Abstract
The present study is a standalone piece of work in this area where the association of mother’s Diabetes Mellitus (DM) and Congenital Heart Disease CHD of children were investigated. The present study was carried out in two hospitals in Dhaka city from June to December 2019. A total of 78 neonatal admitted children having heart disease were to the hospitals for treatment and was taken as study samples. The study applied logistic regression analysis and reported the odd ratio to identify the possible covariates that affect CHD. The present results represent that only 73% of the neonate had CHD problem, 85% of the neonate had cyanosis, 41% had resuscitation, 38% had chest inside, 33% showed murmur sound, 18% had GHTN and only 1% had Eclampsia. The present study identified that 63% of the neonate had Patent Arterial Duct (PDA) found in the ECHO results whereas Atrial Septal Defect (ASD) (67%) and Ventricular Septal Defect (VSD) (25%) were also found. Mothers were found with Diabetic Mellitus (50%), 87% of the neonates of diabetic mothers were experienced CHD than the 59% CHD of neonates of the non-diabetic mothers. Odds ratio from the log, it model shows that there is a 5.8 times higher risk of CHD in neonates if the mother has diabetes. Besides, mother’s age possesses 1.14 times and unwanted event during pregnancy 4.2 times the risk of CHD among neonates. Also, the mother’s higher weight can significantly reduce this probability of CHD. It may be concluded that, the incidence of Congenital Heart Disease (CHD) in Bangladesh is increasing. A significant association was found with mothers and family characteristics. Diabetic mothers and aged mothers have more tendencies to give birth to neonates with CHD problems. Unwanted events increase the risk of CHD of neonates. Change lifestyle of mothers and timely pregnancy may reduce the risk of neonate CHD.
Keywords: Association; Diabetes; Congenital; Heart Disease; Neonate
Introduction
Congenital Heart Disease (CHD) is the most common lesion
among all types of neonatal disease in the world [1]. CHD is defined
as a gross structural abnormality of the heart or intra-thoracic great
vessels which potentially of functional significance [2]. Studies
found that the incidence of CHD varies from 4/1000 to 50/1000
live birth and the relative frequency of different types of major form
of CHD differs with variety of case context especially in stillbirth,
spontaneous abortion and prematurity [3,4]. It is frequently
reported that the CHD incidence is either constant or increasing
worldwide [5,6]. There is no nationwide survey on congenital
heart disease of neonate children in Bangladesh, however, different
studies suggest that the incidence of CHD in Bangladesh is around
18/1000, 15% in India, and 10% in Sri Lanka [6-8]. There are nine
common lesions that constitute the 80% of the CHD where 36%
Ventricular Septal Defect (VSD), 5% Atrial Septal Defect (ASD), 9%
Patent Arterial Duct (PDA), 9% Pulmonary Stenosis, 5% Aortic
Stenosis, 5% Coartation of Aorta, 4% Transposition of Great
Arteries, 4% Tetralogy of Fallot etc. [5].
CHD is the most common lesion among all types of neonatal
disease in the world. The exact causes of the congenital heart disease are not clear, literature have identified that CHD are thought to be
multifaceted and multi-factorial and results from a combination
of genetic predilection and environmental stimulus and severity
of the disease and needs different types of clinical interventions
for their survival [9,10]. The most common neonatal congenital
heart disease are cyanosis, heart failure, collapse, and abnormal
clinical sign identified by regular examination for example, absent
of femoral pulse or heart murmur sound [11]. The most common
problems are cyanosis, clubbing, murmur, syncope, squatting, heart
failure, arrhythmia, failure to thrive in the infant and children,
and adolescent and the adults present with heart failure, murmur,
arrhythmia, cyanosis hypertension, late consequences of previous
cardiac surgery.
The incidence of CHD depends on many factors including
biological factor, socio-economic factors, environmental factors,
healthcare system, and even on the national economy. Besides,
the CHD cases may also come from Down’s syndrome babies,
babies with diabetic mother, and babies with other congenital
malfunctions. It is a matter of fact that most cases of CHD die in
early infancy and some may manifest a delayed exposure. The
prevalence rate of CHD in Bangladesh population is not known as
there is no official representative survey in Bangladesh for that in
the recent years. There are some small-scale studies that shown
the prevalence rate of the CHD in that specific hospital, however,
the research suffers from sample size biasness and endogenecity
problem [12]. Several studies in Bangladesh reported that the
prevalence rate of neonatal CHD is close to 6 to 25 per thousand live
birth. Findings from the study based on the pediatric department
of Rajshahi Medical College and Hospital showed that children
from birth to until 12 years suffer from various CHD problems
specially VSD (42.6%), TOF (18.3%), ASD (14.8%), PDA (7.8%)
where murmur and cardiomegaly were the most important cardiac
findings [13].
Similar studies were found that 65.38% were acyanotic and
34.42% cases were cyanotic, with the commonest CHD of VSD-
33.33%, ASD-16.24%, TOF-11.54%, PDA -10.68% (Hoque et al.,
2014); another study based on the Department of Paediatric
Cardiology at National Institute of Cardiovascular Diseases, Dhaka,
found that VSD-27.2% and TOF-20.5%. A study based on neonate
children aged birth to 28 weeks gestational period were found
that ASD-26%, VSD-16.9%, PDA-18%, TOF-14%, PS-7.75% with
asymptomatic high-risk neonates contributing to early detection
of many trivial lesions [14]. The causes of CHD are assumed to
be associated with many other factors such as pregnancy factor,
mother’s diseases factors, father’s disease factors, socio-economic
characteristics, environmental characteristics and the healthcare
system of the location. In a study conducted in 2000- 2001, found
that diabetes mellitus of mother is associated with the infant’s CHD.
It was found that, pre-existing maternal diabetes is associated with
a fivefold increase in the congenital heart disease [15]. Until 2009,
a study in Norway confirmed that this association of CHD and DM
mothers is almost two to three fold than the non-DM mothers [16].
It is found that several researcher has identified the different type
of CHD of neonate children in Bangladesh [17-19].
Justification of the study: In cases of adverse pregnancy
outcome like complicated delivery, mother’s and baby’s illness
or in any emergency psychological effects of the participants had
been taken care of while asking question or collecting information.
In this context, this study is the unique and standalone piece of
research that studied the association of CHD of neonate children
and mothers’ diabetes after controlling for other socio-economics
characteristics and other health related variables.
Materials and Methods
A total of 78 children were selected who were admitted to the NICU for heart diseases. However, among them, not all children were detected CHD, rather other symptoms of respiratory problems. The mothers of the patients were interviewed based on their consent to take part in this study and their medical tests. The study examined their echocardiogram and other necessary examination, collected child and mother history of previous disease and mother’s diabetic situation. Observational data was collected in the study and logistic regression analysis was conducted for identifying the association among the variables. The target populations are those who visited at Bangladesh Institute of Health Science (BIHS) and Universal medical College Hospital during their pregnancy. In Outpatient department, the study was carried out from July, 2019 to December 2019. Purposive sampling technique was adopted for selecting respondents. A structural questionnaire was used for correlation of necessary information. A check list or medical records were done for assessment of three trimester pregnant women condition. The Anthropometric data (height and weight) was collected based on standard methods. Chi square test was done between categorical variables to show the association between dependent and independent variables. Logistic regression was used for multi variants analysis to control the potential confounding factors.
Results
Socio-Economic Factors
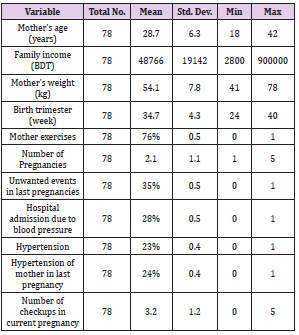
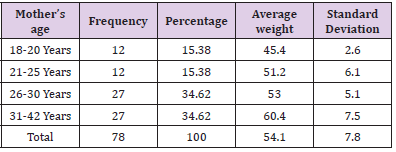
The history of the mothers of the patients include mother’s age, weight, doing exercise, number of pregnancies, unwanted pregnancy events, having hypertension, diabetes, health-seeking behavior, family history of hypertension, family income, neonatal congenital heart disease, types of heart disease, and different types of treatments (Table 1) . In the present study, it was found that 76% of the mother did exercise regularly during pregnancy. On average, there are 2.1 pregnancies for a mother in Bangladesh. About 35% of a mother faced unwanted events during the pregnancy such as abortion and other complications. 28% of the mothers had either high blood pressure or low blood pressure and they had to admit to the hospital. However, 23% of the mothers in the collected sample, had hypertension. On average there were 3.2 doctor’s checkups during the pregnancy (Table 1). Age and weight of mothers: In the present investigation, It was found that almost 70% of mothers were aged over 25 for their current pregnancies, 15% was found very young mothers who were aged 18 to 20 years and their average weight was 45.4 kg which was found to be lower weight according to WHO standard. The average weight of 26 to 30 years old mothers was 53 kg and the average weight of 31 to 42 years mother was 60.4 kg (Table 2).
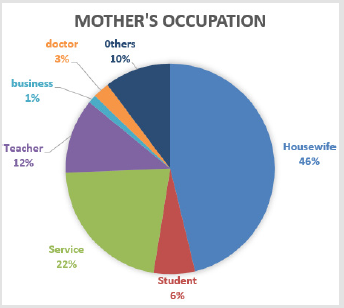
Mothers’ Occupation: Clinical Factors
It is found that 46% of the mothers were housewife and 22% of them were service holders. About 12% of them were teacher, 6% students and 3% doctor. There were other occupations (10%). Mother’s occupation is a valid socio-economic status as it may bring an association of mothers’ income status and have more frequently visited a doctor. This also suggests the connection with diabetes and congenital heart disease of children (Figures 1 & 2).
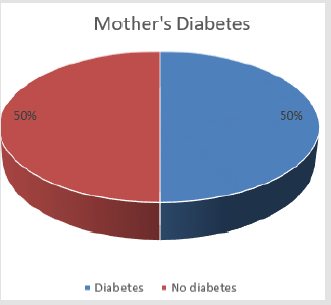
Mother’s Diabetes
To identify any association between the mother’s diabetes and the child ‘s CHD, it was assessed that 50% of the mother had diabetes during the pregnancy and the rest 50% didn’t had (Fig. 2), only those who suffered from diabetes in recent pregnancy were considered.
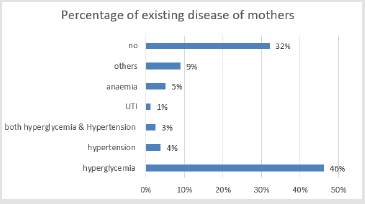
Mothers’ Existing Diseases During Pregnancy
It was found that mothers had different types of diseases during the pregnancy and they had to take medication and it was reported that almost 36 mothers (45%) among 78 had hyperglycemia which means the excess of glucose in the bloodstream. It was found, almost 4% of the mother having hypertension. Almost 5% of the women reported that they had anemia, 3% reported that they had both hyperglycemia and hypertension and 9% had with different other types of diseases. However, 32% of the women were found to have no current disease for which they needed medication (Figure 3).
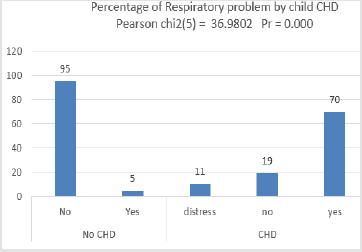
Types of Cardiac Problem by CHD Status
While investigating whether the child had Congenital Heart Disease (CHD) or not, based on the test result, it was found that among the CHD patients, 70% of them were affected by the respiratory problem, and 11% of them had distress during the observation. However, it was also found that 5% of the cases where the child had a respiratory problem but was not conclusive to have CHD status. On the contrary, 19% of the children found without any respiratory problem but was detected as CHD patients as they had other complications rather than the respiratory problem (Figure 4).
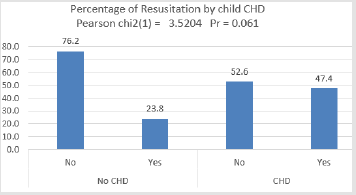
The analysis compared the types of Cyanosis problem by child CHD status, it was found that 24% of the children had no Cyanosis and were not detected as CHD patient and 4% had no Cyanosis but were detected as CHD. It was found that CHD patients had more problems with the peripheral and both peripheral and central cyanosis than the non-CHD patients. It reveals that CHD patients had more exposure to the cyanosis problem than non-CHD patients. The statistical difference of percentage of cyanosis between the CHD and non-CHD was significant as the Pearson Chi-square test value was above the critical value label and the p-value was less than 5% level (Figures 5 & 6): Percentage of Resuscitation by child CHD status (Table 3).
T The Percentage of Resuscitation by Child CHD
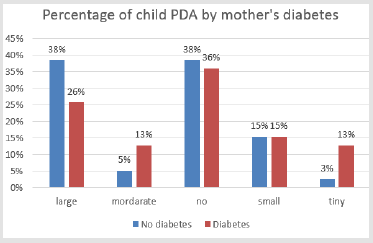
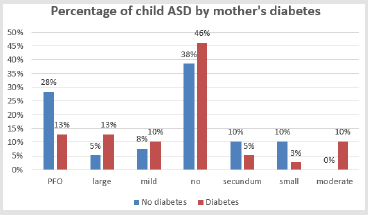
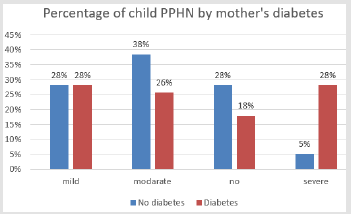
It is found that the percentage of resuscitation was higher in the CHD affected children than those of the non-C HD ci in children. Almost 24% of the resuscitation cases were not detected as CHD problem in the children (Figure 7). The percentage of resuscitation was higher in the CHD affected children than those of the non- CHD children. Almost 24% of the resuscitation cases were not detected as CHD problem in the children. The interaction of the mother’s diabetes and the child heart disease showed a significant relationship exists between these two factors. Child CHD was highly correlated with the mother’s diabetes representing 87.18% of the diabetic mothers’ children were affected by CHD. Diabetic mothers had more tendencies to have PDA children. Moderate and tiny PDA cases, diabetic mothers had a higher percentage of PDA than other PDA cases. Almost 64% of diabetic mothers had PDA affected children than non-diabetic mothers. It was found that the child ASD cases were positively correlated with the mother’s diabetes. In case of mild, moderate, and large ASD cases, the diabetic mothers had higher exposure rate than the non-diabetic mothers (Figure 8).
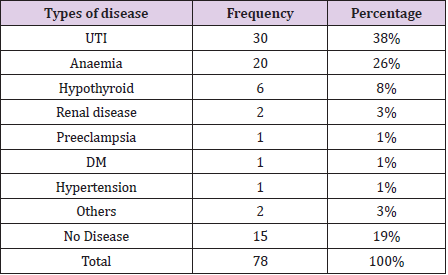
Mothers’ Co-Existing Diseases During Pregnancy
Mothers had also some previous existing diseases that the also reported. In most of the cases that most mother had both current and pre-existing diseases during the prepregnancy. One of the topmost co-existing diseases is the UTI and anaemia. It is reported that almost 38% of the women have UTI and 26% of the women had anaemia. Most of the women have this hyperglycemia and UTI and/or anaemia. Besides, 8% of them had hypothyroidism and 3% of them had renal disease. The co-existing diseases found very low diabetes counts and hypertension, which was most possible that those are mentioned in (Figure 3) for which the mother is already taking medicine.
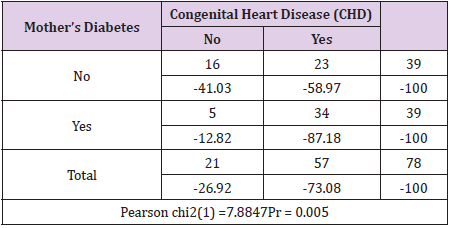
Congenital Heart Disease Among the Neonate of Diabetic Mothers
Mother’s diabetes and child CHD: The interaction of the mother’s diabetes and the child heart disease, there exists a significant relationship between these two factors. Child CHD was highly correlated with the mother’s diabetes. It was found that 87.18% of diabetic mothers’ children were affected by CHD. 12.82% of the mothers although having diabetes, their children were not affected by CHD. On the other hand, 59% of the non-diabetic mothers’ children were having CHD. The Pearson Chi-square test was significant (P<1%) which showed a significant association between the child CHD and mother’s diabetes (Table 4).
Mother’s Diabetes Status and the Child Cardiac Problem
The diabetic mothers had more tendencies to have PDA children according to the (Figure 7). Moderate and tiny PDA cases, the diabetic mothers had higher percentage of PDA than other PDA cases. Almost 64% of the diabetic mothers had the PDA affected children than the non-diabetic mothers. In the current study, PPHN and PDA were found to be the commonest CHD which was followed by ASD and VSD (Figure 9). However, this study has found that the PPHN (82%) and PDA (70%) is higher than any other studies mentioned here possibly because of the neonates who were admitted into the hospital and had these issues.
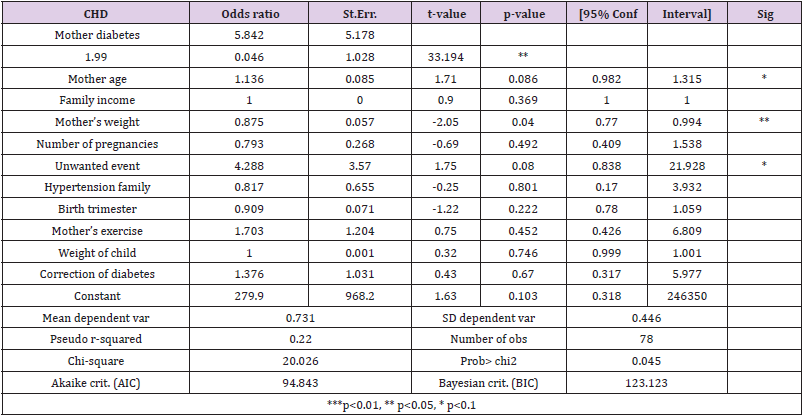
Regression Results
The study applied logistic regression model as the outcome variable was binary in nature (CHD=1, or 0). The presented odds ratio showed the likelihood of occurring the event due to the other independent variables. The study hypothesized that CHD is a function of the mother’s characteristics and household characteristics. There is a statistically significant association present between the CHD of neonatal children (within 28 days of age) and the mother’s diabetes. It shows that if the mother had GDM (diabetes) then the probability of having CHD of the neonate increases by 5.8 times higher than a non-diabetic mother which is significant at 5% level. Mother age was also found significantly associated with the CHD of the child. It shows that the aged mother tends to have the child with CHD 1.14% higher than a young aged mother which is significant at 10% level of significance. Mother’s weight is also found to have a significant negative association with the CHD of the child at 5% level of significance. It implies that mothers with higher weight tend to have non-CHD babies than the lower-weight mother counterpart. Mothers having unwanted event before the current pregnancy possess a significant positive association with the CHD of the child. It implies that if there is presence of unwanted event before the current pregnancy among the mothers, the probability of CHD among the neonatal babies increases by 4.3 times which is significant at 10% level. All these results are controlled for all other variables such as family income, the number of pregnancies, the record of family hypertension, birth trimester, mother’s doing exercise, weight of child, and correction of diabetes of mother etc. (Table 5).
Discussion
Congenital heart disease among the neonatal children was
identified the types of CHD problems. The incidence varies from
locality, region, exposure areas, and even the countries, however
most countries reported it to be 4/1000 to 50/1000 live birth [20].
Many studies also reported that it is increasing globally as well as in
Bangladesh [17,18]. However, in Bangladesh there is no nationwide
study on that however, different studies suggest that the incidence
of CHD in Bangladesh is around 18/1000. Literature has reported
that the causes of CHD is multifaceted and multidimensional and
results from a mixture of inherited predilection and environmental
impetus. Similar study was conducted at the Joslin et al in 1973
identifying a fivefold risk of CHD of neonate children of the DM
mothers than the non-DM mothers. The present investigation is
based on the conceptual analysis where it outlined that neonatal
congenital heart disease is linked with mother’s characteristics,
socioeconomic characteristics of the family, mother’s disease
profile such as records of diabetes, hypertension, hypothyroidism,
anemia, and UTI, and child characteristics such as child weight,
pregnancy delivery weeks (trimester) etc. Mother’s hypertension,
hypothyroidism and diabetes and anaemia also possess a great risk
towards the neonatal CHD. Mother’s occupation was a valid socioeconomic
status as it might bring an association of mothers’ income
status and having more frequently visited a doctor.
Early delivery of pregnancy could be one of the reasons for CHD.
It was found that most women had their deliveries at the week of 37. It was not surprising that few women (almost 5%) had delivery
before they reach at 28 weeks. This type of early delivery of the
baby causes congenital heart disease found in the literature. About
14% of the mother had their child delivery before 32 weeks of their
pregnancy; however, almost 5% told that they have late deliveries
of their babies. In the neonatal outcome, birth weight is one of the
important characteristics of CHD. It was found that almost 58%
of the sample size was born with low birth weight meaning less
than 2.5 kg which was an alarming signal. Only 30% of the sample
babies were born with being 2.5 to 3kg. So, in total it can be said
that almost 86% of the sample babies in this study was less than
3 kg when at birth. This is a clear indication that they would have
other complication later their life. A Healthy baby should have a
good birth weight (more than 2.5kg).
In the current study, PPHN and PDA were found to be the
commonest CHD which was followed by ASD and VSD. These
findings differs with the findings of but similar to. This study found
that acyanotic CHD was the commonest heart disease which was
also similarly found in many other studies ASD (67%) and VSD
(25%) were found in the study complies with other studies such
as. However, this study has found that the PPHN (82%) and PDA
(70%) is higher than any other studies mentioned here possibly
because of the neonates who were admitted into the hospital and
had these issues. It is also found that many neonatal had multiple
lesion which also confirmed by other studies such as.
Comparing the types of Cyanosis problem by child CHD
status, it has found that 24% of the children had no Cyanosis and
was not detected as CHD patient and 4% had no Cyanosis but
were detected as CHD. CHD patients had more problems with the
peripheral and both peripheral and central cyanosis than the non-
CHD patients. It revealed that CHD patients had more exposure
to the cyanosis problem than non-CHD patients. The statistical
difference of percentage of cyanosis between the CHD and non-
CHD was significant. The regression result showed that there was
a statistically significant association present between the CHD of
neonatal children and the mothers’ diabetes. This result is similar
to the results found in [21]. It showed that if the mother had GDM
(diabetes) then the probability of having CHD of the child increases
by 5.8 times higher than a non-diabatic mother which was
significant at 5% level. This result is similar to the studies of Where
Archives of Disease in Childhood (ADC) have found DM increased
the CHD by 5 times, found this relationship of DM increased the
CHD by 4 times. [22] discussed the mother’s diabetic factor as a
underlying cause, but didn’t identify the impact of it on CHD. The
Mother age also found significantly associated with the CHD of the
child. It showed that the aged mother tends to have a child with
CHD 1.14% higher than a young aged mother which was significant
at 10% level of significance.
Conclusion and Recommendation
The present investigation identified that, the association between the neonatal congenital heart diseases and the mother’s diabetic status based on some clinical and observational data from 78 randomly selected patients who got admitted to the Intensive Care Unit (ICU) during the study period. The sample was random because the researcher didn’t have any control who would come for the admission and who will not. The sampling was completely random. This result shows that there was a positive association among CHD and mother’s diabetes, age, and having unwanted events. On the other hand, the mothers’ weight had a negative relationship with the CHD of children. This study identifies the association between the neonatal congenital heart diseases and the mother’s diabetic status based on some clinical and observational data from 78 randomly selected patients who got admitted to the Intensive Care Unit (ICU) during the study period.
Acknowledgement
We like to express our sincere, deepest and heartfelt gratitude to the Faculty of Arts and Social Science, Public Health Department, American International University- Bangladesh, permitted and supported to conduct this research for the MPH courses. Permission was also taken from the Ethical Committee at American International University Bangladesh.
References
- Hoffman JI E, Kaplan S (2002) The incidence of congenital heart disease. Journal of the American College of Cardiology 39(12): 1890-1900.
- Abdulla (1997) What is the prevalence of congenital heart diseases. Pediatr Cardiol 18: 268.
- Fyler D, Buckley L, Hellenbrand W, Cohn H, Kirklin J, et al. (1980) Report of the New England Regional Infant Cardiac Program. Pediatrics 65(2): 375-461.
- Jordan SC, Scott O (1989) Heart Disease in Paediatrics (3rd Editio). Butterworth-Heinemann.
- Fatema N, Chowdhury R, Chowdhury L (2008) Incidence of Congenital Heart Disease among Hospital Live Birth in a Tertiary Hospital of Bangladesh. Cardiovascular Journal 1(1): 14-20.
- Naik S, Irshad M, Kachroo A, Ahmad M (2019) A study of prevalence and pattern of congenital heart disease at Sopore, Kashmir, North India. International Journal of Contemporary Pediatrics 6(2): 275.
- Saxena A (2005) Congenital heart disease in India: A status report. Indian Journal of Pediatrics 72(7): 595-598.
- Sharmin LS, Haque MA, Bari MI, Ali MA (2008) Pattern and Clinical Profile of Congenital Heart Disease in A Teaching Hospital. TAJ: Journal of Teachers Association 21(2): 58-62.
- Deo B, Jadhav J, Idgampalli N, Deo N, Sabale R, et al. (2015) Study of clinical profile of Congenital Heart Disease in paediatric age group. Indian Journal of Basic and Applied Medical Research 4(4): 269-272.
- ADC (2004) Congenital heart disease and maternal diabetes. Archives of Disease in Childhood 89(3): 211.
- Chambers TL (2004) Forfar & Arneil’s Textbook of Pediatrics: 6th edition. Journal of the Royal Society of Medicine 97(2): 96.
- Abu-Sulaiman R M, Subaih B (2004) Congenital Heart Disease in Infants of Diabetic Mothers: Echocardiographic Study. Pediatric Cardiology 25(2): 137-140.
- Arul AS, Babu Kandha Kumar AS, Kiruthiga K, Priya MK, Neveythaa SA, et al. (2019) Spectrum of Cardiovascular Abnormalities in Infants Born to Diabetic Mother in a Tertiary Care Center. Indian Journal of Cardiovascular Disease in Women WINCARS 04(03): 124-128.
- Begum S (2013) Congenital Heart Disease - Bangladesh Perspective. Bangladesh Journal of Anatomy, 10(2): 43- 44.
- Bloomfield P, Bradbury A, Grubb N, Newby D (2006) Cardiovascular Disease. In N. Boon, N. Colledge, & B. Walker (Eds.) Davidson’s Principle and Practice of Medicine (20th ed, pp.519-646). Edinburgh: Churchill Livingstone.
- Hoque M, Hussain MM, Ahmad AR, Uddin MS (2014) Pattern of Congenital Heart Disease in Children Admitted into Tertiary Care Hospitals of Sylhet: A Multicenter Study. Bangladesh Journal of Child Health, 38(1): 15-18.
- Leirgul E, Brodwall K, Greve G, Vollset SE, Holmstrøm H, et al. (2016) Maternal Diabetes, Birth Weight, and Neonatal Risk of Congenital Heart Defects in Norway 128(5): 1116-1125.
- Mita SA, Salim M, Haque MA, Shahriar A, Zakia MNU, et al. (2017) Comorbidities with Congenital Heart Disease among Hospitalized Children in a Specialized Cardiac Hospital in Bangladesh. Cardiovascular Journal 9(2): 83-89.
- Rowland TW, Hubbell JP, Nadas AS (1973) Congenital heart disease in infants of diabetic mothers. The Journal of Pediatrics 83(5): 815-820.
- Sen SS, Barua T, Dey D, Chowdhury MA, Nessa L, et al. (2018) Pattern of Congenital Heart Disease in Children Presenting at Paediatric Cardiology Unit in Chattagram Maa Shishu-O-General Hospital, Chittagong. Chattagram Maa-O-Shishu Hospital Medical College Journal 16(2): 40-43.
- Simeone RM, Devine OJ, Marcinkevage JA, Gilboa SM, Razzaghi H, et al. (2015) Diabetes and Congenital Heart Defects. American Journal of Preventive Medicine 48(2): 195-204.
- Wren C, Birrell G, Hawthorne G (2003) Cardiovascular malformations in infants of diabetic mothers. Heart 89(10): 1217-1220.

 Research Article
Research Article