Abstract
Introduction: Surgery is the first-line treatment for athletes with anterior cruciate ligament tear and who want to regain their preinjury sport level. The main determinants of recovery are joint stability, muscle recovery, and restoration of functional skills. Joint stability is provided by surgery, but there is little information on muscle and functional recoveries. While different surgical techniques are now established and well documented, recovery of muscle properties is not well understood, and few explorations have been done. Currently there is no consensus on the time frame for resuming sports activities after anterior cruciate ligament reconstruction (ACLR), nor on the means of objectifying it. Nevertheless, at 9 month post-operatively there is a great disparity observed in the levels of muscle recovery or reinjury. Anticipating patient status evolution would allow more personalized and adapted rehabilitation. The aim of this study is to test the ability of preoperative and 3 months postoperative measurements to predict neuro-muscular recovery at 9 months postoperative. To that end, trophic (MRI), mechanical (peak torque, work) and neuromuscular (RMS and median frequency) measurements will be performed in sportive subjects followed-up from before surgery to 9 months post-ACLR.
Methods and Analysis: This study is a prospective single-center study, with 3 repeated assessments at 0 (pre-operative), 3, and 9 months post-ACLR. 40 patients will be included. 40 healthy subjects will be also enrolled in a single visit as a control group. At each visit, thigh muscle properties will be explored through MRI imaging, isokinetic tests in isometry and dynamic conditions synchronized with surface electromyogram. Questionnaires (IKDC, ARPEGE), and a functional test (COFRAS) will be conducted. All will be crossed to neuromuscular adaptation, muscle strength and fatigue.
Discussion: The combination of all these elements coupled with longitudinal monitoring aims to better understand neuromuscular evolution, provide objective criteria for the RTS and propose guidelines for rehabilitation. Depending on the evolution of patients at each stage, it would be interesting to propose a personalized re-athletization according to the patient profile.
Strengths and Limitations of This Study:
a) This trial includes pre- and post-surgical assessments.
b) This study offers long term follow up (9 months) on technical measurements.
c) This trial includes a control group of healthy subjects to establish reference
values.
d) This study will include highly motivated population to return to preinjury sport
level (recreational athletes).
e) Physiotherapy protocols could not be standardized. Each patient will follow
usual rehabilitation program.
Keywords: ACLR; RTS; Disuse; RMI; Isokinetic; SEMG; Functional Skills
Abbreviations: BPTB: Bone To Patellar Tendon Bone; RTS: Return To Sport; IKDC: Isokinetic Tests in Isometry and Dynamic Conditions Synchronized with Surface Electromyogram; V1: First Visit (V1); V2: Second Visit; V3: Third Visit; RF: Rectus Femoris; VL: Vastus Lateralis; VM: Vastus Medialis; BFL: Biceps Femoris Longus; BFB: Biceps Femoris Brevis; ST: Semi- Tendinosus; SM: Semi Membranosus.
Introduction
Of the injuries that can lead to surgery, knee sprain with ACL
rupture is common, with a reported incidence of 60 to 71 per
100,000 subjects [1]. ACL tearing involves joint instability that
leaves a vulnerability to reinjury or early osteoarthritis. ACL
reconstruction (ACLR) is useful for joint stability restoration and
highly indicated in young athletes who want to regain their sport
level (prior level before injury). But surgery can lead to muscle
disuse and disorders particularly during the 3 first months [2], with
a high risk of iterative injuries [3]. Lower limb function is altered at
different levels (muscle strength, trophicity fatigability and neural
drive,) and these alterations remain until functional recovery [4,5].
Factors influencing recovery after ACLR are numerous and
interconnected, but they can be divided into three axes: joint
stability [6], joint mobility [7] and muscle recovery [8]. ACLR
is now mature and well documented, it permits the return to
effective joint stability by erasing post-traumatic laxity. Mobility
is usually sufficient for daily life but a postoperative re-athletizing
is necessary for sportsmen [9]. Currently, return to sport (RTS) is
allowed at 6- post-operative month in the absence of instability or
mobility complications [10,11]. At this postoperative time frame,
even though biological integration of the graft is supposed to be
efficient, Grindem et al. showed that patients who returned to
high level sports had [4,3]. times higher reinjury rate compared to
non-injured athletes [12]. Previous studies showed that re-injury
frequency can reach rate of 22 to 35.7% [13,14] much more, the
longer the convalescence is, the lower the risk of recurrence is.
Grindem et al. showed that the reinjury rate was significantly
reduced by 51% for each month RTS was delayed until 9 months
after surgery, after which no further risk reduction was observed
[12]. Thomeé et al. showed at two years only 23% of operated
subjects have a lower limb symmetry index (LSI) greater than
90% [15]. So far, there is no consensus on most relevant criteria
to RTS [10, 15-18] whereas an optimal restoration of thigh muscle
properties is necessary to prevent recurrences [12].
For that, the main time of rehabilitation takes place during the
first three months after surgery [19]. Then, the re-athletization
begins (3 to 6 post-operative months), under the cover of the
validation by the surgeon. Usually patients use cycling, swimming
or running retraining, well tolerated, but insufficient for return to
previous level.20 A complete recovery of muscular capacities then
makes it possible to pretend to prepare a new step: the specific
relearning linked to the practice of sport, in pivot, in pivot-contact,
jumps, etc. There is therefore a new period from the sixth to the ninth
post-operative month. Moreover, there are several patients with
high risk level of recurrence at 9 months.21 The speed of recovery
remains dependent to recovery of various muscle properties
(trophicity, strength, power and fatigue resistance) and age [21,22].
On the one hand, a slow progression leads to demotivation and fixes
the apprehension of injury risk. On the other hand, an accelerated
progression -with premature RTS- significantly increases the risk of
re-injury[10-12,23,24]. It therefore seems reasonable to delay the
resumption of sport from 6 to 9 months. However, there are still
disparities in recovery at 9 months, and in fact, the return to sport
is often delayed by patients themselves [11,18].
In addition, deciding when RTS becomes possible is important
for patient satisfaction and safety. This is a challenge in the context
of secondary and tertiary prevention.The aim of this study is
to test the ability of preoperative and 3 months postoperative
measurements to predict neuro-muscular recovery at 9 months
postoperative. Trophicity is commonly assessed using a simple
thigh perimeter, by comparing injured leg to non-injured leg. Such
methodology does not take into account either the variation in noninjured
leg, or the variation in fat mass and lean mass and muscles
predominantly affected.The intrinsic characteristics of muscle
(such as strength, fatigability, neuro-muscular recruitment), must
be evaluated collectively to provide guidelines for rehabilitation.
For example, evaluating the maximum force does not inform about
fatigue resistance. Moreover, the rehabilitation program can impact
differently these muscle properties.Additionally, since hamstrings
knee control is mainly ensured by the quadriceps-hamstrings pair,
evaluation of the later muscle group is a crucial issue.
Whereas quadriceps evaluation is the reference, this is not
systematically the case for hamstrings. If historically the first autografts were bone to patellar tendon bone (BPTB), it is criticized
for its donor site morbidities such as anterior knee pain, patellar
fracture, and quadriceps rupture [25]. Due to those morbidities,
the recent trend is shifting toward the hamstring tendon graft. It is
therefore natural to combine the same measures for quadriceps and
hamstrings that can be impacted by grafting. Finally, kinesiophobia
and functional performance are essential to ensure follow-up to
guide the patient in his recovery. Self-questionnaires and functional
test are needed concurrently for a complete evaluation of patient’s
situation.Our strategy is therefore to use the most efficient
measurement methods for trophicity, strength and recruitment, by
means of are MRI, isokinetism and EMG respectively. The question
of muscle recovery is a precondition for functional performance and
so RTS. The challenge of RTS and the difficulty of muscle recovery
therefore raise questions about their relationship.
The WEAKNESS Study Aims to Provide Quantitative and Qualitative Elements
a) An evaluation of muscle trophicity by MRI measurements,
taking into account the evolution of the contralateral member
as well as the fat mass evolution.
b) An evaluation of the maximal voluntary isometric force
and in parallel of the dynamic force and total work (fatigue).
c) An evaluation of neuromuscular recruitment by surface
electromyogram during force measurements.
d) Questionnaires and a functional test explore kinesiophobia
and the functional quality of knee motor skills.
The combination of all these elements coupled with longitudinal monitoring aims to better understand neuromuscular evolution, provide objective criteria for the RTS and propose guidelines for rehabilitation. Depending on the evolution of patients at each stage, it would be interesting to propose a personalized re-athletization according to the patient profile.
Population and Methods
The present study is a prospective single-center study, with repeated measures at 15 days pre-surgical, 3 and 9 months postoperatively after ACLR. The control group have a single visit. The research started in May 2018 and is due to be completed in July 2020.
Patient and Public Involvement
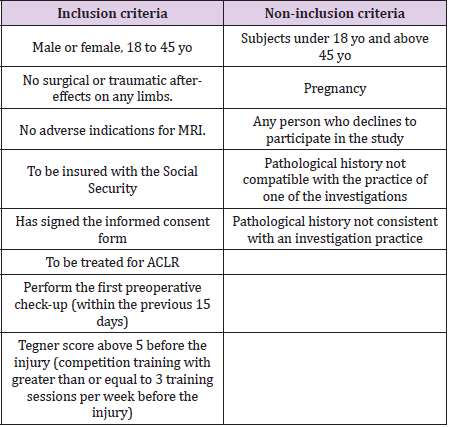
here are two groups: Operated group (OG) and Healthy group (HG), with 40 persons each. Patients of group OG will be enrolled among the patients of the Military health Teaching Hospital of Brest (orthopaedic surgery unit), and the orthopaedic surgery and traumatology department of local private clinics (Keraudren and Pasteur, Brest). Criteria for inclusion/exclusion are shown in Table 1. Patients are offered to participate at their own discretion in the WEAKNESS study. Our experience of 15 years of isokinetic evaluation after ACLR has confronted us with several recurring questions from patients. The design of this study takes up a certain number of them, such as the level of muscle recovery and physical activities that can be performed, in accordance with post-operative period. The objective of this study is to clarify the conditions of RTS which is a major issue for patients.
Patients Involvement
Participation to this study is proposed during the preoperative orthopaedic consultation, during which patients receive all information about this trial. Once the informed consent has been signed, patients are involved.
Volunteers Involvement
Participants of HG will be recruited through a poster and flyer campaign targeting the university or in sports medicine practices for civilians, and during employment readiness visits for military personnel. All study patients will undergo postsurgical rehabilitation. Nevertheless, rehabilitation after ACLR is well described nowadays, is the subject of recommendations and is common enough to be relatively homogeneous. Regular monitoring of surgeons makes it possible to detect patients in difficulty, in conjunction with physiotherapists. We note the number of reeducation sessions carried out and their location (in a rehabilitation center or in a private office). At each visit, each patient or public (volunteers), receive a complete review of isokinetic assessment by the investigator. This document specifies presence or absence of abnormality and the need for specialized consultation to answer them (for e.g. surgery, physiotherapist).
Study Design
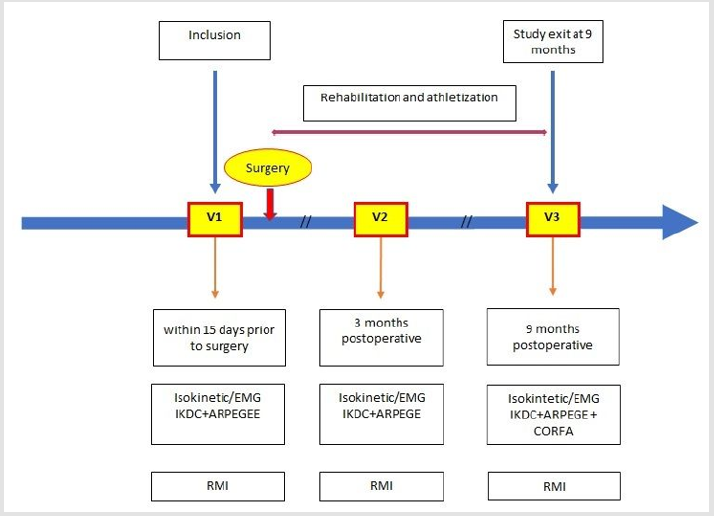
Measurements are realized during visits at the Military health Teaching Hospital of Brest. There is one visit for HG subjects and three for each OG patient. For OG subjects, first visit (V1) occurs within the two weeks before the surgery, second visit (V2) at 3 months postoperative and third visit (V3) at 9 post-operative months. The study design is presented in Figure 1.
Assessment Method
Population Descriptive Statistics
For HG, age, gender, BMI, sport level, education level, sport practiced, and dominant side are collected. The same variables are also collected for OG, along with sport level before injury and ‘surgical’ variables as time between injury and surgery, sprain mechanism, per-operative damage inventory, type of surgery, additional surgical procedures, tourniquet time, conditions of trauma, and anesthesia type.
MRI Assessment
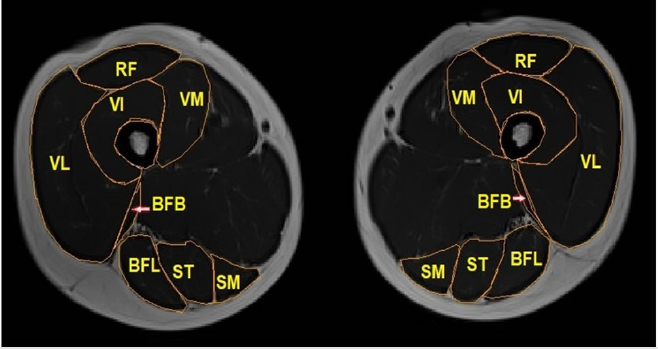
Figure 2: Intermediate thigh MRI slice with RF= Rectus Femoris; VL= Vastus Lateralis; VM= Vastus Medialis; BFL= Biceps Femoris Longus; BFB= Biceps Femoris Brevis; ST Semi-Tendinosus; SM= Semi-Membranosus.
MRI is a non-invasive and non-radiating imaging modality that provides objective data on patients’ muscle condition26. All the MRI scans were performed using Magnetom Avanto fit 1.5T (Siemens Healthineers) with a 16-channels body coil. Each subject will be installed on a device specially designed for the project, providing optimal installation and measurement reproducibility. MRI imaging of thigh muscles provides objective data on patients’ muscle condition in a non-invasive method [26]. Measures are centered on three muscle chiefs, not impacted by surgery: vastus medialis, vastus lateralis and biceps femoris. Segmentation is showed in Figure 2.
Semimembranosus (SM) and semitendinosus (ST) are only segmented on middle slice to allow hamstrings torque normalization. We use 2 types of sequences: T1 SE (thick sections: (TR : 490 ms, TE : 25 ms, cutting thickness : 10 mm) and T2 ME (TR : 2000 ms, TE : 22, 44, 66, 88, 110 and 132ms, cutting thickness : 4 mm). Image processing software is MIPAV V7.4.0. for T1 spin echo (T1SE) and T2 multi-echo (T2ME) with MR-map V1.4. Slices are centered by a marker placed on the skin and located at middistance from the base of the patella and the anterior superior iliac spine (ASIS), with a 6 % withdrawal towards the knee to avoid overflowing on the gluteal muscles. T1 SE allows measuring the cross-section area, muscle volumes, muscle fat involution by Gouttalier score [27], thigh muscle circumference (muscle minus skin and adipose tissue), total thigh volume, all in localization of interest (half distance ASIS-patella minus 6%, from patella). T2 ME allows visualizing the T2 weighted MRI images (48 sections) is performed by the MR-Map V 1.4 software. We obtain the transverse relaxation time T2 in milliseconds which can vary according to the physico-chemical organization of the water in the tissue [28].
Clinical Knee Testing and Measurements
A systematic clinical examination is performed at each visit on both knees. It consists of Lachmann’s test, knee front drawer and jerk tests, swelling, meniscus exploration, and thigh circumference. KT 1000 laxity assessment is performed at V1 and V3. We test both limbs for each participant. After testing zeroed position with three knee back drawers, the standard procedure is to perform three knee front drawer tests. The KT1000 gives audible indications of the actual traction level at 15, 20, and 30 pounds (lbs). The value selected is the difference between each limb for 30-pound load traction.
Questionnaires
As in the vast majority of ACLR studies, IKDC test is used [29]. IKDC score within 15 % of healthy gender–age-matched subjects relate good condition for RTS. The IKDC is the only score which is correlated with instrumental laxity evaluations (KT1000) [30]. IKDC is more sensitive to instability [31]. We add the ARPEGE French score, which is centered on the RTS. It explores three areas: mobility, stability and fatigue resistance during sports activities [32]. It ranks the score according to the following distribution: competitive, recreational, active, sedentary [31] IKDC is more sensitive to pain, while ARPEGE is more sensitive to kinesiophobia [31].
Functional Knee Test
We choose to include COFRAS functional knee test [33] for OG at the last visit (V3). This score is useful for assessing the ability of patients to participate in a sporting activity, but would have been very poor and difficult for patients to achieve during the first two visits. The structure of this test is divided into three axes: frontal and rotative stability (10 points), strength and apprehension, both on one leg (12 points), and finally functional activities of the knee joint (8 points). A total of 30 points ensure abilities to practice pivoting or jumping activities.
Isokinetic Assessment
After a standardized warm-up (10 minutes on ergo-cycle at 60 -70 rpm at a power equivalent to the subject’s weight, 1 Watt/Kg) [34-36], dynamometer measures will be performed on Con-Trex MJ® (CMV AG, Dübendorf, Switzerland). The isokinetic quadriceps and hamstring muscle strength assessment will be performed last, as the resulting tiredness could affect the other tests if performed first. This will be done on a Con-Trex Multi-Joint dynamometer (CMV AG, Dübendorf, Switzerland) and controlled by Con-Trex Software. The installation is described elsewhere in the literature, [34-36] and respect the protocol we use for 15 years. The participants will be seated with backrest at 85° and doubled-strapped in place at chest, pelvis and specific one on distal third of the thigh to avoid postural compensation during assessment. Contralateral limb will be free to move, and arms are bent over the chest to avoid compensation and the risk of strain on the lumbar spine. The axis of the dynamometer will be aligned with the rotation axis (lateral femoral epicondyle) of the knee joint. We use the double counter-base provided with the Con-Trex to attach the leg to the dynamometer arm. It makes possible to suppress anterior drawer induced by quadriceps contraction. This avoids constraints on surgery, prevents onset of pain or inhibition reactions and provides patients with a sense of security. The range of knee motion will be set from 82° (+/-0.8°) for a safe, comfortable, comparative assessment of quadriceps (extensor) and hamstring (flexors) muscles. Assessment will begin on the healthy knee, and then on the injured knee, and each series of repetitions will be followed by 1 min of rest.
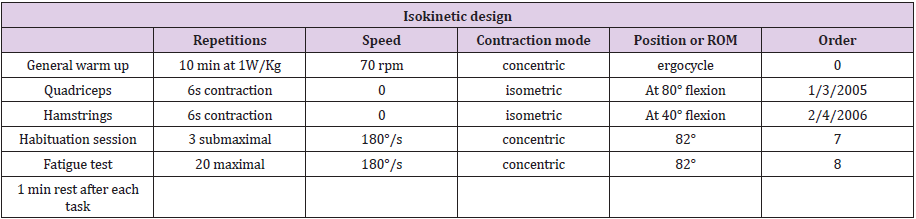
Dynamic isokinetic assessment will be performed using gravity corrections, at a range of motion of 16°-98° and measuring peak torque for each test session. A gravity correction is performed before the measurements of each lower limb, as well as the calibration of the goniometer and dynamometer. SEMG calibration is performed afterwards. The test measurements consist in performing, first, isometric tasks and, second, dynamic tasks as indicated in Table 2.
a) Measurement of the maximum voluntary isometric
force of the quadriceps: working angle fixed at 80° of flexion,
horizontal reference to 0° given by Con-Trex®. Three 6-s test
measurements at maximum voluntary contraction (MVC) with
verbal encouragements given to the participant are completed,
interspersed with 1-min rest period.
b) Measurement of the maximum voluntary isometric
hamstring force: working angle fixed at 40° of flexion,
horizontal reference at 0° given by Con-Trex®. Three 6-second
test measurements at MVC with verbal encouragements given
to the participant are performed, interspersed with 1-min
rest period. The tests for the quadriceps and hamstrings are
alternated.
c) Dynamic measurements of work/fatigue: one 180°/s
trials of three submaximal repetitions to learn the action
followed by 60 seconds rest. Then the participant carries out
the 180°/s test of 20 maximal repetitions with standardized
verbal encouragements.
Surface Electromyogram (SEMG) Assessment
SEMG recording is therefore synchronized in real time with the isokinetic device (tab 2 isokinetic test, tab 3 SEMG variables). A part of the seat on the dynamometer was especially designed for the experiments to prevent contact artifacts among EMG electrodes of the hamstrings. For each leg tested, the electrodes are placed on the Vastus lateralis (VL), Vastus medialis (VM), and biceps femoris (BF). Thought technology’s Flexcomp® system includes:
a) A SEMG signal capture box with 10 high-speed channels
(2048 samples) with 14 bits of resolution (1 part in 16364).
b) 3 preamplified Myoscan® sensors that pick up the SEMG
signal in raw form.
c) TT-USB receiver and USB cable for PC control.
d) A connection cable and its voltage isolator® box allowing
to recover the Con-Trex MJ® data in real time (position, speed
and torque).
e) Whole system is connected to a PC with the Physiology
Suite software suite© from Thought Technology Ltd to process
all data.
f) Each sensor has three electrodes. One sensor for the vastus
lateralis, one for the vastus medialis, and one for the biceps
femoris. Location of the electrodes is described in the SEMG
device manual. Installation of the electrodes is reproducible
using standard anatomical markers in reference to SENIAM.
Isokinetic measurements are therefore edited as report for the prescribing surgeon and on the other hand for the global collections of the study. We will retain the root mean square (RMS) and the median frequency (MedF) as an average value for the sixsecond isometric activity [29, 37 & 38]. For dynamic activities we take the average values of the RMS and MedF over the first 3 and last 3 contractions of the fatigue test. The time window will be 300 milliseconds centered on the peak torque. This will allow a recording of the same muscle area under the electrodes and limit the analysis at the time of peak torque.
Follow-Up After ACL Surgical Reconstruction
The patient’s follow-up ends 9 months after the operation. At the evaluation at 9 months post-surgery, patients will be questioned regarding their running activities, pivoting sport-specific training, pivoting sport competition, real level of sport achieved, as well as the date and the nature of any reinjury that may occur. The reinjury is defined as rupture of the transplant, or the contralateral ACL, or any injury requiring the sporting activity to cease and necessitating a consultation and/or medical care. We will also collect the Tegner score at 9 months post-ACLR. The decision for clearance to an RTS will be made by the surgeon, blinded to all the tests results except the isokinetics results. This decision will be taken after considering the time from surgery, clinical experience, and the isokinetics results.
Primary Outcomes
The main outcome measure, which is assessed at each visit is the muscle torque in Newton. Meter (Nm.). we will retain only the absolute peak torque, the most reproducible parameter [39]. The peak torque value normalized to the BW (Nm/kg) will be recorded for each mode and speed of contraction for the quadriceps (Q) and hamstring (H). Total work value normalized to the BW (Nm/ kg) will be recorded in dynamic condition for the quadriceps (Q) and hamstring (H). The Q/H ratio will be calculated for each mode and speed of contraction on the operated side, with a ratio ≥69% considered to be physiologically sufficient to obtain joint control [35].
Secondary Outcomes
Volume (cm³) and cross section area (CSA, cm²) of vastus lateralis (VL), vastus medialis (VM) and biceps femoris longus (BFL) will be assessed to evaluate trophicity and be normalized to isometric torque. The EMG signal of the same muscles will be measured. We will use the RMS (mV) and the medF (Hz). EMG will be normalized to CSA for each muscle. (VL, VM, BFL).
Statistical Analysis
The exploratory analysis of the data will be carried out with the support of the Clinical Investigation Center (CIC) of the University hospital of Brest. After ensuring the similarity and homogeneity of the HG and OG subgroups, the first step will be the HG analysis. We will establish the standard deviations expected in our study population for all measurement tools used. The statistical analysis will be performed using the software (IBM SPSS statistics). The isokinetic deficits and progress will be expressed in percentages of healthy limb results, idem for RMI and SEMG results. The average and the standard deviation for instrumental laxity will be calculated for first visit and 9 months after surgery and for queries at each visit. All factor’s interactions will be tested, and the significance level is set at p<0.05. Ordinary statistical methods will be employed, including means (X) and standard deviation on HG. Average SEMG RMS and medF values for the three muscles studied will be considered for analysis. In OG, to analyze differences in primary outcomes between each visit, a repeated measures ANOVA will be computed to identify significant differences for the dependent variables. After performing a correlation matrix and calculating collinearity using linear regression, we will calculate several generalized linear models if possible: linear regression, generalized estimating equations and generalized linear mixed model, depending on the characteristics of our variables.
Data Management, Monitoring and Quality Control
Data will be collected by investigator on a paper CRF and then collected and controlled by the Clinical Research Assistants (ARC) of Research Department of Military Teaching Hospital Clermont- Tonnerre, in accordance with the current protocol and regulations guarantying the anonymity of the patient.
a) Recruitment will be monitored by the Research
Department of Military Teaching Hospital Clermont-Tonnerre.
The sponsor (French Army Minister, DCSSA) will receive a
newsletter on a quarterly basis. Recruitment will be analyzed
after 9 and 15 months to identify unforeseen issues and
motivate centers to reach the recruitment goal.
b) Clinical Research Associates will have access to patients’
medical files and CRFs. Unscheduled inspections could also be undertaken.
c) Clinical Research Management Office of the Army
Biomedical Research Institute have the decision to submit the
report for publication, including ultimate authority over it.
d) Data extracted from measurements requiring postprocessing
such as SEMG signal, MRI segmentation, were
prepared by a training of the principal investigator. A double
reading was applied to ensure measurement reliability and
reproducibility. A randomized control of the files will be carried
out to ensure the quality of the data collection in the same way
during the study.
Study Statement
This study is actually ongoing.
Ethics Approval and Consent to Participate
The present study has been approved by the National ethical committee (approval number: 2017-A00301-52) and is recorded on Clinical Trials. Gov (ID: NCT03200678). Prior to enrolment in the study, all patients will be asked to give their written informed consent. Each patient can decide at any time to be released from the study, and they will be informed of this in the information flyer. His/ her data will then be deleted from the data collection file. Leaving the study will have no incidence on the normal monitoring protocol of patients’ post-surgery.
Consent to Publication
All data will be anonymous. All participants are informed and consent to the use of their data for the study and for publication. This is specified in the written consent document.The results of this study will be disseminated via presentation at local, national and international conferences and peer-reviewed journals.
Ethics and Dissemination
The results of this study will be disseminated through peerreviewed publications and scientific presentations. Ethical approval was registered prospectively and obtained through Comité de Protection des Personnes Sud-Méditerranée 3, approval number: 2017-A00301-52. Protocol 2.0 05/24/2019.
Declaration Section
a) Clinicaltrials.gov
b) Trial registration number: NCT03200678
c) Registered on June 27, 2017
d) Protocol version 1.5.
e) h t t p s : / / c l i n i c a l t r i a l s . g o v / c t 2 / s h o w /
NCT03200678?term=WEAKNESS&draw=2&rank=1
f) To access the data, please ask the author under the
authority of the Ministry of Army, Direction Centrale du Service des Armées, Santé des Armées 60 Boulevard du General Martial
VALIN CS 21623 75509 PARIS cedex 15
Funding
This research has governmental funding. It was supported by French Health Military Service, grant number [2017RC01], depending from French Army Minister. (Direction Centrale du Service de Santé des Armées, DCSSA, 60 Boulevard du Général Martial VALIN CS 21623 75509 PARIS cedex 15).
Authors’ Contributions
RG, FT, MG and MGAM designed the WEAKNESS study and contributed to development of the study protocol. RG, FT, FR and MAGM drafted the manuscript. RG submitted to ethic committee. All authors read and approved the final manuscript.
Acknowledgements
The authors are grateful to the study participants, HIA-CT Radiology Staff, HIA-CT MPR staff, HIA-CT Clinical research staff.
References
- Nordenvall R, Bahmanyar S, Adami J, Stenros C, Wredmark T, et al. (2012) A Population-Based Nationwide Study of Cruciate Ligament Injury in Sweden, 2001-2009: Incidence, Treatment, and Sex Differences. Am J Sports Med 40(8): 1808-1813.
- Andrade MS, Lira CAB, Vancini RL, Nakamoto FP, Cohen M, et al. (2014) Differences in muscle strength after ACL reconstruction do not influence cardiorespiratory responses to isometabolic exercise. Braz J Phys Ther 18(2): 144-151.
- Kamath GV, Murphy T, Creighton RA, Viradia N, Taft TN, et al. (2014) Anterior Cruciate Ligament Injury, Return to Play, and Reinjury in the Elite Collegiate Athlete: Analysis of an NCAA Division I Cohort. Am J Sports Med 42(7): 1638-1643.
- Chung KS, Ha JK, Yeom CH, Ho Jong Ra, Jin Woo Lim, et al. (2015) Are Muscle Strength and Function of the Uninjured Lower Limb Weakened After Anterior Cruciate Ligament Injury?: Two-Year Follow-up After Reconstruction. Am J Sports Med 43(12): 3013-3021.
- Neuman P, Kostogiannis I, Fridén T, Roos H, Dahlberg LE, et al. (2009) Patellofemoral osteoarthritis 15 years after anterior cruciate ligament injury-a prospective cohort study. Osteoarthritis Cartilage 17(3): 284-290.
- Mather RC, Koenig L, Kocher MS, Timothy M Dall, Paul Gallo, et al. (2013) Societal and Economic Impact of Anterior Cruciate Ligament Tears. J Bone Joint Surg Am 95(19): 1751-1759.
- Biggs A, Jenkins WL, Urch SE, Shelbourne KD (2009) Rehabilitation for Patients Following ACL Reconstruction: A Knee Symmetry Model. North Am J Sports Phys Ther NAJSPT 4(1): 2-12.
- Garrison JC, Hannon J, Goto S, Victor Kosmopoulos,Subhash Aryal, et al. (2019) Knee Loading After ACL-R Is Related to Quadriceps Strength and Knee Extension Differences Across the Continuum of Care. Orthop J Sports Med 7(10).
- Kvist J (2004) Rehabilitation Following Anterior Cruciate Ligament Injury: Current Recommendations for Sports Participation. Sports Med 34(4): 269-280.
- Barber Westin SD, Noyes FR (2011) Objective Criteria for Return to Athletics After Anterior Cruciate Ligament Reconstruction and Subsequent Reinjury Rates: A Systematic Review. Phys Sportsmed 39(3): 100-110.
- Ardern CL, Webster KE, Taylor NF, Feller JA (2011) Return to the Preinjury Level of Competitive Sport After Anterior Cruciate Ligament Reconstruction Surgery: Two-thirds of Patients Have Not Returned by 12 Months After Surgery. Am J Sports Med 39(3): 538-543.
- Grindem H, Snyder Mackler L, Moksnes H, Engebretsen L, Risberg MA (2016) Simple Decision Rules Reduce Reinjury Risk After Anterior Cruciate Ligament Reconstruction. Br J Sports Med 50(13): 804-808.
- Myklebust G, Holm I, Mæhlum S, Engebretsen L, Bahr R (2003) Clinical, Functional, and Radiologic Outcome in Team Handball Players 6 to 11 Years after Anterior Cruciate Ligament Injury: A Follow-up Study. Am J Sports Med 31(6): 981-989.
- Webster KE, Feller JA (2018) Return to Level I Sports After Anterior Cruciate Ligament Reconstruction: Evaluation of Age, Sex, and Readiness to Return Criteria. Orthop J Sports Med 6(8): 232596711878804.
- Thomeé R, Neeter C, Gustavsson A, Pia Thomeé, Jesper Augustsson, et al. (2012) Variability in leg muscle power and hop performance after anterior cruciate ligament reconstruction. Knee Surg Sports TraumatolArthrosc 20(6): 1143-1151.
- Petersen W, Zantop T (2013) Return to play following ACL reconstruction: survey among experienced arthroscopic surgeons (AGA instructors). Arch Orthop Trauma Surg 133(7): 969-977.
- Van Melick N, Van Cingel REH, Brooijmans F, Camille Neeter, Tony van Tienen, et al. (2016) Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med 50(24): 1506-1515.
- Dingenen B, Gokeler A (2017) Optimization of the Return-to-Sport Paradigm After Anterior Cruciate Ligament Reconstruction: A Critical Step Back to Move Forward. Sports Med 47(8): 1487-1500.
- Kvist J (2004) Rehabilitation Following Anterior Cruciate Ligament Injury: Current Recommendations for Sports Participation. Sports Med 34(4): 269-280.
- Dauty M, Menu P, Dubois C (2010) Effects of running retraining after knee anterior cruciate ligament reconstruction. Ann Phys Rehabil Med 53(3): 150-161.
- Ueda Y, Matsushita T, Shibata Y, Kohei Takiguchi, Akihiro Kida, et al. (2019) Longitudinal Quadriceps Strength Recovery After Anterior Cruciate Ligament Reconstruction With Hamstring Autograft: Patients Stratified by Preoperative Quadriceps Strength Deficit. J Sport Rehabil p. 1-20.
- Shibata Y, Matsushita T, Araki D, Akihiro Kida, Kohei Takiguchi, et al. (2019) Prediction of quadriceps strength recovery after anterior cruciate ligament reconstruction with a hamstring autograft: Decision tree analysis. J Orthop Sci 24(2): 301-305.
- Lutz C (2014) Critères de reprise du sport après reconstruction du ligament croiséanté J Traumatol Sport 31(3): 185-187.
- Nagelli CV, Hewett TE (2017) Should return to sport be delayed until two years after anterior cruciate ligament reconstruction? Biological and functional considerations. Sports Med Auckl NZ 47(2): 221-232.
- Kartus J, Movin T, Karlsson J (2001) Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthrosc J Arthrosc Relat Surg 17(9): 971-980.
- Ropars J, Gravot F, Ben Salem D, Rousseau F, Brochard S, et al. (2020) Muscle MRI: A biomarker of disease severity in Duchenne muscular dystrophy? A systematic review. Neurology 94(3): 117-133.
- Somerson JS, Hsu JE, Gorbaty JD, Gee AO (2016) Classifications in Brief: Goutallier Classification of Fatty Infiltration of the Rotator Cuff Musculature. Clin OrthopRelat Res 474(5): 1328-1332.
- Bonny JM, Zanca M, Boespflug Tanguy O, Dedieu V, Joandel S, et al. (1998) Characterization in vivo of muscle fiber types by magnetic resonance imaging. MagnReson Imaging 16(2): 167-173.
- Logerstedt D, Di Stasi S, Grindem H, Andrew Lynch, Ingrid Eitzen, et al. (2014) Self-Reported Knee Function Can Identify Athletes Who Fail Return-to-Activity Criteria up to 1 Year After Anterior Cruciate Ligament Reconstruction: A Delaware-Oslo ACL Cohort Study. J Orthop Sports Phys Ther 44(12): 914-923.
- Hrubesch R, Rangger C, Reichkendler M, Sailer RF, Gloetzer W, et al. (2000) Comparison of Score Evaluations and Instrumented Measurement after Anterior Cruciate Ligament Reconstruction. Am J Sports Med 28(6): 850-856.
- Chaory K, Poiraudeau S (2004) Les grilles d’évaluations dans la ligamentoplastie du LCA. Ann Réadapt Médecine Phys 47(6): 309-316.
- Cazenave M, Deloge F (2013) Étude prospective sur la reprise d’activités physiques de 20 militaires après ligamentoplastie du genou par prélèvement au niveau de la patted’oie. Kinésithérapie Rev 13(137): 13-19.
- Oria S (2010) Le score Cofras :évaluationfonctionnelle du genouavant reprise sportive. Kinésithérapie Rev 10(97): 27-31.
- Rochcongar P (2004) Évaluationisocinétique des extenseurs et fléchisseurs du genouenmédecine du sport : revue de la litté Ann Réadapt Médecine Phys 47(6): 274-281.
- Croisier JL, Ganteaume S, Binet J, Genty M, Ferret JM (2008) Strength Imbalances and Prevention of Hamstring Injury in Professional Soccer Players: A Prospective Study. Am J Sports Med 36(8):1469-1475.
- Busnel F, Rochcongar P, Andre AM, Beillot J, Jan J (2006) Exploration isocinétique du genou du judoka et risque de rupture du LCA. Àproposd’uneenquête prospective auprès des athlètes du pôle France de Rennes. Sci Sports 21(3): 148-153.
- Drechsler WI, Cramp MC, Scott OM (2006) Changes in muscle strength and EMG median frequency after anterior cruciate ligament reconstruction. Eur J Appl Physiol 98(6): 613-623.
- Bilodeau M, SchindlerIvens S, Williams DM, Chandran R, Sharma SS (2003) EMG frequency content changes with increasing force and during fatigue in the quadriceps femoris muscle of men and women. J Electromyogr Kinesiol 13(1): 83-92.
- Maffiuletti NA, Bizzini M, Desbrosses K, Babault N, Munzinger U (2007) Reliability of knee extension and flexion measurements using the Con-Trex isokinetic dynamometer. Clin PhysiolFunct Imaging 27(6): 346-353.

 Research Article
Research Article