Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Ram B Singh1, Viliam Mojto*2, Jan Fedacko3, Galal Elkilany4, Krasimira Hristova5, Agnieszka Wilczynska6 and Dr Kumar Kartikey7
Received: January 12, 2019; Published: January 24, 2019
*Corresponding author: Viliam Mojto, 3rd Internal Clinic, Faculty of Medicine, Comenius University, Bratislava, Slovakia
DOI: 10.26717/BJSTR.2019.13.002421
There is an endorsement from American Heart Association that depression should be considered a risk factor of heart disease and recommends its screening as part of routine practice. However, all experts do not agree due to controversy on account of inconsistencies in the evidence linking treatment of depression to improved outcomes in Cardiovascular Diseases (CVDs). Further evidence indicates that chrono-behavioral and chrono-physiological dysfunctions can predispose traditional risk factors of CVDs as well as other psychological disorders including depression. Recently, reduced duration of sleep which is a risk factor of depression has also been reported to be risk factors of CVDs. Chronic mood disorders such as depression are also known to predispose acute Myocardial Infarction (MI). The incidence of depression may be three-fold higher among Acute Coronary Syndrome (ACS) patients compared to the control subjects. Therefore, there is a need to treat depression to prevent CVDs. Depression can increase amygdalar activity in the brain, which could be examined as tremors in the amygdala by Functional Magnetic Resonance Imaging (fMRI). The activation of amygdala may be associated with increased bone marrow activity and inflammation with increased hsCRP. Western diet is a possible risk factor of depression as well as myocardial infarction, and both are associated with oxidative stress and inflammation. Hence Mediterranean styles diets that are anti-inflammatory, may be used for the preventions of both the diseases. Recent clinical trials in subjects with depression after recent myocardial infarction revealed that antidepressant therapy with escitalopram can cause a lower risk of major cardiovascular events. Further studies are needed to establish the role of antidepressants, along with Mediterranean style diets, in the management of depression in patients with ACS.
Keywords: Anxiety Disorders; Heart Attack; Sleep Disorders; Mood Disorders; Inflammation
Abbreviations: CVDs: Cardiovascular Diseases; MI: Myocardial Infarction; ACS: Acute Coronary Syndrome; fMRI: Functional Magnetic Resonance Imaging; AHA: American Heart Association; MACE: Major Adverse Cardiovascular Events; CAD: Coronary Artery Disease; RRs: Relative Risks; SSRI: Selective Serotonin Reuptake Inhibitors, CHF: Chronic Heart Failure
Apart from the traditional risk factors, non-traditional risk factors; late-night sleep, late-night eating, heavy meals, psychosocial stress, and sleep deprivation are called chrono-behavioral risk factors of Acute Coronary Syndrome (ACS) or Myocardial Infarction (MI) [1-3]. These chrono-behavioral and chronophysiological dysfunctions can predispose the traditional risk factors of Cardiovascular Diseases (CVDs), as well as chronic anxiety disorders such as depression leading to MI [4-10]. Recently, duration of sleep which is a risk factor of depression has also been reported to be risk fac tors of CVDs [11]. Chronic mood disorders such as depression have become important risk factors of ACS, which can explain much of the hidden risk that increases the vulnerability of MI patients to increased cardiovascular events [8-11]. Despite increases in the use of modern drug therapy and interventions, the residual risk of death, MI, or stroke up to 1 year after acute MI remains high. There is a need to control this risk by preventing adverse effects of elevated glucose, inflammation, oxidative stress and chronic mood disorders, such as depression by nutritional modification and drug therapy, because increased risk of recurrent cardiovascular events, among these patients, appears to be related to mood disorders such as depression.
.Recently, American Heart Association (AHA) has advised that depression should be considered as a risk factor CVDs and therefore screening for this entity should be as part of clinical practice [5]. However, it has been met with controversy because of inconsistencies in the data that have been used to link treatment of depression leading to improved outcomes in CVDs. This narrative and selective review aims to emphasize that treatment of depression by drug therapy and nutritional intervention may be beneficial in patients with CVDs.
AHA conducted a systematic review of literature to assess the association of depression with adverse medical outcomes among patients with recent ACS [5]. The outcomes were nonfatal cardiovascular events, cardiac mortality, all-cause mortality, and composite outcomes for mortality and CVDs. The strength, independence, consistency, and generalizability of the published studies in this review, were duly considered. Of total 53 studies, 12 reported on association with cardiac mortality, 32 with all-cause mortality and 22 with composite outcomes but only 4 meta-analyses met inclusion criteria. Although due to limitations in heterogeneity in some studies, this review showed consistent associations between depression and adverse outcomes due to CVDs. The preponderance of evidence supports the recommendation that the AHA should consider depression as a risk factor for CVDs, in patients with ACS [5].
A more recent study prospectively examined the association between known depression and Major Adverse Cardiovascular Events (MACE) in patients referred for exercise stress tests [4]. This study included 2385 consecutive patients with history of CVD and antidepressant use. After a follow up of 8.8-years, treatment with antidepressant was associated with a 30% decline in risk of MACE (Hazard ratio [HR] = 0.697; 95% confidence interval [CI] = [0.504, 0.964]; p = .029). A 46% reduction in risk was reported with antidepressant therapy among those without CVD (HR = 0.542; 95% CI [0.299, 0.981]; p = .043). Interestingly, patients with depression had a 33% lower risk of MACE associated with antidepressant use (adjusted HR = 0.674; 95% CI [0.440, 1.033]; p = .07). It is possible that antidepressant drug therapy may be cardio-protective among patients presenting for stress testing independent of risk factors including CVD and depression.
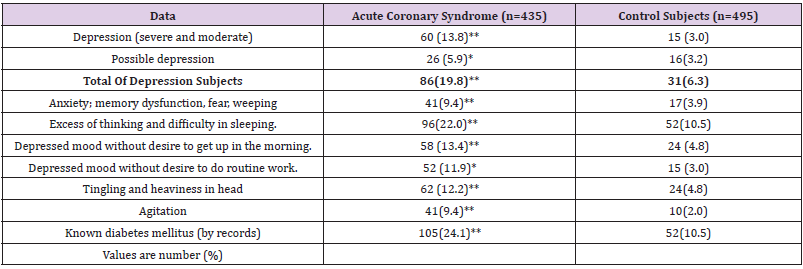
Recently, Tawakol et al. have demonstrated that emotional stress such as depression can increase amygdalar activity in the brain, which could be examined as tremors in the amygdala by Functional Magnetic Resonance Imaging (fMRI) [12-14]. The activation of amygdala was associated with increased bone marrow activity and inflammation with increased hsCRP [12]. A recent case study revealed that the incidence of depression was three-fold higher among ACS patients compared to the control group (Table 1). Depression is one of the most important mental disorders that have adverse effects on the brain as well as on the cardiovascular system. A large number of systematic review articles as well as meta-analyses of epidemiological studies reported the relation between depression and the risk of Coronary Artery Disease (CAD), which had some limitations [4-11]. In a meta-analysis comprising of 893,850 subjects (59,062 CAD cases), the period of follow-up ranged from minimum 2 years to 37 years. The Relative Risks (RRs) were significant 1.30 (95% CI: 1.22-1.40) for CAD and 1.30 (95% CI: 1.18-1.44) for myocardial infarction. Further analysis of subgroup by duration of follow up, the RR of CAD was 1.36 (95% CI: 1.24- 1.49) for less than 15 years follow-up, and 1.09 (95% CI: 0.96-1.23) for equal to or more than 15 years follow-up [9]. These findings indicate that depression may have independent association with a significantly greater risk of CAD and myocardial infarction. A more recent meta-analysis assessed the association between depression and the risk of myocardial infarction and coronary death [10].
Table 1: Frequency of depression and its characteristics in patients with acute coronary syndrome and controls.
In another meta-analysis including 19 eligible cohort studies with 323,709 participants, 8,447 cases of myocardial infarction and coronary death were reported during follow-up ranging from 4 to 37 years. The pooled adjusted HRs for patients with depression (vs. those without) were 1.22 (95% CI: 1.13-1.32) for combined myocardial infarction and coronary death, 1.31 (95% CI: 1.09–1.57) for infarction alone (9 studies), and 1.36 (95% CI: 1.14-1.63) for coronary death alone (8 studies). The increased risk of infarction and coronary death associated with depression was consistent using modified inclusion criteria across most subgroups, and after adjusting for possible publication bias [10]. Effective prevention and treatment of depression may decrease such risk. Insomnia and difficulty in initiating sleep are important characteristics of depression. In a recent meta-analysis, 15 studies including 23 cohorts were assessed [11]. Positive associations were observed between difficulty initiating sleep, difficulty maintaining sleep and non-restorative sleep with risk of cardio-cerebral vascular events. The pooled relative risks and 95% confidence intervals were 1.27 (1.15-1.40), 1.11 (1.04-1.19) and 1.18 (1.05-1.33), respectively. However, less evidence existed to support the conclusions about the association between early-morning awakening and cardio-cerebral vascular events. It is clear that insomnia symptoms of difficulty initiating sleep, difficulty maintaining sleep and non-restorative sleep were associated with an increased risk of future CVDs [11].
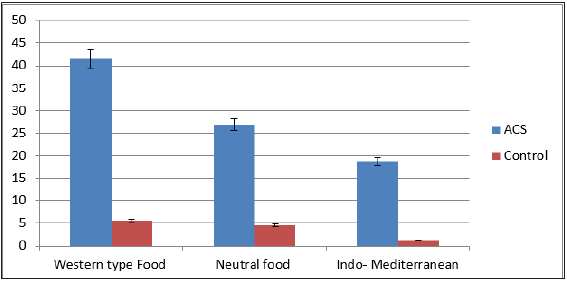
Patients with major depression show significantly higher median (interquartile range) plasma triglycerides levels and significantly lower HDL-cholesterol levels compared to subjects without depression [15,16]. In a case-control study design including 435 patients with ACS, comparison was made with 495 age- and gender-matched control subjects [3]. Depression as risk factor of ACS was assessed by validated questionnaires. The incidence of depression (19.8 vs. 6.3%, P<0.001) and increased intake of Western-type foods were significantly more common among ACS cases compared to the control group (Tables 1 & 2). The consumption of Indo-Mediterranean foods and blood nitrite concentrations were significantly lower among ACS patients as compared to the control group. After adjustment for age and BMI, depression was positively and strongly associated with ACS (P<0.001), as shown by odds ratios and their 95% confidence intervals. Depression (males: 0.33 (0.29- 0.38), P<0.001; females: 0.29 (0.23-0.35), P<0.001) and Westerntype foods intake (males: 0.44 (0.38-0.53), P<0.001; females: 0.47 (0.41-0.53), P<0.001 were significantly and strongly associated with ACS (P<0.001). Indo-Mediterranean food intake-0.46 (0.38- 0.48),P<0.001, and females-0.43 (0.37-0.47), P<0.01; and blood nitrite (males: 0.61 (0.51-0.75), P<0.01; females: 0.58 (0.43- 0.72), P<0.01, were inversely and weakly associated with ACS (P<0.02). The study revealed that depression, Western-type food consumption and high blood angiotensin converting enzyme were significant risk factors of ACS. Indo-Mediterranean type food intake and blood nitrite showed beneficial effects on risk of ACS. Figure 1 shows that incidence of depression was significantly more common among subjects consuming western type of diet compared to those eating Indo-Mediterranean diets. After a follow up of 2 years, depression was significantly associated with all-cause mortality. Of 435 patients with ACS, 87 died due recurrent cardiovascular events as given in Table 3. Almost half of these victims were suffering from depression. It is not absolutely clear that how many patients were suffering from depression before the ACS and in how many of them, depression was the result of ACS [18-21]. Depression may be associated with deficiency of angiotensin converting enzyme as well as serotonin, and treatment with antidepressant drugs may be protective [20-22]. RAAS may be a new target for treating depression [3,20]. An experimental study reported that acute MI can cause neuro-inflammation in the tissues in the brain and other body systems with increase in cytokines which may lead in to depression and diabetes as well as increased risk of recurrent cardiovascular events [19,22].
Note: ACS = Acute coronary syndrome. Values are number (%), P-values were obtained by Chi square test by comparison of depression in ACS with control group and within groups. *P < 0.01, **P < 0.001.
Table 3: Frequency of depression among patients with cardiovascular events in acute coronary syndrome group and control group after 2 years of follow up.
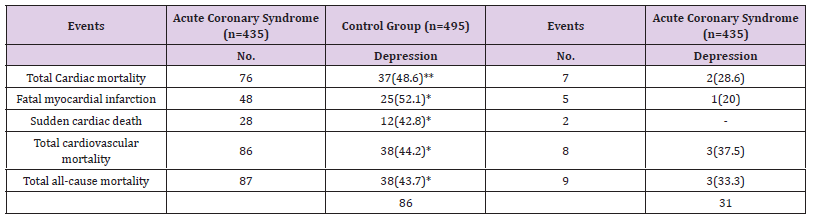
Note: Values are number (%), **=p<0.0001, *=p<0.001. (11 patients and 10 control group subjects lost in follow up.
Figure 1: Association of depression with food consumption pattern, indicating high incidence of depression among subjects consuming western type foods, graded decrease with neutral food and lowest with Indo-Mediterranean food intake in the ACS group. (modified from reference 3).
There is evidence that Selective Serotonin Reuptake Inhibitors (SSRI) can influence neurotransmitter serotonin which is used by nerves in the brain to send messages to one another. These chemical messengers are released by one nerve and taken up by other nerves to maintain memory function. Neurotransmitters that are not taken up by other nerves are taken up by the same nerves that released them which is termed “reuptake.” SSRIs work by inhibiting the reuptake of serotonin, an action which allows more serotonin to be available to be taken up by other nerves [16,17]. Depression is an associated risk factor among patients with Chronic Heart Failure (CHF) and may predispose complications in these patients [16]. There is only limited information on long term safety and efficacy of these agents (SSRIs) among these patients. A recent doubleblind trial examined the effects of escitalopram for 24 months in patients of CHF with depression to know its effects on mortality, morbidity, and mood. In addition to optimal heart failure therapy, patients (n=372) were randomized to receive escitalopram (10- 20 mg) or identical placebo for a period of 24 months [16]. After a median follow up of 18.4 months (n = 185) on escitalopram therapy and 18.7 months (n = 187) on placebo, the death or hospitalization occurred in 116 (63%) subjects and 119 (64%) victims respectively. The mean sum score for depression reduced from 20.2 at baseline to 11.2 at 12 weeks in the treatment group. However, in the placebo group, it decreased from 21.4 to 12.5. It is clear that in patients with CHF, with low ejection fraction, along with depression, escitalopram administration for 18 months verses placebo, caused no significantly reduction in all-cause mortality or hospitalization, without any significant improvement in depression [16].
In subjects with ACS, depression may predispose more complications, but data are scanty on the effects of antidepressant therapy on long-term prognosis in such patients. In a recent study among patients with ACS, the effects on long-term major adverse cardiac events of depression were examined [17]. All 300 patients with recent ACS and depression were randomly assigned either escitalopram in dosages of 5, 10, 15, or 20 mg/d (n = 149) or identical placebo (n = 151) for 24 weeks. After a median follow up of 8.1 years, there was a significant decline in MACE; 61 vs 81 patients (40.9% vs 53.6% respectively) in the escitalopram group compared to placebo (hazard ratio [HR], 0.69; 95% CI, 0.49-0.96; P = .03). The incidences for all-cause mortality were 20.8% vs 24.5%, for cardiac death, 10.7% vs 13.2%; for MI, 8.7% vs 15(P = .04), and for PCI. It is clear that in subjects with depression after recent ACS, 24-week therapy with escitalopram compared with placebo can cause a lower risk of MACE. There is a need for more research at different centers to demonstrate if such therapy can be the generalized with similar results.
It is possible that a lack of benefit on treatment with escitalopram in patients with depression with ACS may be due to confounders such as unhealthy diet, tobacco and alcohol intake and diabetes which have independent adverse effects on both diseases [3,23,24]. Since treatment of depression with escitalopram is beneficial, it should be included in the management of patients with ACS suffering from depression. It has been demonstrated that ACS also causes neuro-inflammation, which may enhance the risk and severity of depression due to inflammation in the amygdala among these patients [6,19]. Thus, ACS has a bidirectional adverse effects on neurons and cardiomyocytes as well as endothelial cells.
In brief, depression has become a common problem among patients with ACS. The incidence of depression among patients with ACS may be approximately 20% which is twofold more compared to general population in developed countries. Treatment of depression by administration of drug therapy with escitalopram can cause significant decline in CVDs. Mediterranean style foods may also have beneficial effects on risk of MI as well as on depression.
International College of cardiology for providing logistic support to write this article.


