Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Maha Oudrhiri*1, Chaima Rherib1, Mouna Oulja1, Abdellah Assermouh1, Chafik Mahraoui1 and Naima EL Hafidi1,2
Received: January 22, 2019; Published: February 12, 2019
*Corresponding author: Maha Oudrhiri, Pediatrics Department, Pediatric Infectious Diseases Division, Rabat children’s, S12A11 Hay Riad Rabat Morocco
DOI: 10.26717/BJSTR.2019.14.002553
A benign oropharyngeal infection without appropriate treatment can be complicated by a jugular vein thrombosis. This septic clinical picture most commonly known as Lemierre syndrome. Though this complication appears to be rare, early diagnosis and prompt intervention have proven critical in survival outcome. We describe two pediatric cases who has presented this syndrome. Adequate antibiotic treatment for 6 weeks associated with anticoagulant treatment have allowed a complete recovery without sequel.
Keywords: Lemierre’s Syndrome; Septic Thrombophlebitis; Bacterial Infections; Child
Lemierre’s syndrome is a rare complication following an acute oropharyngeal infection. The syndrome is characterised by a primary oropharyngeal infection followed by metastatic spread and suppurative thrombophlebitis of the internal jugular vein. This syndrome is an uncommon but potentially lethal complication of otolaryngological infections. Pediatricians and Emergency physicians should be aware of this syndrome because its incidence appears to be increasing. In an effort to emphasize the importance of early diagnosis and treatment of this once “forgotten disease,” we present 2 pediatric patients with Lemierre syndrome.
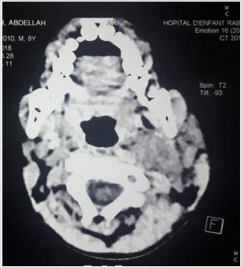
An 8-year-old previously healthy boy presented to our pediatric emergency room complaining of fever and cervical pain for 3 day. His fever was continuous, reaching a maximum of 39°C, and was associated with limitation of movement of his neck. He had no seizures, no altered level of consciousness, and no lethargy. These symptoms were preceded by a five-day prodrome of nasal congestion, minimal cough, and sore throat. On admission, there was swelling of the left neck and restriction in range of movement with mild trismus (Figure 1), although there was no photophobia, and on examination he had a negative Kernig’s and Brudzinski sign. Her temperature was 39.9°C, respiratory rate was 18 breaths/ min, blood pressure was 105/44 mmHg, and heart rate was 147 bpm. The remainder of the examination was within normal limits. Doppler ultrasound of the neck showing a large echogenic thrombus in the left internal jugular vein (Figure 2). A computed tomography (CT) of the neck showed a thrombus in the left internal jugular vein (IJV) extending to cavernous sinus (Figure 3) with 2 abscess formation measuring 20*14 mm and 15*11 mm associate to ipsilateral lymphadenopathy.
Figure 2: Doppler ultrasound of the neck showing a large echogenic thrombus in the left internal jugular vein.

Figure 3: Doppler ultrasound of the neck showing a large echogenic thrombus in the left internal jugular vein.
Initial laboratory investigations showed leucocytosis (white cell count 13.7 × 109/L) and an elevated C-reactive protein (CRP). His blood culture was positive for group A Streptococcus within 48 hours. The patient was started antibiotic therapy intravenous: ceftriaxone and metronidazole. In view of the extensive venous thrombosis involving left internal jugular veins with extension to the cavernous sinus, he was started on anticoagulation. He was treated with subcutaneous low molecular weight heparin for 6 weeks. The patient had a rapid response to therapy. he had recovered completely after discharge and his Doppler ultrasonography was normal.
A 13 months old boy with no significant medical history was admitted with a 1-week history of fevers, after an episode of pharyngitis. Her illness initially started with fever, odynophagia, and swelling in the neck. His parents administered him without a medical prescription of cefixime then amoxicillin clavulanic acid. On examination, the child was febrile but hemodynamically stable. There was a large left neck mass, 2 × 3 cm in size which was warm and tender with overlying erythema with torticollis. There was no palpable lymphadenopathy and the tonsils were not enlarged or deviated. He was well looking, well hydrated, and had negative meningeal signs. Examinations of the other systems were unremarkable. A computed tomography (CT) scan of the patient’s neck demonstrated thrombosis of the left internal jugular vein with abscess parapharyngeal without bone lysis (Figure 4). Initial laboratory tests revealed a white cell count of 23.5 × 109/L (neutrophils 17.9 × 109/L), red blood cell count of 5 × 1012/L, platelet count of 584 × 109/L, C-reactive protein levels of 123 mg/L, and hypochromic microcytic anemia with hemoglobin levels of 10.1 g/dL.
The child was initially started on ceftriaxone upon admission. However, the above findings increased the suspicion of Lemierre’s syndrome, and therefore metronidazole and enoxaparin were added. Multiple repeated blood cultures (including specific anaerobic ones) were obtained during the admission, all of which were negative. The patient clinically improved while on treatment, did not require surgical drainage and was ultimately discharged with a total of 6 weeks of antibiotics and anticoagulation.
Described by Lemierre in 1936, septic phlebitis of the internal jugular vein secondary to oropharyngeal infection, or Lemierre’s syndrome, is extremely rare [1]. In the post antibiotic era, it was named the “forgotten disease” until recently, when it started presenting more frequently and uniquely. This apparent increase in the incidence may be due to antibiotic resistance or changes in antibiotic prescription patterns and overconsumption nonsteroidal anti-inflammatory drugs during ENT infections, and decreased tonsillectomy since the 1970s [2,3]. A constellation of clinical history, examination, microbial isolate, and radiologic findings of thrombosis is used to label the patient with LS. It is characterized by
a) a history of recent oropharyngeal infection,
b) clinical or radiological evidence of internal jugular vein thrombosis (IJVT), and
c) isolation of a pathogen [4].
The aetiological agent is typically anaerobic bacteria of the genus Fusobacterium. A comprehensive review of the literature on bacterial ecology involved in this syndrome found several species of Fusobacterium (funduliform, specians, nucleatum), Streptococcus (group A, B, C, oralis, constellatus, intermedium), Staphylococcus (methicillin-sensitive / resistant aureus, epidermidis) [5,6], of Enterococcus, Proteus mirabillis, Klebsiella pneumoniae, of Pseudomonas aeruginos (5). Many cases with negative cultures was reported (4,6).
The possible causes of this diagnostic outcome, including length of time needed for cultures to grow and suppression of growth because of prior antibiotic use, which would include our patient (case 2) [7]. As there is no set standard diagnostic criterion for Lemierre’s syndrome, we strongly recommend that providers rely on their clinical judgment especially considering the rarity of this condition and possible variants. An enhanced computed tomographic scan of the neck is the technique of choice to demonstrate the thrombosis of the internal jugular vein [8]. LS is rare but very devastating disease and is on the rise. Pediatricians should be very vigilant in recognizing and managing it. The mechanism of clot formation, especially in the internal jugular veins, is secondary to an inflammatory and septic process. Patients are not generally at increased risk for coagulopathy. LS complications are responsible for morbidity and mortality important in the absence of rapid introduction of anti-infective treatment [9]. Indeed, the risk of dissemination septic is directly correlated with the time to treatment [10].
Like all infections, the optimal antibiotic regimen depends on the source of infection. Initial management should include coverage with broad-spectrum antibiotics. Acceptable antibiotic regimens include high-dose ceftriaxone along with metronidazole or clindamycin monotherapy (11). Vancomycin can be added if suspicion or prevalence of methicillin-resistant Staphylococcus aureus is high. Minimal therapy seems to include at least 2 to 4 weeks of IV antibiotics followed by another 2 to 4 weeks of oral therapy. Currently, there is no consensus opinion on the use of anticoagulation in patients with Lemierre syndrome complicated by septic internal jugular thrombosis and embolism [11]. Case series have reported 21%-30% of patients are treated with anticoagulation. A few authors have advocated for the use of anticoagulants in all cases of Lemierre’s syndrome. Others have recommended anticoagulation only if thrombosis extends into the cerebral sinuses or if there has been no improvement in symptoms with antibiotic therapy alone [12]. Surgical involvement is usually a last step in the process. Surgery may be indicated for complications of Lemierre syndrome, such as loculated empyemas, brain abscesses, pulmonary abscesses, retropharyngeal abscesses, or other adverse sequelae (13). Successful management rests on the awareness of the condition, a high index of suspicion, and a multidisciplinary team approach [13].
Lemierre’s syndrome is rare but needs to be identified early in the course. He must be evoked in front of any oropharyngeal infection accompanied by lateral neck pain. Treatment is not consensual but large antibiotic therapy associated with anticoagulation seems effective.


