Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Emmanuel Rotimi Sadiku*1, Victoria Fasiku2, Oluranti Agboola3, Idowu David Ibrahim4, Oluyemi Ojo Daramola1,5, Jimmy L Olajide1, Williams Kehinde Kupolati6, Samuel Sanni3 and Mokgaotsa Jonas Mochane1,7
Received: December 24, 2018; Published: January 11, 2019
*Corresponding author: Emmanuel Rotimi Sadiku, Department of Chemical, Metallurgical and Materials Engineering, South Africa
DOI: 10.26717/BJSTR.2019.13.002353
Health workers are constantly exposed to infectious materials and pathogens while they provide care to the patients. There are plenty of chances for health workers to get affected by infection, so infection control measures are most necessary for health workers. By practicing infection control techniques, the health workers can avoid spreading microorganisms. This can be possible when there is up gradation of knowledge and attitude of health workers regarding PPE. A pre-experimental one group, pre-test-post-test study was conducted to assess the effectiveness of planned teaching program regarding personal protective equipment use among the students of GNM1st year at Maharaja Agrasen College of Nursing, Hisar. The study was conducted amongst 30 students of GNM 1st year by using structured knowledge questionnaire. The study findings reveal that only 43% study subjects had previous knowledge regarding PPE. The mean difference between pre-test and post-test score was 5.07 and it is statistically significant at 0.05 level of significance. The standard deviation of mean difference is 3.28 for pre-test and 2.89 for post-test. The paired ‘t” test value calculated is 7.31. Planned teaching program was effective to improve knowledge regarding personal protective equipment use.
Keywords: Nanotechnology; Antimicrobial Resistance; Microorganisms
The word antimicrobial has its origin from the Greek words: “anti”, “mikros” and “bios”, which mean: “against”, “little” and “life”, respectively. Hence, antimicrobial agents are generally known to be any substance or compound capable of killing (microbicidal) or inhibiting the growth (biostatic) of microorganisms [1]. The use of antimicrobial agents in the treatment of a wide range of infectious diseases have, been very effective, in the past decades. However, with the indiscriminate use of these antimicrobial agents, antimicrobial resistance has developed, by a broad strain of several microorganisms [2,3] and thus, it has become very difficult to manage several infectious diseases. Some popularly known microorganisms that have developed resistance to antibiotics include: Mycobacterium tuberculosis, Pseudomonas aeruginosa, Streptococcus agalactiae, Methicillin-resistant Staphylococcus aureus, Klebsiella pneumoniae, Methicillin-resistant Staphylococcus aureus, Escherichia coli and Salmonella typhi, amongst many others [4]. Antimicrobial resistance has led to an increased statistical value in the numbers of morbidities and mortalities caused by infectious diseases [5] and there is a disturbing economic impact on the medical and human cost [6]. The development of resistance to antimicrobial agents (antibiotics) by microorganism, cuts across all known classes of natural and synthetic compounds that are available for treating microbial infectious diseases.
The cost and complexities involved in the discovery of novel drugs have limited their synthesis and as a result, only a few new antibiotics have been produced since the emergence of antimicrobial resistance [7]. A variety of mechanisms has been linked to the development of resistance to antibiotics by microorganisms [8]. The most common of all mechanisms, being the inactivation of antimicrobial agents via the enzymic degradation of the drug by hydrolysis, group transfer or redox mechanisms [9,10]. The global rise in drug resistance by disease-causing microorganisms has become a pressing subject, thereby, posing a very dangerous public health issue [11-13]. Therefore, it is paramount for new and more effective strategies to be developed by synthesizing new antimicrobial agents or modifying the already existing ones in order to enhance their antimicrobial activity [3]. This has been significantly achieved by employing new technologies, such as: nanotechnology, its implication in combating resistance faced with the use of conventional methodology is briefly summarized in this mini review.
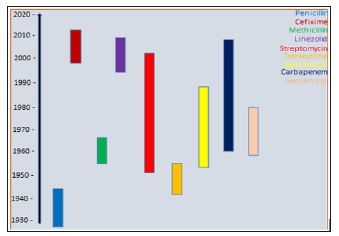
Prior to the year 1930, there was a remarkable breakthrough in the treatment of infectious diseases by using antimicrobials following the discovery of penicillin. Subsequently, other antibiotics, such as: cefixime, linezolid, gentamicin, carbapenem, methicillin, vancomycin and streptomycin, were discovered [14,15]. These antibiotics were extensively employed in treating microbial infectious diseases as a result of the numerous benefits associated with their usage. The mode of antimicrobial actions of these agents varies, based on their structural nature and the degree of their affinities to the sites of the intended targets in the cells of the microorganism (bacteria) [1]. Unfortunately, over the years, these drugs (antibiotics) as well as the method of drug delivery appeared to have failed due to the development of drug (antibiotic) resistance by these microorganisms [16]. Microorganisms, especially bacteria have developed ways such as inactivation of enzyme, reduction in cell permeability, alteration in target site/enzyme, protection of target site by the formation of biofilms as mechanisms to resist antimicrobial agents (antibiotics) [5]. Thus, the route of the conventional approach of treating infectious diseases, can be very difficult. Figure 1 below shows an estimated duration of the time of the discovery of these antimicrobial agents and the year they developed antimicrobial resistance.
Figure 1:Some examples of antibiotics, year of discovery and year of antimicrobial resistance development.
Limitations: It has been observed that there is a concurrent exhibition of antimicrobial resistance by pathogenic microorganisms on most of the old and new antibiotics used in clinics and hospitals [17]. This has been associated with the limitations of the conventional dosage forms used in combating infectious diseases caused by microbes. Some of these limitations include, but are not restricted to, the following [18-20]:
a) Inadequate concentration at target infection sites
b) Poor penetration of the antibiotics
c) Exposure of antimicrobial agents to healthy sites
d) Unfavorable side effects
e) Poor patients’ compliance
f) Ultimately, development of resistance by microorganisms
This implies that if these limitations are not overcome, antimicrobial resistance will inevitably; follow with the use of antibiotics [21]. Therefore, in order to avoid sliding back to the era of pre-antibiotic, a judicious modification of existing antimicrobials and the method of delivery must be developed.
Nanomedicine, which is a branch of nanotechnology, has experienced significant advancement in diagnosis, monitoring, drug delivery and control of diseases [4]. The limitations of conventional drugs and the methods employed for combating antimicrobial resistance, have prompted researchers from multidisciplinary fields worldwide, to explore the potential applications of nanotechnology in order to overcome antimicrobial resistance. This has led to the development of novel and more effective antimicrobial compounds as well as more effective strategies against antimicrobial resistance [22,23]. The advances made in recent years in the biomedical field, have offered new therapeutic agents and novel delivery systems that can target the infected site(s) [5]. The use of materials with nanosized (nanomaterials) is rapidly developing in order to overcome most of the antimicrobial resistant strain microorganisms. Some of these materials have inherent antimicrobial properties and can deliver antibiotics to targeted sites at the same time [5].
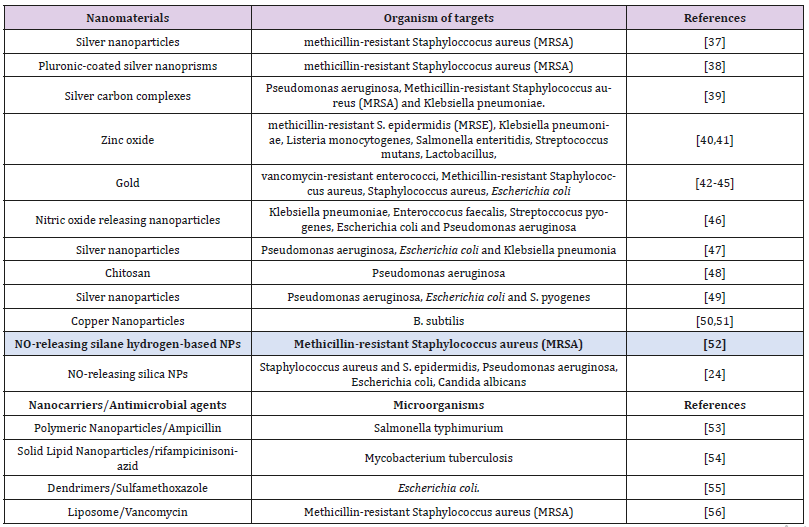
Nanoparticles, however, stand out as the mostly widely employed nanomaterial due to their interesting properties, such as enhanced drug stability and solubility [24], biocompatibility and ability to modulate their release via stimuli control [25], ease in the methods of synthesis [26] and possibility to functionalize them with different (bio) molecules. These features provide major advantages over the conventional therapies in the treatment of infectious diseases, caused by intracellular antimicrobial resistant pathogens [5]. Nanomaterials exhibit their antimicrobial activities by interacting with the cell wall of the bacterial directly, preventing the formation of biofilm, production of reactive oxygen species, triggering the immune response of the host as well as interacting with DNA and proteins [5,27-36]. Table 1 below summarizes some of the studies carried out on various strains of antimicrobial resistant microorganisms. The various nanotechnology approaches above and even many more have shown promising potentials as alternate methods of circumventing antimicrobial resistance in microorganisms.
Table 1: Types of nanomaterials/antimicrobial agent used in combating antimicrobial resistance in different microorganisms.
The development of antimicrobial resistance by microorganisms, has been linked to the difficulties encountered in treating infectious diseases. This has led to the development and application of nanotechnology approach in circumventing the limitations of the conventional drug dosage forms. Several in-vitro and in-vivo studies have shown to be very promising as reported in some of the references cited in this mini review. Therefore, it is highly anticipated and envisaged that in few years’ time, the issue of antimicrobial resistance is expected to become a thing of the past because it is hoped that a far more efficient therapeutic method for combating antimicrobial resistance will be in the market. Although, these new approaches tend to be greatly promising, it is encouraged that further researches should still be undertaken by scientists from various fields in order to completely provide a long-lasting solution to antimicrobial resistance. This will indeed bring and restore a greater hope in eradicating antimicrobial resistance globally, thus leading to a probable longevity of human beings and a healthier community.


