incidence and
types of ocular and motility disorders in patients who had sustained
maxillofacial injuries. Further, we aimed to evaluate mechanism
of injury, facial fracture type and treatment outcomes of patients
treated for ophthalmic injuries and maxillofacial bone fractures.
Methods
A retrospective study was designed to include surgical records
of all patients admitted to the Department of Oral and Maxillofacial
Surgery at School of Dental Sciences, Greater Noida, Uttar Pradesh,
India who sustained a maxillofacial fracture during the years from
August 2006 to July 2019. Excluded from the analysis were patients
with maxillofacial fractures not associated with ophthalmic
injuries, cranial bleeds that required craniotomy and pre-existing
ophthalmic defects. The Institutional ethics committee approved
the study. We reviewed patients’ charts for data which were
collected during this 13 year period. Our surgeons examined 3708
patients with maxillofacial fractures. Radiographs and computed
tomography scans were utilized to confirm the diagnosis. An
ophthalmologic examination by a consultant ophthalmologist was
conducted in cases of zygomatico-maxillary, orbital, naso-orbitoethmoidal,
Lefort III, Lefort II, Lefort I and panfacial trauma cases
when deemed necessary.
Patients’ personal and clinical data, mechanism of injury and
clinical ophthalmic signs were reviewed. All patients had signed
informed consent letters as part of the presurgical protocol.
Ophthalmic signs were divided into “minor” or “major” based
on the chances of the injury leading to permanent loss of vision.
Impairment of visual acuity was categorized as “mild” with
readings of 6/12 or 20/40, “moderate” between 6/12 or 20/40
and 6/60 or 20/200 or “severe” with less than 6/60 or 20/200,
following a careful assessment. Patients were grouped into four
groups depending on the type of operative intervention that they
required. Group I consisted of purely orbital fractures or nasoorbito-
ethmoid (NOE) fractures; Group II included fractures
of LeFort I, II and III levels; Group III were fractures of the of
zygomatico-maxillary-complex [ZMC]; and Group IV included
pan facial fractures (midface with mandible fractures). Fractures
were either treated by open reduction and internal fixation with
titanium miniplate and screw system under a general anaesthetic
or managed conservatively. Orbital defects were reconstructed with
titanium mesh were indicated. Ophthalmic injuries were managed
by specialist ophthalmologists.
Drivability criteria involved a measurement of visual acuity for
each eye separately and without optical correction. In cases where
optical correction was needed, vision was retested with appropriate
corrective lenses. A standard visual acuity chart such as Snellen
chart was used with five letters on the 6/12 line. Charts are placed
six metres from the person tested. More than two errors in reading
the letters of any line were regarded as a failure to read that line. In
the case of a private vehicle driver, uncorrected vision (without eye
glasses) must be a minimum of 6/12 to pass the drivability criteria.
For commercial vehicle drivers, visual acuity in the driver’s both
eyes or better eye (with or without corrective lenses) must be 6/9
or better. 6/9 or 6/12 vision meant that the patient must be able to
see clearly a letter or alphabet on the Snellen chart at a distance of
6 metres what a person with normal vision may see clearly at 9 or
12 metres respectively.
Data collected was recorded in Microsoft Excel and analysed
using IBM SPSS Statistics for Windows (version 22.0, IBM Corp,
Armonk NY, USA). The Kolmogorov-Smirnov test of normality with
Lilliefors significance correction was used to test for normality
of continuous variables in the study. Based on the outcome of the
normality test, median and inter quartile range (IQR) for nonparametric
data were derived. Descriptive data were reported
as a number (%). Categorical data were analysed using the Chi
square test to determine whether there was a significant difference
between minor and major ophthalmic signs and other variables.
Binary logistic regression was utilized to assess the significance
of association between minor and major ophthalmic signs, the
severity of visual impairment, and its association with the various
locations of fractures. A probability value of < 0.05 was considered
as statistically significant.
Results
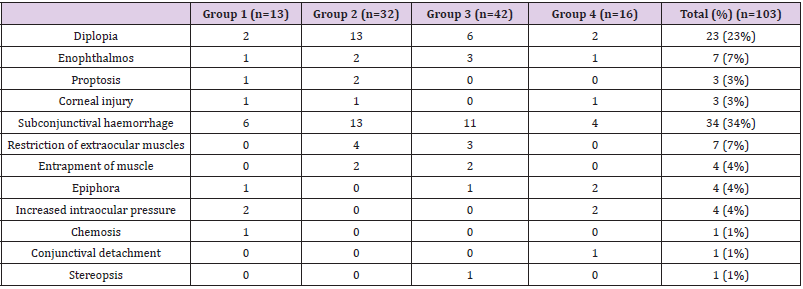
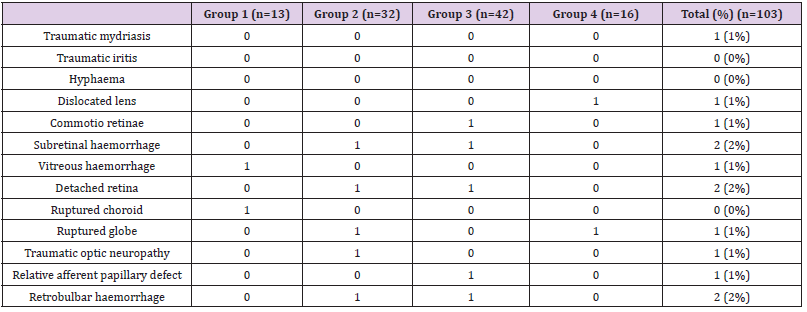
The study sample consisted of 103 patients, of whom 81 were male (79%), with a median (IQR) age of 38 (18-59) years. The number of patients who had each type of fracture were Group I (n=13, 13%), Group II (n=32, 31%), Group III (n=42, 41%), and Group IV (n=16, 16%). Road traffic accident (RTA) was the most common mechanism of injury, and accounted for 72/103 cases (70%), followed by assaults (15/103, 15%), falls (13/103, 13%), and sports injuries 03/103, 5%). Most patients (90/103) were surgically treated within 2 weeks of the trauma. Those treated after this period were those with persistent diplopia or unaesthetic enophthalmos, or those in whom early orbital reconstruction was contraindicated because of persistent, severe, intra ocular injuries. Minor and major ophthalmic findings are outlined in Tables 1 & 2.
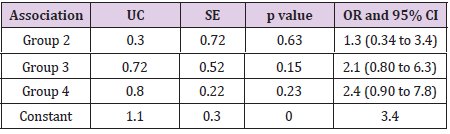
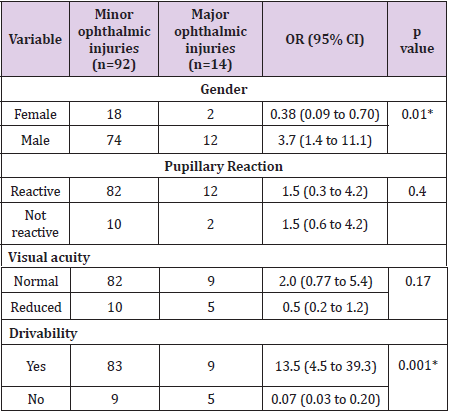
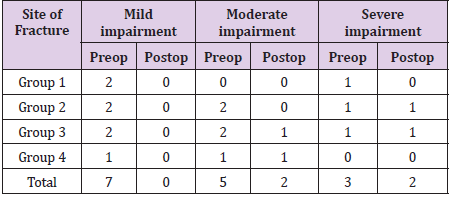
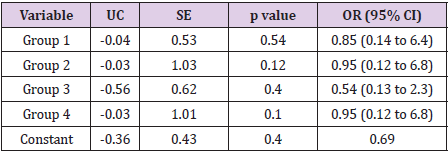
Table 3 shows the association of minor and major ophthalmic signs and the various types of fracture using univariate logistic regression, with the reference group being orbital trauma. The regression model explained between 3.2% (Cox and Snell R2) and 5.6% (Nagelkerke RS2) of variance and correctly classified 80% of cases. Visual impairment severity is tabulated in Table 4. Impairment of visual acuity before and after operation for the various types of fractures is shown in Table 5. The association between severity of loss of vision and the various types of fracture using univariate logistic regression with the reference group being orbital trauma is tabulated in Table 6. The regression model explained between 1.6% (Cox and Snell R2) to 2.2% (Nagelkerke RS2) of variance and correctly classified 68 % of cases.
Table 3: Univariate logistic regression analysis for association between minor/major ophthalmic injuries and fracture groups (reference group: orbital trauma).
UC= Unstandardised coefficient, SE = Standard error, p < 0.05, OR= Odds ratio, CI = Confidence interval.
Table 6: Univariate logistic regression analysis for association between severity of visual impairment and types of fracture (reference group: orbital trauma).
UC= Unstandardized coefficient, SE = Standard error, p < 0.05, OR= Odds ratio, CI = Confidence interval.
Discussion
This study retrospectively analysed data on patients’ personal
and clinical details, mechanisms of injury and the preoperative
ophthalmological injuries associated with maxillofacial fractures.
Studies have indicated the association between ophthalmic injuries
and midface fractures [6,7]. However, these studies failed to specify
the type of fracture or the specific ophthalmic injuries sustained.
Most of these studies have reported ocular injuries in patients with
midface fractures in general [8], without specific categorization
of maxillofacial fractures. However, our study has segregated
ophthalmological injuries into those associated with the four
different categories of fractures. The results indicated that there
were considerably more male than female patients (81/103, 79%)
with maxillofacial fractures and the median age was 38 years (IQR
18-59). These findings were consistent with the results of some
previous studies [6,7]. The distribution of mechanism of injury was
predominated by road traffic accidents, followed by a distant second
by interpersonal violence or assault. This pattern is drastically
different from similar studies on ocular injuries [5,9,10], where
the predominant cause of injury was alcohol-related assault. This
difference could be attributed to the fact that all these studies were
carried out western countries where there is a higher prevalence of
alcohol-related interpersonal violence.
The reported incidence of ophthalmic injuries associated
with maxillofacial fractures is very much dependent on the
exact classification system used to quantify them. This study
has segregated ophthalmic injuries into minor/temporary/
reversible injuries and major/irreversible/permanent injuries.
This classification was modified from those described previously
[11,12]. Subconjunctival haemorrhage, diplopia, enophthalmos and
restriction of extra ocular muscles, in decreasing order of frequency,
were the commonest minor ophthalmic injuries associated with
maxillofacial fractures. Further, entrapment of extra ocular muscles
was observed only in Group 2 and 3. Subretinal haemorrhage,
detatched retina, ruptured globe and retrobulbar haemorrhage
were the commonest major ophthalmic injuries associated with all
maxillofacial fractures.
This study confirms the fact that the reported incidence of
major ophthalmic injuries is low [13,14]. A majority of the major
ophthalmic injuries were recorded in group 2 and 3. This finding
seems to suggest that a greater degree of intraocular damage can
result from these types of fractures than by any other maxillofacial
fractures.
The univariate logistic regression analysis for ophthalmic
injuries and types of fracture showed no statistically significant
relation. However, findings from the study indicated that, fortunately,
minor ophthalmic injuries are more likely than major ophthalmic
injuries. Two patients experienced retrobulbar haemorrhage, one
had traumatic optic neuropathy and one had a ruptured globe.
Traumatic optic neuropathy can be a cause of severe permanent
visual impairment, many times with concomitantly reduced visual
acuity or a relative afferent papillary defect [15]. However, the
patient in our study regained full vision following high dose steroid
therapy with concomitant reduction of fractures and fixation.
Permanent loss of vision or blindness is an unfortunate
complication associated with maxillofacial fractures, whose
reported incidence varies between studies, 0.32%-9% [16] and
0.7-3% [7]. This devastating consequence may manifest as a result
of direct injury to the globe, optic nerve injury, retinal oedema or
detachment, vascular compromise to the eye, intracranial injury to
the optic chiasm or brain and retrobulbar hemorrhage [16,17]. It
would be prudent to think that patients on anticoagulants might
be at an increased risk of a retrobulbar bleed. Therefore, a careful
medical history must be sought at initial examination. Furthermore,
literature review indicates that blindness is commonly observed
with penetrating injury to the globe, an increased number of facial
fractures, ZMC complex fracture, a Glasgow Coma Scale score less
than or equal to 8 at examination and involvement of all three
eye zones from injury [18]. Some uncommon causes of blindness
reported in literature include optic nerve transaction, globe luxation and retinal detachment [19]. Out of the two patients with
retrobulbar haemorrhage in this study, one lost vision in the eye.
Reduced visual acuity was diagnosed in all patients who did
not score 6/6 on visual assessment. Five patients with major
ophthalmic injuries (5/14, 36%) and 10 out of 85 patients (10/85,
12%) with minor ophthalmic injuries experienced reduced visual
acuity in our study. Twelve of these 15 patients needed orbital wall
reconstruction. Similar percentage distributions were reported by
other studies [11,20]. This finding reinforces the fact that greater
intraocular damage may be expected from maxillofacial fractures
that disrupt orbital walls than after other types of fracture.
Four patients experienced persistent postoperative changes at
12 weeks, with preoperative ophthalmic injuries of commotio
retinae, subretinal haemorrhage, globe rupture and retrobulbar
haemorrhage.
Drivability relates to the patient’s ability to drive independently, whether private (lesser than 6/12) or commercial vehicles (lesser than 6/9). There was a significant association of male gender with ocular injuries, a finding derived from the fact that maxillofacial fractures were also predominant in the male population in our study. Visual acuity and papillary reactivity did not differ significantly. However, the study found an OR of 0.07 (95% CI 0.03 to 0.20, p = 0.001) for those patients who had a major ophthalmological sign and inability to drive, which was statistically significant. No significant associations were observed in univariate logistic regression analysis between impairment of visual acuity and types of fracture. However, findings from the study reinforce the finding that visual impairment is a risk of any maxillofacial fracture that involves the orbit. Improvement in visual acuity within a week of the injury has been reported [20], a finding confirmed in our study. Fractures of the Le Fort III level and ZMC fractures, even when present as a part of panfacial fractures are associated with a higher proportion of major than minor ophthalmic injuries. This fact may be a result of high velocity being the main mechanism of trauma in such cases [4]. Similar observations have been reported in other studies on the subject [16,21,22].
The retrospective design of the study was a shortcoming which could be overcome by evaluating ophthalmic injuries with maxillofacial fractures in a prospective manner. The large sample size and availability of complete follow up records are the strengths of this study.
Conclusion
Ophthalmic injuries must be suspected in midface injuries and promptly evaluated by an ophthalmologist, particularly in case of ZMC and Le Fort II/ III fractures. Minor injuries are commoner than major injuries. However, a missed diagnosis of ophthalmic injury could lead to permanent alteration or loss of vision, thereby inviting medico legal consequences
References
- Mittal G, Singh N, Suvarana S, Mittal SR (2012) A prospective study on ophthalmic injuries related to maxillofacial trauma in Indian population. Natl J Maxillofac Surg 3(2): 152-158.
- Dutton GN, Al-Qurainy (1997) Oral and Maxillofacial trauma. In: Fonseca RJ, Walker RV, editors. 2nd Pennsylvania: W.B. Saunders Company.
- Holt GR, Holt JE (1983) Incidence of eye injuries in facial fractures: An analysis of 727 cases. Otolaryngol Head Neck Surg 91(3): 276-279.
- Magarakis M, Mundinger G, Kelamis J, Dorafshar AH, Bojovic B, et al. (2012) Ocular injury, visual impairment and blindness associated with facial fractures: a systematic literature review. Plast Reconstr Surg 129(1): 227-233.
- Jamal BT, Pfahler S, Lane K, Bilyk JR, Pribitkin EA, et al. (2009) Ophthalmic injuries in patients with zygomaticomaxillary complex fractures requiring surgical repair. J Oral Maxillofac Surg 67(5): 986-989.
- Zhou H, Liu Q, Yang R, Li Z, Li ZB (2014) Ocular trauma in patients with maxillofacial fractures. J Craniofac Surg 25(2): 519-523.
- Septa D, Newaskar V, Agrawal D, Tibra S (2014) Etiology, incidence and patterns of mid-face fractures and associated ocular injuries. J Maxillofac Oral Surg 13(2): 115-119.
- Patil SG, Kotwal I, Joshi U, Allurkar S, Thakur N, et al. (2016) Ophthalmological evaluation by a max-illofacial surgeon and an ophthalmologist in assessing the damage to the orbital contents in midfacial fractures: a prospective study. J Maxillofac Oral Surg 15(3): 328-335.
- Mellama P, Dewan M, Lee M, Smith SD, Harrison AR (2009) Incidence of ocular injury in visually asymptomatic oribtal fractures. Ophthal Plast Recontr Surg 25(4): 306-308.
- Johnson NR, Singh NR, Oztel M, Vangaveti VN, Rahmel BB, et al. (2018) Ophthalmological injuries associated with fractures of the orbitozygomaticomaxillary complex. British Journal of Oral and Maxillofacial Surgery 56(3): 221-226.
- Al-Qurainy I, Stassen L, Dutton G, Moos KF, El-Attar A (1991) The characteristics of midfacial fractures and the association with ocular injury: a prospective study. Br J Oral Maxillofac Surg 29: 291-301.
- Agrawal R, Shah M, Mireskandari K, Yong GK (2013) Controversies in ocular trauma classification and management: review. Int Ophthalmol 33(4): 435-445.
- Kloss F, Stigler R, Brandstatter A, Tuli T, Rasse M, et al. (2011) Complications related to mid-facial fractures: operative versus non-surgical treatment. Int J Oral Maxillofac Surg 40(1): 33-37.
- Karabekir H, Gocmen-Mas N, Emel E, Karacayli U, Koymen R, et al. (2012) Ocular and perocular injuries associated with an isolated orbital fracture depending on a blunt cranial trauma: anatomical and surgical aspects. J Craniomaxillofac Surg 40(7): e189-e193.
- Lee V, Ford R, Xing W, Bunce C, Foot B (2010) Surveillance of traumatic optic neuropathy in the UK. Eye (Lond) 24: 240-250.
- Ansari MH (2005) Blindness after facial fractures: a 19-year retrospective study. J Oral Maxillofac Surg 63(2): 229-237.
- Andrews BT, Jackson AS, Nazir N, Hromas A, Sokol JA, et al. (2016) Orbit fractures: identifying patient factors indicating high risk for ocular and periocular injury. Laryngoscope 126(suppl 4): S5-S11.
- Vaca EE, Mundinger GS, Kelamis JA, Dorafshar AH, Christy MR, et al. (2013) Facial fractures with concomitant open globe injury: mechanisms and fracture patterns associated with blindness. Plastic and reconstructive surgery 131(6): 1317-1328.
- Bossert RP, Girotto JA (2009) Blindness following facial fracture: treatment modalities and outcomes. Craniomaxillafac Trauma Reconstr 2(3): 117-124.
- Richards N, Brown N, Kidwell Jr E (2015) Visual acuity in orbital floor fractures: does surgical subspecialty management matter? J Craniofac Surg 26(5): 1668-1672.
- Beogo R, Coulibaly TA, Dolo MT, Traore I, Ouattara B, et al. (2018) Facial fracture-associated blindness. Journal of Craniofacial Surgery 29(3): 751-753.
- Rallis G, Stathopoulos P, Igoumenakis D, Krasadakis C, Mourouzis C, et al. (2015) Treating maxillofacial trauma for over half a century: how can we interpret the changing patterns in etiology and management? Oral Surg Oral Med Oral Pathol Oral Radiol 119(6): 614-618.

 Research Article
Research Article