Abstract
Objectives: The aim of the study is to assess the subjective and objective factors in office workers who use computers as the primary tool of everyday work.
Methods: The retrospective study included 119 individuals – office workers who worked in front of a computer every day. The study was conducted in an Outpatient Department in Warsaw between October 2019 and February 2020. We compared the parameters assessing the condition of the ocular surface (the OSDI questionnaire, Schirmer’s test, NIBUT, osmolarity) in persons who had used computers for many years. The parameters were assessed before and after using lubricating drops and the appropriate modification of occupational hygiene.
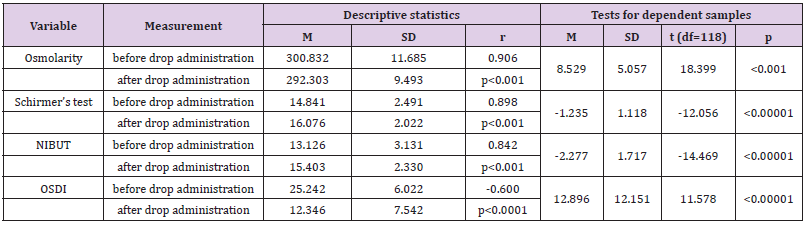
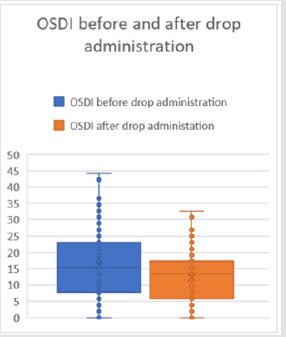
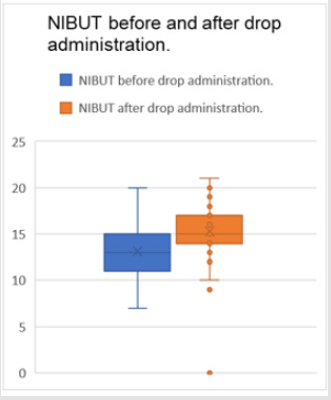
Results: We obtained the following results: the mean baseline osmolarity was 300.832±11.685, and in the final phase it was 292.303±9.493. The mean Schirmer’s test result before instilling drops was 14.84±2.491, while after drop administration the mean was at the level of 16.076±2.02 millimeters. The mean NIBUT result prior to instilling drops was 13.126±3.131 seconds, while at the end of the study it was 15.403±2.33. The mean OSDI score before drop administration in office workers was 25.242±6.022, while after instilling drops and appropriate work modification it was 12.346±7.542.
Conclusion: A large amount of time spent in front of a screen may cause serious consequences for the eyes leading to severe dry eye syndrome and all the related consequences including the deterioration of vision. The correct diagnosis of eyeball surface disorders and the proper modification of working conditions may reduce or eliminate the problem entirely.
Keywords: Computer Users; Dry Eye; Osmolarity; Discomfort; Lubricants
Introduction
Currently, due to technological development people spend increasing amounts of time in front of a screen at work and at home [1]. It leads to the development of economy, industry and modern technologies. Conversely, more and more users of electronic devices complain of unfavourable symptoms associated with the eyes [2-4]. In 1994 the American Academy of Ophthalmology used the definition of computer vision syndrome (CVS) to describe ocular and extraocular manifestations associated with near-vision work, which are experienced during work on the computer or other electronic devices, such as tablets or smartphones [5]. It was noted that computer users complained of such signs and symptoms as eye redness, irritation, burning, ocular pain, sensation of having sand under eyelids. Some patients experienced double or blurred vision, or even a subjective feeling of visual deterioration [6]. In Poland, due to the increasing access to computers CVS is a growing social problem. According to data obtained in 2020 the average time spent by Polish computer users in front of a screen was 6 h 26 min (the data were retrieved from Digital 2020 report published by WeAreSocial website in cooperation with Hootsuite). The risk of developing various ocular problems was found to increase with work duration of over 4 hours [5,6]. The problem will be intensifying in the following years. It is associated with prolonged lifespan, longer working time, and the necessity to work on the computer. Therefore, it is important to increase patient awareness of suitable working conditions to provide proper care of the eyesight.
Objective
The aim of the study is to assess subjective and objective factors in office workers who use computers as the primary tool of everyday work. It is the first study conducted in the Polish population to assess the parameters testing the eyeball surface in computer vision syndrome and their analysis after the administration of lubricating drops and the implementation of suitable work hygiene in computer users.
Subjects and Methods
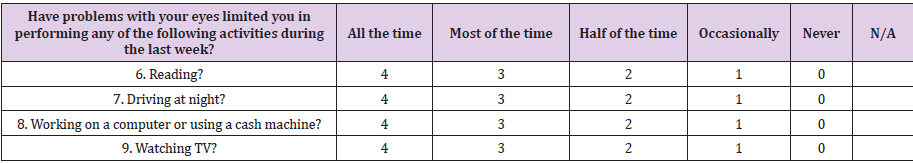
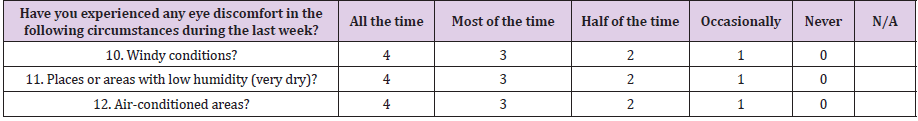
The retrospective study included 119 individuals – office workers who used a computer every day. The study was conducted in an Outpatient Department in Warsaw between October 2019 and February 2020. Study participants were asked about the number of hours they spent in front of a computer daily, job seniority in the current workplace expressed in years. The study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all the subjects. The subjective assessment of ocular manifestations in computer users. The participants completed the OSDI (Ocular Surface Disease Index) questionnaire concerning the symptoms, their influence on visual quality and environmental factors which may trigger or exacerbate the symptoms. The content of the questionnaire is presented in Tables 1-3 below. The OSDI index is calculated according to the formula:

The Ocular Surface Disease Index is assessed on the scale from 0 to 100 with higher scores referring to more severe manifestations and ocular surface disorders [7].The total score interpretations are: from 0 to 12 (normal score), 13-22 (mild dry eye syndrome), 23-32 (moderate dry eye syndrome), and 33-100 (severe dry eye syndrome). The objective assessment of ocular manifestations in computer users. Schirmer’s test used for the quantitative assessment of the watery layer of the tear film, osmolarity and the non-invasive tear break-up time (NIBUT) are important parameters in the diagnostics of ocular disorders and the diagnosis of dry eye syndrome [8]. The parameters were measured in the same room at the temperature of 22 degrees Celsius and the air humidity of 45%. Schirmer’s test was performed after instilling 1 drop of an analgesic medication (Proxymetacaine hydrochloride 0.5%) in the conjunctival sac. One minute had to pass to obtain the therapeutic effect of the drops. A strip of test paper was placed in the lateral canthus. The eyes had to be closed for another 5 minutes. The result was visible on the millimeter scale of the strip showing its wetting.
All study participants had the osmolarity of the tear film measured with the TearLab device. Non-invasive tear film breakup time (NIBUT) was tested with comprehensive eye surface and tear analyser (OSA). All study participants were advised to use lubricating drops including trehalose 3% and sodium hyaluronate 0.15%. The dosage was 1 drop, four times a day for 2 months. The participants were instructed to introduce appropriate conditions of work on a computer, i.e. the proper distance between the eyes and the screen (65-80 cm), proper lighting in the workplace, frequent blinking, breaks every 30 minutes of work in front of a screen and fixing one’s eyes on a distant point for a minute. The OSDI questionnaire, Schirmer’s test, osmolarity, and NIBUT were performed again after 2 months.
Statistical Analysis
A t-Student test for dependent samples was used to compare the analyzed values: the OSDI index, Schirmer’s test, osmolarity, NIBUT before and after using lubricating drops, and suitable work hygiene. Statistical calculations and graphs were performed with Excel 365 and Statistica 12 licensed to the Medical University of Warsaw.
Results
The study included 119 participants (79 men and 40 women) who had been using computers for a long time. Their average age was 38.34±6.99 (range: 25-55) years. The mean duration of daily work on the computer was 4.8±2.09 (range: 2-10) hours. The mean job seniority in the workplace requiring work on the computer was 13.66±7.01 (range: 2-27) years. The mean baseline osmolarity was 300.832 mOsm/l ±11.685, while after drop administration it was 292.303±9.493 mOsm/l. It was demonstrated that osmolarity was significantly higher prior to instilling drops (p<0.001). The mean Schirmer’s test result before instilling drops was 14.84±2.491 millimeters, while after drop administration the mean was at the level of 16.076±2.022 millimeters. Schirmer’s test results were significantly higher after drop administration (p<0.00001). The mean NIBUT score prior to instilling drops was 13.126±3.131 seconds, while after the administration it was 15.403±2.33 seconds. NIBUT results were significantly higher after drop administration (p<0.00001). As regards the OSDI variable the mean baseline result was at the level of 25.242±6.022, while 2 months later it was 12.346±7.542. OSDI reached significantly higher scores prior to instilling drops (p<0.00001) (Table 4) (Figures 1&2).
Discussion
It is commonly known that the large amount of time spent in
front of a computer has a negative effect on the condition of the
eyeball surface, which may lead to dry eye syndrome [8]. The
complaints of eye discomfort, sensation of a foreign body, pain,
blurred or deteriorated vision are more commonly voiced by
computer users than by those who spend little time in front of a
screen. The symptoms exacerbate during reading, watching TV,
driving a car, or spending time in dry air-conditioned rooms [9,10].
Such undesirable manifestations lead to the malaise, poor mental
status and even frustration. It may result in the reduced productivity
of workers [10,11]. In a study conducted on a group of Polish
dentistry students by Bartoszek et al. over 70% of participants
suffered from computer vision syndrome. In contrast to our study
they were younger individuals (mean age 21,65 years, SD 1,98) and
women dominated (77%) vs our study (33,6%) [12].
The present study showed the influence of working on
a computer on the condition of the ocular surface measured
through the following parameters: the OSDI index, Schirmer’s test,
osmolarity, non-invasive tear film break-up time in office workers
and the improvement of the parameters after the administration
of lubricating drops and adjusting working conditions. According
to the present analysis the mean Schirmer’s test result was
14.84±2.49 seconds which means the initial deficit of the watery
component of tears. Nakamura et al. also demonstrated a reduction
in tear secretion and indicated poorer Schirmer’s test results in
individuals using computers for many years [13]. Akkaya et al. noted
no significant difference between Schirmer’s test results obtained
in the morning and evening in a group of workers using computers.
Similar observations were reported by Uchino, et al. [14,15]. The
osmolarity of the tear film is one of the best markers of dry eye
syndrome [16]. Increased osmolarity has a negative influence
on the corneal epithelium, causing its more marked shedding,
increased loss of intercellular connections, and the aggravation of
symptoms associated with dry eye syndrome in people [17,18].
Normal osmolarity values of the tear film range from 296 to
302 mOsm/l in healthy individuals [19]. The present analysis
showed the mean baseline value of osmolarity to be within normal
limits for the healthy population (300.832±11.685 mOsm/l). The
mean non-invasive tear break-up time (NIBUT) prior to drop
administration in office workers was 13.13±3.13 seconds, which is
normal in the healthy population. The result of over 10 seconds is
considered normal for the healthy population [16]. A similar result
was obtained by Unlü et al. They reported the mean non-invasive
tear break-up time at 11.37±3.69 seconds in computer users
[10]. Uchino et al. obtained much lower values in a group of office
workers. The results were 4±2.5 seconds which meant advanced
dry eye syndrome [15]. The present analysis showed that the mean
OSDI index in computer users before instilling drops was 25.24,
which meant moderate dry eye syndrome. OSDI values reported
in the literature are higher. Unlü et al. reported the OSDI index of
37.12±19.05 in their analysis [20]. The fact that our patients used
lubricating drops including trehalose 3% and sodium hyaluronate
0.15% and were instructed to adjust working conditions when
using a computer translated into the improvement of all parameters
used to assess the condition of the ocular surface.
The mean OSDI (Ocular Surface Disease Index) concerning
subjective ocular manifestations, environmental factors and
visual function improved, with the value decreasing from 25.242
to 12.346, i.e. by approx. 50% compared to baseline. Fariselli et al.
also demonstrated OSDI values to be reduced by 20% [21]. Fondi
et al. reported OSDI reduction, but the change was not statistically
significant [22]. In the present analysis the mean non-invasive tear
break-up time (NIBUT) improved by 17% - from 13.126 seconds to
15.403 seconds. Fondi et al. and Fariselli et al. also demonstrated
an improvement concerning tear film break-up time [21,22].
Schirmer’s test result improved, as it increased from 14.84±2.49
seconds to 16.07±2.02 seconds. Such an increase was not reported
by [21,22]. Normal osmolarity values of the tear film range from 296
to 302 mOsm/l in healthy individuals [19].The mean osmolarity was
300.83±11.68 mOsm/l. Yazici et al. conducted a study in which they
obtained 306.6±14.9 mOsm/L at the beginning of a working day
and 311.0±12.5 mOsm/L at the end of a working day in computer
users [23]. The present study showed the mean NIBUT before drop
administration in office workers to be 13.13±3.13 seconds, which
is normal.
A similar result was obtained by Unlü et al. who reported the
mean non-invasive tear break-up time at 11.37±3.69 seconds [20].
It may be compared with the results obtained by Uchino et al. The
mean non-invasive tear break-up time (NIBUT) was 4±2.5 seconds
which meant advanced dry eye syndrome [16]. The fact that our
patients used lubricating drops including trehalose 3% and sodium
hyaluronate 0.15% and observed appropriate working conditions
when using a computer caused the improvement of all parameters
used to assess the condition of the ocular surface. The mean OSDI
decreased from 25.24 to 12.34, i.e. by approx. 50% compared to
baseline. Fariselli et al. also demonstrated OSDI values to be reduced
by about 20% in computer users [21]. Fondi et al. demonstrated
a reduction in the OSDI index from 37.3±21.4 to 36.1±21.5 after
using a lubricating gel including trehalose, sodium hyaluronate
and carbomer and to 33.4±20.2 after the application of lubricating
drops including sodium hyaluronate. The measurements were
performed after 1 week of using lubricating agents. However, the
changes were not statistically significant [22].
A more marked improvement in the OSDI index observed in
the present analysis may be due to the implementation of suitable
work hygiene combined with the use of lubricating drops. In the
present analysis the mean non-invasive tear break-up time (NIBUT)
improved by about 17% - from 13.13 to 15.40 seconds. Fondi et al.
also reported an improvement in the tear film break-up time (BUT)
from 3.5±1.7 seconds to 4.2±1.7 seconds after using a lubricating
gel and 4.3±1.9 seconds after using lubricating drops for 1 week
[22]. Similarly, Fariselli et al. observed a 20% increase in the
tear film break-up time (BUT) compared to baseline values [21].
Schirmer’s test result improved, as it increased from 14.84±2.49
seconds at baseline to 16.076±2.02 seconds at the end of the study.
Such an increase was not reported by Fariselli et al. and Fondi et al.
(a change from 11.6±9.6 to 11.0±9.2 seconds) [21,22]. The present
study showed the mean osmolarity result to be within normal
limits (300.83±11.69 mOsm/l). The implemented drop regimen
and suitable working conditions contributed to its improvement,
i.e. a reduction to 292.30±9.49.
The reduction in osmolarity level causes better stability of
the tear film, lower evaporation of the tear film, and the resultant
alleviation of symptoms associated with dry eye syndrome and
computer vision syndrome [24]. Corrales et al. demonstrated a
beneficial influence of using lubricating drops by the reduction
in osmolarity, homeostasis improvement on the ocular surface
and the alleviation of undesirable symptoms associated with dry
eye syndrome [25]. The present paper demonstrated a positive
influence of the use of lubricating drops and the modification of
working conditions, i.e. adequate distance between the eyes and
the screen (65-80 cm), taking breaks every 30 minutes during
work and fixing one’s eyes on a distant object, frequent blinking,
suitable lighting, appropriate temperature and humidity in the
workplace. All the parameters were measured under the same
conditions (temperature, humidity, the same time during the day –
the afternoon). All the participants were using the same lubricating
drops for the same period and received identical recommendations
regarding the adjustment of working conditions. Further research
requires an analysis including a double-blind trial with a lubricating
drop group and a placebo group (e.g. with 0.9% normal saline
solution) and the comparison of the influence of lubricating drops
and modified working conditions on the ocular surface. Moreover,
it is worth studying various types of lubricating preparations in
patients with computer vision syndrome.
Conclusions
A large amount of time spent in front of a screen may cause serious consequences for the eyes leading to severe dry eye syndrome and all the related consequences including the deterioration of vision and the subsequent irritability, frustration, and even depression among computer users. It may be prevented by the appropriate diagnosis of ocular surface disorders, using proper eye lubricating substances and the modification of working conditions when using a computer.
Acknowledgement
The authors thank all volunteers for participating in the study. The study was funded from the present authors’ own resources.
Disclosure
Approval of the research protocol: N/A. Informed consent: All participants signed an informed consent for the original trial. Registry and the Registration No. of the study/trial: N/A. Animal Studies: N/A. Conflict of Interest: The authors declare no conflicts of interest.
Author’s Contributions
KEN had the idea for the study and developed the study design with KN. KEN performed the analyses and wrote the first draft of the article together. JPSz contributed with her expertise in all steps. All authors critically reviewed and approved the final manuscript.
References
- ÇalÕúkan HK (2015) Technological Change and Economic Growth. Procedia - Social and Behavioral Sciences 95: 649-654.
- Blehm C, Seema Vishnu, Ashbala Khattak, Shrabanee Mitra, Richard W Yee, et al. (2005) Computer vision syndrome: a review. Surv Ophthalmol 50(3): 253-262.
- Loh K, Redd S (2008) Understanding and preventing computer vision syndrome. Malays Fam Physician 3(3): 128-130.
- Fujita H (2019) Blind working time in visual display terminal users. J Occup Health 61(2): 175-181.
- American Optometric Association. Computer vision syndrome (CVS).
- Mylona I, Emmanouil S Deres, Georgianna Despoina S Dere, Ioannis Tsinopoulos, Mikes Glynatsis, et al. (2020) The Impact of Internet and Videogaming addiction on adolescent vision: A Review of the Literature. Front Public Health 8: 63.
- Ozcura F, Aydin S, Helvaci MR (2007) Ocular surface disease index for the diagnosis of dry eye syndrome. Ocul Immunol Inflamm 15(5): 389-393.
- (2007) Methodologies to Diagnose and Monitor Dry Eye Disease: Report of Diagnostic Methodology Subcommittee of International Dry Eye Workshop. Ocul Surf 5: 108-123.
- Rossi GCM (2019) Prevalence of dry eye in video display terminal users: a cross-sectional Caucasian study in Italy. Int Ophthalmol 39(6): 1315-1322.
- Rosenfield M (2011) Computer vision syndrome: a review of ocular causes and potential treatments. Ophthalmic Physiol Opt 31(5): 502-515.
- Daum (2004) Productivity associated with visual status of computer users. Optometry 75: 33-47.
- Bartoszek A, Szalast K, Kardas G (2019) Computer Vision Syndrome among undergraduate dentistry students. Journal of Education,Health and Sport 9(6): 407-414.
- Nakamura S (2010) Lacrimal hypofunction as a new mechanism of dry eye in visual display terminal users. PLoS One 5(6).
- Sezen Akkaya. Prevalence of Dry Eye Disease and its Risk Factors in Visual Display Terminal Users: The Osaka Study.
- Uchino M (2013) Prevalence of dry eye disease and its risk factors in visual display terminal users: the Osaka study. Am J Ophthalmol 156(4): 759-766.
- (2007) The epidemiology of dry eye disease: report of the Epidemiology Subcommittee of the International Dry Eye WorkShop. Ocul Surf 5(93): 1-7.
- Lemp MA (2011) Tear osmolarity in the diagnosis and management of dry eye disease. Am J Ophthalmol 151: 792-798.
- Gilbard JP, JB Carter, DN Sang, MF Refojo, LA Hanninen, et al. (1984) Morphologic effect hyperosmolarity on rabbit corneal epithelium. Ophthalmology 91(10): 1205-1212.
- Tomlinson A (2006) Tear film osmolarity: determination of a referent for dry eye diagnosis. Invest Ophthalmol Vis Sci 47(10): 4309-4315.
- Unlü C (2012) Comparison of ocular-surface disease index questionnaire, tearfilm break-up time, and Schirmer tests for the evaluation of the tearfilm in computer users with and without dry-eye symptomatology. Clin Ophthalmol 6: 1303-1306.
- Fariselli Ch (2018) Trehalose/hyaluronate eyedrop effects on ocular surface inflammatory markers and mucin expression in dry eye patients. Clin Ophthalmol 12: 1293-1300.
- Fondi K (2018) Effect of Hyaluronic Acid/Trehalose in Two Different Formulations on Signs and Symptoms in Patients with Moderate to Severe Dry Eye Disease. J Ophthalmol 6.
- Yazici A (2015) Change in tear film characteristics in visual display terminal users. Eur J Ophthalmol 25(2): 85-89.
- Lemp MA (2011) Tear osmolarity in the diagnosis and management of dry eye disease. Am J Ophthalmol 151(5): 792-798.
- Corrales RM (2008) Effects of osmoprotectants on hyperosmolar stress in cultured human corneal epithelial cells. Cornea 27(5): 574-579.

 Review Article
Review Article