Abstract
Background: Morbidity and mortality for trauma accidents in rural settings is nearly three to six times as high as in urban settings in the United States. In both developed and developing countries, most morbidity due to trauma occurs in the prehospital period. This increase in morbidity and mortality is in part, due to a lack of appropriate critical care education of first responders in rural settings. We sought to address this issue by increasing the number of trained first responders as well as to assess the confidence and competency of participants’ trauma management skills. The Vyas Global Prehospital Education Initiative (VGPEI) aims to address this problem through implementation of a four-tiered trauma education program, which incorporates high-fidelity simulation, video-recorded debriefing, and retraining. These four tiers include a Massive Open Online Course (MOOC) Trauma Training, Acute Trauma Training (ATT), Broad Trauma Training (BTT) (in-depth ATT curriculum especially designed for trainers of ATT), and Cardiac and Trauma Training (CTT). Previous studies show that this approach can be an effective strategy for teaching prehospital trauma management skills. Additionally, this innovative educational program has been shown to be efficacious in improving first responder confidence in management of trauma. This study focuses on the implementation of ATT in a rural setting in West Texas, geared at educating and empowering community stakeholders (medical students with interest in pursuing rural family medicine track, established volunteer fireman, police) with trauma training. The BTT trainers will enable exponential growth of establishing chains of training centers. Basic trauma management skills were targeted at community members to evaluate proof of concept of this program being used to address critical care needs in the pre-hospital period. The purpose of this study is to evaluate the efficacy of BTT in improving competence and competence in community stakeholders with varying levels of educational attainment and medical training. This educational session was intended to test proof of concept that this type of training could be more broadly applied to populations across West Texas.
Objective: To assess the efficacy of a trauma care training program in West Texas.
Method: The First Responder Trauma and Emergency Care Program uses an interactive model of lectures, followed by breakout sessions where program participants practice the skills discussed in simulation environments. Simulation has previously been shown to be a useful tool in the training of trauma-related clinical skills. This session was intended to test proof of concept of this type training being useful in West Texas where sparse population and isolated location make trauma care uniquely challenging and similar in many ways to trauma care in the developing world. This study aims to assess whether the program is effective in improving specific skills related to trauma care.
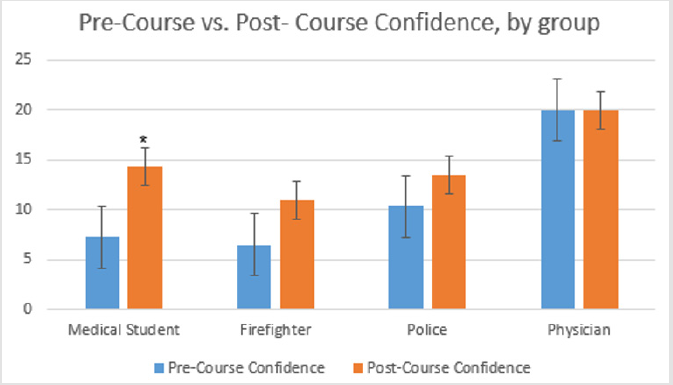
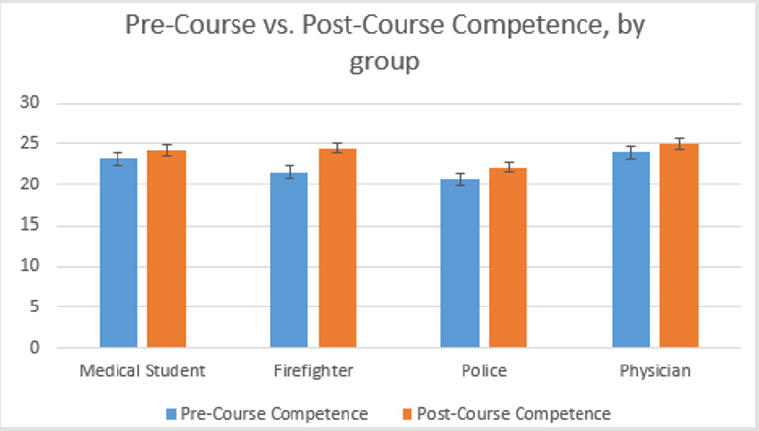
Results: The change in confidence of medical students was significant; t(8)=0.005, p=0.013. While no other groups showed significant changes in competence or confidence, there was demonstrated improvement in all groups.
Conclusion: The initial assessments point towards the First Responder Trauma and Emergency Care Program being a worthwhile effort in the West Texas region. This pilot study also shows that despite a small sample size showed an upward trend in confidence and competence attainment and are likely effective in improving confidence and competence of first responders, but further studies are needed to assess whether this program produces a significant difference in these areas. Future efforts will include recreation of this session in the cities of Lubbock and Amarillo, further analysis of data points collected from these additional sessions, and determination of what additional locations would benefit from these sessions in addition to analysis of the efficacy of the program in improving trauma care.
Abbreviations: MOOC: Massive Open Online Course; ATT: Trauma Training; Acute Trauma Training; BTT: Broad Trauma Training; CTT: Cardiac and Trauma Training
Introduction
General Background
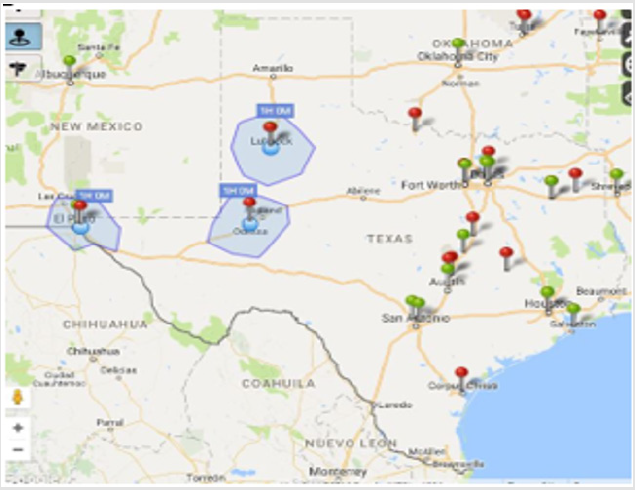
Trauma is a leading cause of death worldwide and is particularly prevalent and troubling in the United States. The “Golden Hour” in trauma has long been cited as the critical goal to reduce morbidity and mortality. However, there is increasing evidence to suggest not only that this benchmark may not be as ideal as previously thought, but also that many Americans face significant geographical barriers in receiving trauma care in this timeframe [1-6]. This disparity in care can be viewed in Figure 1, showing the vast areas of West Texas that are not within a 1 hour driving distance to a Trauma Center [5]. With increasing evidence suggesting that with appropriate training, civilians can safely administer basic prehospital care, there is clear need for effective training of large portions of the population as a strategy to improve prehospital trauma care, and ultimately, traumarelated morbidity and mortality [5]. Prehospital trauma care first became an area of major focus for the medical community during the Vietnam War, after noting marked improvements in battlefield injury outcomes related to improved hemostatic intervention and transport systems [6,7]. Improved structure of trauma systems has been noted to both decrease time to definitive care as well as trauma outcomes [6]. However, especially in sparsely populated and remote areas, the need for on-site intervention by bystanders is an area that could greatly improve trauma outcomes by stabilizing the patient, and potentially extending the traditional golden hour [1].
Therefore, a prehospital trauma care training program has the potential to spread these skills to a much broader cohort than the traditional medical community and to provide greater trauma care coverage to all citizens, especially those in underserved areas. Many models of prehospital care promote the use of first responders [8]. Two complimentary approaches, designated Tier 1 and Tier 2 care, have been suggested by the WHO in their publication, “Prehospital Trauma Care Systems”. Tier 1 denotes individuals without formal Training, such as bystanders. Tier 2 indicates the use of formally medically trained personnel. This study specifically addresses the prehospital period denoted by Tier 1.
Relationship of Confidence to Bystander Effect
Some estimates place the portion of the world’s population living in areas without access to formal EMS at 50-75%. This means that the use of Tier 1 individuals could have broad effects on prehospital morbidity and mortality outcomes [8]. The creation groups of Tier 1 responders via training resources in basic first aid and trauma care techniques via mobilization of community members could be one way of accomplishing this. Previous studies have shown that many (83%) of bystanders are willing to perform lifesaving skills (i.e. CPR) in emergency situations such as Cardiac Arrest [9]. Of the respondents not willing to perform these skills, they cited lack of confidence as a barrier [9]. By simply strengthening the confidence of bystanders via education and training, a direct increase in willingness to provide emergency care has been previously shown [1].
Pedagogical Efficacy in Relation to Traditional Training Programs
In a previous literature review, several themes were found to be common amongst trauma education initiatives directed towards layperson first responders [2] These included assessing existing resources, adapting existing resources to optimally educate laypersons, tailoring training methods to low or variable education and literacy levels, and a post-training method of assessment. Of note was that the optimization of technology for remote use was found to be particularly valuable in low resource settings. The Million Life Fighters Campaign implemented via the Vyas Global Prehospital Education Initiative (VGPEI) proposes and implements a novel four-tiered trauma training protocol that can address the gaps in existing trauma training protocols. These existing protocols become particularly problematic in low-resource settings [9]. VGPEI takes an innovative approach to trauma skill education by implementing a program that accommodates educational and socioeconomic diversity, which prioritizes utilizing layperson language, accessibility, cost-effectiveness and high-fidelity simulation training [3]. This program was initially implemented in a large police training center in Jodhpur, India and showed promising efficacy in improving competence and confidence.
General Goals and Future Direction
Limited evidence exists regarding prehospital training and outcomes, but in limited data among medical personnel, simulation training improves confidence in performing prehospital care [4]. In more directed study, a precursor curriculum to the one studied showed statistically significant improvement competence increases in all areas of trauma management tested [10]. The need for prehospital training, lack of sufficient coverage by trauma centers and medical personnel, and evidence to suggest that training is a serviceable way to transfer prehospital care skills necessitate that the medical community make use of the opportunity to spread prehospital care skills to as many people as possible.
Traditional trauma training programs such as Advanced Trauma Life Support (ATLS), International Trauma Life Support (ITLS), and Basic Life Support (BLS) have proven ineffective as conduits to transfer trauma skills to civilians [1]. In our training paradigm, we have introduced a four-tiered program that consists of Acute Trauma Training (ATT), Broad Trauma Training (BTT), Cardiac Trauma Training (CTT), and Massive Open Online Course (MOOC) Trauma Training [3]. Traditional trauma training paradigms are designed to complement medical education, and therefore are ill-suited for use as curriculum structures for the general public [3]. Previous studies have shown the efficiency and efficacy of lay trauma training and provide foundational evidence to support implementing a lay trauma training program in the United States, especially in remote areas [11].
We have taken our curriculum with previously shown success in rural India and implemented it in a one-day workshop with a varied group of students with myriad levels of medical knowledge and educational attainment. We hypothesized that the participants would attain or improve upon identified trauma ca-re skills in the given time, as measured by a written pre and posttest. It is our hope that by maximizing the efficacy of this program and widely distributing it amongst community stakeholders from a diverse set of backgrounds in West Texas, we can greatly impact the distribution of trauma first responders in this vast geographical area, and ultimately impact morbidity and mortality in trauma [12- 14].
Materials and Methods
This prehospital training program has evolved over multiple trials to maximize clinical relevance and educational efficacy. The previous version of this course, which this pilot study’s curriculum was based off of, was a ten-skill curriculum delivered in a one-day course in order to best replicate current trauma training curricula. This course was one day long and heavily emphasized skills most critically important to prehospital trauma care. This course was instructed by making broad use of presentations laden with images, complemented by a text manual that was comprehensive in nature, interactive sessions for skill practice and refinement, and debriefing in order to best support long term retention. Practical skills training incorporated a standard mannequin and basic first aid and trauma care tools.
Setting
The training program was conducted in the Texas Tech University Health Sciences Center simulation center at Medical Center Hospital in Odessa, Texas. The program was conducted over a full day in April 2016. This program was conducted as a pilot study to investigate the feasibility and efficacy of our international curriculum in a domestic but rural setting. We collaborated with community and institutional partners in hopes of conducting future training sessions in additional locations.
Participants
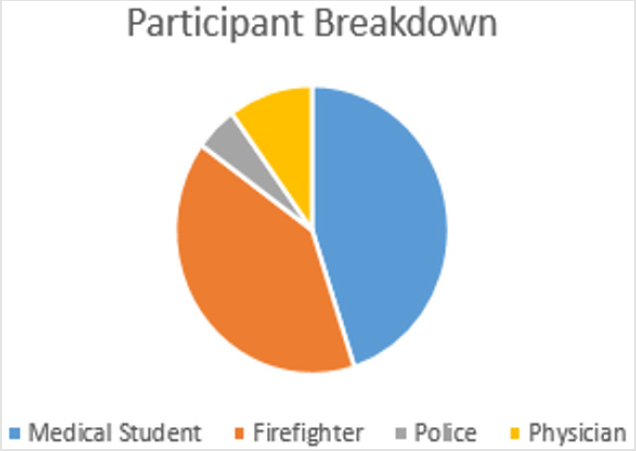
The individuals most likely to first interact with victims of trauma in West Texas include the police, firefighters, nurses, emergency medical technicians, and hospital staff. Participants from these fields were recruited with assistance from established stakeholders, which included a medical school dean and senior officials from local fire and police departments. Instructors were recruited from TTUHSC faculty and hospital staff [14-18]. The physicians trained were primarily comprised of family medicine residents-as they serve a major role as the first line in health care-and trauma care-in this region. Additionally, these residents and medical students were intended to serve as trainers to first responders and lay people in future events. A breakdown of the participants in this course can be seen in Figure 2.
Figure 2: Breakdown of Participants in pilot course showing that the overwhelming majority of participants were medical students and volunteer firefighters, but that participants from a wide variety of backgrounds took part in the course.
Training Curriculum
Our program attempts to make a maximal educational impact in a minimally short course duration by creating a fully immersive experience. The curriculum included a set of ten essential trauma topics: airway management, hemorrhage control, fracture stabilization, cervical spine immobilization, chest injury management, intravenous access, extrication and helmet removal, scene management, triage, and communication. Didactic instruction consisted of live lectures delivered by Dr. Vyas. After the lectures, a short question and answer period ensued, with questions being answered by Dr. Vyas. This was followed by 30-40 minutes of practical skills simulation training, which culminated with a period of 15-20 minutes for video-recorded debriefing. ATT practical session groups consisted of up to 5 participants per instructor, who provided real-time feedback on proper skills techniques for many who practiced on a standard mannequin.
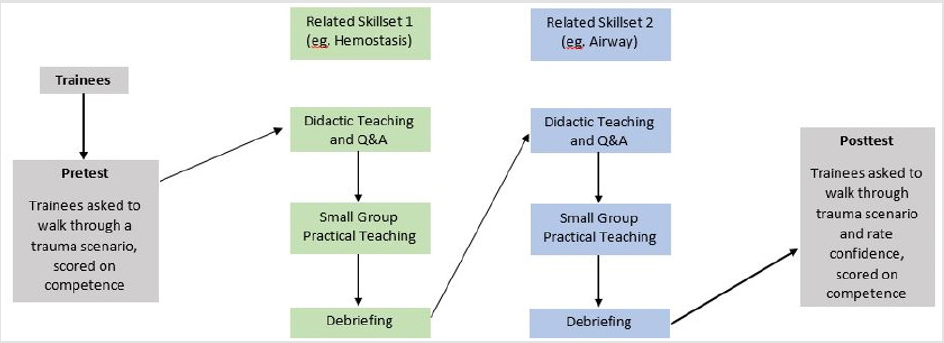
Practical session groups were restricted to up to five trainees per instructor, in order to maximize the amount of time each participant practiced the skills and degree of feedback given. Specific skills introduced included pulse identification, cardiopulmonary resuscitation, intravenous catheter placement, airway insertion, tourniquet application, fracture splinting, helmet removal, cervical collar placement, log-roll movement onto a backboard, and hypothetical triage and communication exercises. Emphasis was placed on practical solutions in low-resource settings by creating medical devices with objects that are more generally available, such as wooden slabs, bed sheets, towels, sticks, and pens. However, trainees also were trained to use advanced instruments like pulse oximeters and the disposable King LT Airway. All trainees were provided with low-cost trauma kits at the conclusion of the training program, including the King LT Airway, pulse oximeters, scissors, bandages, surgical tape, latex gloves, and simple tourniquet supplies. A flowchart of the curriculum flow can be seen in Figure 3.
Study Design
Our study aims to identify increases in confidence and competence of participants after completing our training curriculum. Improvement in confidence was measured using de-identified pre-training and post-training surveys wherein participants evaluated their confidence in performing the skills in each of the course’s core topics. Each topic was rated by the trainee on a three-point Likert scale: 0=Not at all confident (do not understand, cannot perform skills); 1=Moderately confident (have some doubts in understanding, but can attempt skills if necessary); 2=Very confident (completely understand, can perform skills readily and independently). Competence was measured by a 29-item questionnaire, which covered various topics covered both in didactic sessions and verbal questions about skills learned. Statistical analysis was performed under a general linear model using Microsoft Excel 2010. Homoscedastic t-tests with twosample equal variance were used to analyze differences in mean confidence between the pre- and post-training survey data, which were virtually identical in response rates.
Results
In the pre-course confidence assessment, Medical Students and Firefighters showed the lowest level of confidence in their trauma care skills, at 7.22/20 and 6.50/20. Physicians showed the highest level of pre and post course confidence and competence and had the smallest change in competence. The change in confidence of medical students was significant; t(8)=0.005, p=0.013. There was demonstrated improvement in confidence and competence in all groups, as shown in Figures 3 & 4, respectively, which may have been statistically significant with a larger sample size.
Figure 3: The flow of the day-long curriculum of the ATT Program showing the cyclical manner in which participants are introduced to skills and concepts via didactic teaching, and then the lessons are driven home through simulation and mock drills both to show attained competence and information retention but also to improve confidence in performing skills in future scenarios.
Figure 4: Pre-Course versus Post-Course Confidence showing a significant increase in medical student confidence and a general positive trend in all groups’ confidence attainment.
Discussion
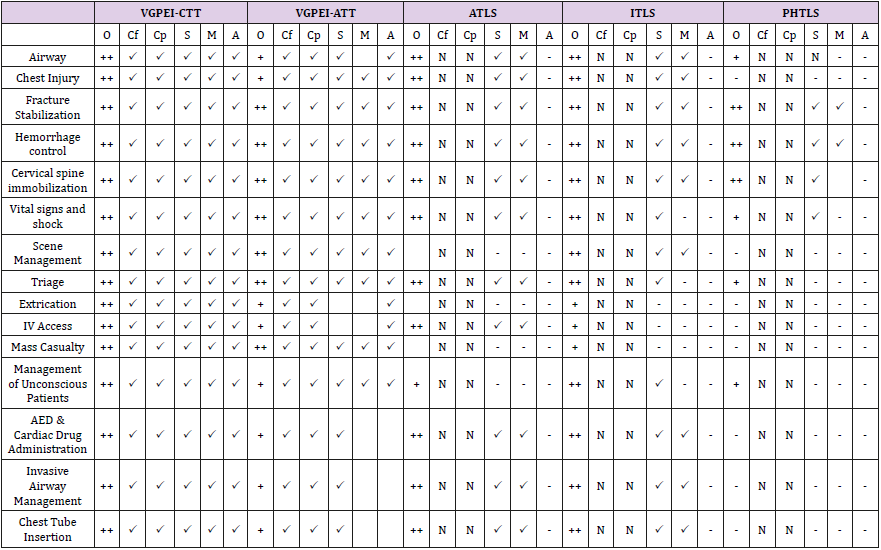
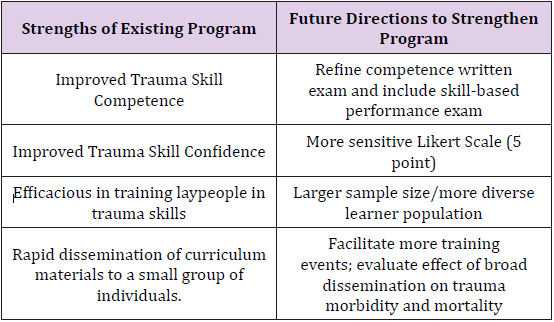
Our study demonstrated improvement in participant confidence and competence with a variety of trauma care-related topics. This improvement demonstrates the capacity for our curriculum to enhance trainees’ perception of their skills and potentially make them more likely to utilize such skills toward the improved care of trauma victims. Further study will be required to investigate the efficacy of this training program in a variety of populations and geographic areas. Despite a great deal of growth in recent years due to a booming oil market, West Texas is still largely rural and is a profoundly medically underserved region encompassing a vast geographic area [HRSA]. However, the region notably lacks the development of a centralized, robust pre-hospital care system, leading to unnecessary trauma-related mortality throughout the region. This paper examines the efficacy of a novel trauma care training program in transferring trauma care skills to laypersons. Through repeated study, we have identified weaknesses in the program that can be improved with continuing program evaluation and restructuring. A notable weakness in the ATT curriculum is the limited scope of topics taught relative to US-based trauma care curriculums (ATLS, BLS, etc) (Table 1) & (Figure 5). Topics in this curriculum were chosen based on feasibility of skill attainment and retention as well as potential clinical yield. Future program development will broaden skills taught at various tiers, as well as offering lower-tier training more frequently and in more locations. Another structural weakness of this program is its’ utilization of a 3-point Likert scale to represent confidence, as opposed to a 5- or 7-point Likert scale to allow for better discrimination between differences in confidence.
Table 1: Comparison of coverage and teaching efficacy of multiple skills between VGPEI, ATLS, ITLS and PHTLS. This chart shows that VGPEI is superior is having been studied and shown proven confidence improvement in multiple skill areas, as well as providing participants with a mock drill to practice their skills. O denotes the overall coverage of the subject material, Cf indicates confidence improvement, Cp indicates competence improvement, S denotes simulation teaching, M indicates a Mock Drill is performed with that skill and A denotes the use of animation-assisted education. NDA denotes that the topic either is not covered in the course or has not been studied. + Denotes the topic is mentioned and completion of the course indicates understanding of the concept. ++ denotes extensive coverage and mastery of the concept or skill. – indicates that the topic is not covered in the course. Indicates usage of a teaching modality or proven efficacy.
Previous studies have described the process of developing various layperson first responder training programs and have shown their ultimately positive effect on trauma outcomes. These programs vary in length, trainee backgrounds represented, baseline experience and education, and geographic location. This study lays the groundwork for future broad study to evaluate and implement lay trauma training in the United States. There are specific limitations to this study which prevent it from giving the definitive evidence program efficacy. First, we utilized a 3-point Likert scale-mostly for course-participant simplicity as our participants’ educational attainment ranged from less than high school to postgraduate medical training. In addition, the data was not analyzed in a paired manner, which would have provided greater clarity in elucidating the relationship between confidence and competence improvement pre and post-course. A representation of current strengths of the program and planned future study and solutions to weaknesses in the study and program design are presented in Table 2.
Figure 5: Comparing Pre-and Post-Course Competence by group showing a generally positive trend as well as a high baseline competence.
Table 2: Examining current program strengths and outlining future directions of study and alteration in program design to strengthen both study and program design.
Conclusion
Given the morbidity and mortality burden of trauma in the United States, and the particular failure of the current medical system to adequately care for trauma victims in rural areas, there is great need for bystander trauma training. This preliminary study shows proof-of-concept for our curriculum to be used to teach trauma care skills to community stakeholders (Police, Firefighters, EMT’s), as well as lay persons to create a broader network of individuals capable of providing aid to trauma victims until definitive care can be reached. There is a considerable and growing body of evidence to suggest the importance of even minimal interventions such as tourniquets, CPR, fracture stabilization, etc.
Acknowledgement
Disclosure
Dinesh Vyas, Arogyaa Vyas Healthcare Pvt Ltd, Mission Million Life Fighter and VGPEI supported the growth of the study material and implementation of various programs. Natalie, Mayank and Manisha reported no proprietary or commercial interest in any product mentioned or concept discussed in the article.
Funding
VGPEI sponsored this study.
Author Contributions
Natalie Tully, Manisha Bhatia, Mayank Aranke, and Dinesh Vyas were involved with the conception and development of the study. Natalie Tully, Mayank Aranke and Dinesh Vyas were involved with data collection; Natalie Tully was involved with data analysis and interpretation. Natalie Tully and Dinesh Vyas were involved with writing the article. Natalie Tully and Dinesh Vyas were involved with the approval of the final version.
References
- Mock C (2009) Strengthening Prehospital Care in the Absence of Traditional Emergency Medical Services. World J Surgery 33(12): 2510-2511.
- Callese TE, Richards CT, Shaw P, Schuetz SJ, Issa N, et al. (2014) Layperson trauma training in low-and middle-income countries: a review. J Surg Res 190(1): 104-110.
- Abraham R, Vyas D, Narayan M, Vyas A (2015) Strategically Leapfrogging Education in Prehospital Trauma Management: Four-Tiered Training Protocols. Amer J Robot Surg American Journal of Robotic Surgery 2(1): 9-15.
- Dillen CMV, Tice MR, Patel AD, David A Meurer, Joseph A Tyndall, et al. (2016) Trauma Simulation Training Increases Confidence Levels in Prehospital Personnel Performing Life-Saving Interventions in Trauma Patients. Emergency Medicine International p. 1-5.
- (2016) Find Shortage Areas. Find Shortage Areas. Accessed.
- Alarhayem A, Myers J, Dent D, Liao L, Muir M, et al. (2016) Time is the enemy: Mortality in trauma patients with hemorrhage from torso injury occurs long before the “golden hour.” The American Journal of Surgery 212(6):1101-1105.
- Passos E, Dingley B, Smith A, Engels PT, Ball CG, et al. (2014) Tourniquet use for peripheral vascular injuries in the civilian setting. Injury 45(3): 573-577.
- Kanstad BK, Nilsen SA, Fredriksen K (2011) CPR knowledge and attitude to performing bystander CPR among secondary school students in Norway. Resuscitation 82(8): 1053-1059.
- Cheskes L, Morrison LJ, Beaton D, Parsons J, Dainty KN (2016) Are Canadians more willing to provide chest-compression-only cardiopulmonary resuscitation (CPR) -a nation-wide public survey. CJEM 18(4): 253-263.
- Aekka A, Abraham R, Vyas D, Hollis M, Boudiab E, et al. (2015) Prehospital trauma care education for first responders in India. Journal of Surgical Research 197(2): 331-338.
- (2016) Find Your Local Trauma Center - American Trauma Society.
- Esposito TJ, Maier RV, Rivara FP, Pilcher S, Griffith J, et al. (1995) The impact of variation in trauma care times: urban versus rural. Prehosp Disaster Med 10(3): 161-166.
- Jayaraman S, Mabweijano JR, Lipnick MS, Nolan Caldwell, Justin Miyamoto, et al. (2009) First Things First: Effectiveness and Scalability of a Basic Prehospital Trauma Care Program for Lay First-Responders in Kampala, Uganda. PLos one 4(9).
- Ritter M, Bowyer MW (2005) Simulation for trauma and combat casualty care. Minim Invasive Ther Allied Technol 14(4): 224-234.
- Scerbo MH, Mumm JP, Gates K, Love JD, Wade CE, et al. (2016) Safety and Appropriateness of Tourniquets in 105 Civilians. Prehospital Emergency Care 20(6): 712-722.
- Varghese M (2005) World Health Organization. Prehospital trauma care systems.
- Vyas D, Hollis M, Abraham R, Rustagi N, Chandra S, et al. (2016) Prehospital care training in a rapidly developing economy: a multi-institutional study. J Surg Res 203(1): 22-27.
- (2014) World Health Organization. Injuries and violence: the facts.

 Research Article
Research Article