Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Izquierdo Gómez K1, González Navarro B2, García Ortiz de Zárate F3, Arranz Obispo C3, Jané Salas E3 and López López J3*
Received: December 02, 2018; Published: December 10, 2018
*Corresponding author: José López López, Section of Oral Medicine, School of Dentistry, L’Hospitalet de Llobregat Barcelona, Spain
DOI: 10.26717/BJSTR.2018.11.002164
The third molar extraction is a common practice in oral surgery [1,2]. They are present in 90% of the population and around 33% of patients have at least an impacted third molar, whose cause is associated to genetic and environmental factors [3]. The possible complications related to the presence of impacted or retained inferior third molars (infectious, inflammatory, tumors, or neurological complications) forces the surgical extraction in many occasions, either for therapeutic or prophylactic reasons. The surgical exodontia of the inferior third molar implies several postsurgical complications, such as damage into the structures adjacent to the third molar (nerves, bone and soft tissues), and the tissues near the surgical area (tongue and lips among others). In the postsurgical period, pain, inflammation, trismus, early or late infection, or paresthesia have been described. Therefore, designing and implementing an optimum flap would facilitate a better technique, better visibility for the surgeon and minimize complications [4]. There are different types of flaps to perform third molar surgery. The most commonly used are:
a) Partial Newmann flap (triangular flat, with three corners or vertical incision);
b) Modified partial Newmann flap (modified triangular, bayonet, modified Szmyd or L-shaped incision) and
c) Envelope flap (Szmyd flap).
Since there is no agreement on the type of flap which is most advisable, in this review we will try to analyze the advantages and disadvantages of the three most used flaps.
A literature review of the last 15 years was performed (since 2001 to 2017) introducing keywords “flap” & “third molar” in the Pubmed Medline database. Only those studies which compared at least two or three types of the flaps analyzed (the envelope flap, partial Neumann flap or partial modified Neumann flap), in English or Spanish and clinical trials with a minimum level of incidence 1b, 2b were included [5]. Jadad criteria were applied to the clinical trials [6].
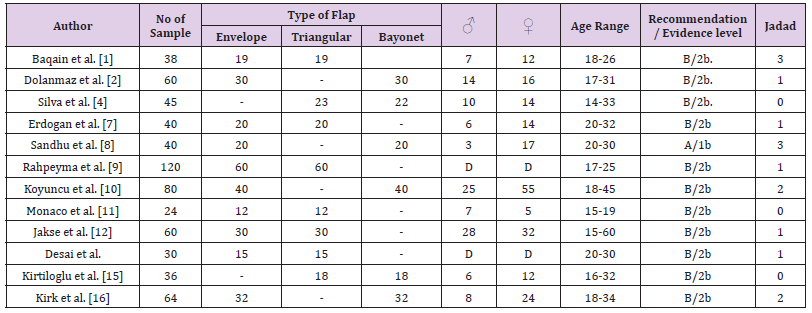
The initial search revealed 134 articles. After reading the abstracts, or the full text if necessary, and exclusion of those which did not fulfill inclusion criteria, 14 articles were selected (Figure 1). Out of these resulting studies, 1 was evidence level 1b and level A of recommendation [7] and the remaining 13 were evidence level 2b and level B of recommendation (Table 1). From the analyzed articles, 2 studies had a Jadad index 3, 3 had 2, 6 had 1 and 3 had an index of 0 (Table 1). All were prospective randomized clinical trials except 3 that were not referred to as randomized [4,8,9] and only 1 study was a double blind one [7]. The reviewed clinical acts represent a total of 705 flaps, 298 are envelope flaps, 231 Newmann partial flaps and 176 Newmann partial modified flaps (Table 1). In most of the clinical trials except in the study by Monaco et al. [8] the majority of patients were females [10-12] and 3 studies did not specify the male/female ratio. The age range was between 15 to 60 years old (Table 1). While reading the analyzed articles we found two systematic reviews that analyzed 58 and 33 [3,13] studies respectively
Table 1: Relation between the clinical trials with data referred to the “n” analyzed, sex, age, type of flap, recommendation and level of evidence (5) and Jadad index (6).
On analyzing the data obtained we observed that the different clinical trials do not usually compare the same flaps and that they have a different sample size and level of evidence (Table 1). We found some difficulties while classifying the flaps since the authors of one or other studies have slight differences between their flaps, and a clear classification that would unify criteria allowing us to include flaps in one type or other doesn’t exist. We grouped the results obtained in 5 different items together. In the first three we analyzed the aspects that distinguishes each type of flap, in the fourth the studies that did not find differences and the final considerations in the fifth.
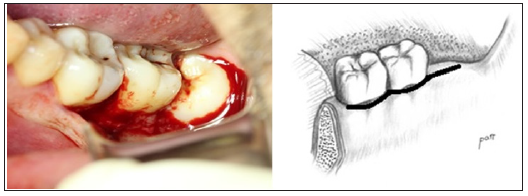
Authors like Baqain et al. [1] observed that the envelope flap (Figure 2) produces statistically significant less inflammation and trismus compared to the triangular on the second and the seventh day after surgery, and on the 7th or 14th days respectively. But, the inflammation stops being significant on the 14th day. Erdogan et al. [13] who also compared the envelope flap to the partial Newmann flap, referred that the envelope flap results in less inflammation after surgery and better results in pain control, the difference being statistically significant on day 3 and 7 after surgery. Borgonovo et al. [14] concluded that the envelope flap is the simplest to make and the easiest to suture. In agreement with these authors, Sandhu et al. [7] described an increase in dehiscence on the distal surface of the second molar, and the first added that there is more post-op pain than with the bayonet flap. According to Rahpeyma et al. [10] there is also more dehiscence in the envelope flap with respect to the triangular, but it wasn´t statistically significant. Koyuncu et al. [15] reported a significantly greater inflammation on day 2 and 7 after surgery with respect to the modified partial Newmann flap. Monaco et al. [8] found a greater probing depth on the seventh day of the postoperative period than in the case of the triangular flap. However, this value is insignificant at the 3 months mark. Finally, Borgonovo et al. [14] pointed out that it is more difficult to carry out ostectomy in this type of flap, compared to the other two.
Figure 2: Envelope flap.
(A) Clinical image.
(B) Diagram. It is performed beginning at the level of the retromolar triangle, in the area distal to the second molar, till the distal line angle of the second molar and the second or the last part is made from the distal aspect of the second molar till the mesial part of the first molar following the gingival sulcus.
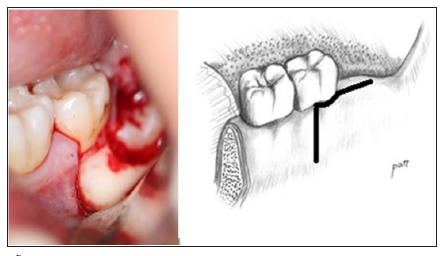
Triangular flap with three corners or with vertical incision (Figure 3) Borgonovo et al. [14] suggested that this flap could be the one of choice in patients with difficulties in mouth opening (< 30 mm). Erdogan et al. [13] also talked about less inflammation and less pain after surgery than with the envelope flap. In the study by Baqain et al. [1] they described an earlier return to the preoperative probing depth than with the envelope flap. Jakse et al. [16] also compared the partial Newmann flap with the envelope flap and agreed that there is a better primary healing and a less cases of dehiscence. Borgonovo et al. [14] alludes that, unlike the envelope flap, the partial Neumann flap shows an adequate area to surround the structures and to perform ostectomy. Disadvantages of the partial Neumann flap include poor preservation of a keratinized gingiva and according to Borgonovo et al. [14] more bone resorption (greater bone exposition), as with the bayonet flap. In addition, Desai et al. [11] comparing it with the envelope flap showed more hematomas, more dehiscence and caused greater distal periodontal pocket in adjacent teeth.
Figure 3: Partial Newmann flap.
(A) Clinical image.
(B) Diagram. It is performed with a first incision at the level of the retromolar triangle, in the area distal to the second molar, till the distal line angle of the second molar, it is circled following the sulcus till the mesial aspect, where the vertical releasing insicion is made till the end of the vestibule, in a forward and downward fashion.
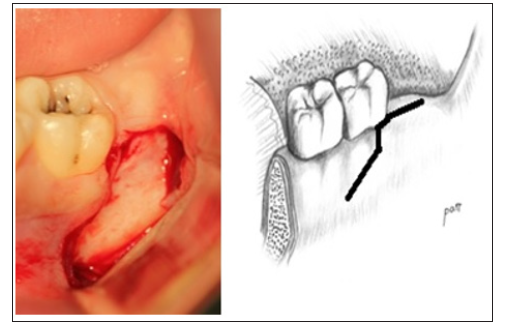
Modified triangular, bayonet or modified Szmyd or L-Shaped incision (Figure 4). Kirtiloglu et al. [9] reported a better primary healing than the triangular flap and Koyuncu et al. [15] demonstrated significantly less postoperative pain during the first 4 days after surgery with regards to the envelope flap. Silva et al. [4] stated that this flap allowed for a less traumatic surgery than the partial Newmann flap. This aspect could lead to a better healing of the surgical wound, along with a more comfortable postoperative period, with less edema and dehiscence, thus reducing postoperative complications. On the other hand, Borgonovo et al. [14] claimed that this flap, like the triangular flap, could be useful in patients with difficulties in mouth opening (< 30 mm).
Figure 4: The modified partial Neumann flap.
(A) Clinical image.
(B) Diagram. It is similar to the previous flap, but attempts are made to conserve the attached gingiva and the gingival sulcus in the cervical-vestibular area of the second molar. In order to do so, the second incision is made approximately two millimeters from the first and it is directed forward, parallel to the neck of the second molar, till the mesial surface of this tooth, at which point the vertical releasing incision is made downwards towards the bottom of the vestibular sulcus.
Koyuncu et al. [15] in their studies found a greater incidence of alveolar osteitis than in the envelope flap but it wasn’t statistically significant. The first one claimed a longer surgical time, even though it was statistically insignificant. Kirk et al. [17] emphasizes more on the increased inflammation that occurs on the second day after surgery. As mentioned previously, Borgonovo et al. [14] talked about greater bone reabsorption than in the envelope flap.
Different authors have derived conclusions that the flap election is not important. They considered other factors more important, or they did not find significant results to choose one type or other. In this way, Dolanmaz et al. [2] inferred that the degree of impaction, nicotine consumption and the duration of the surgery (this last factor shared by Sandhu et al. [7] have clearly more influence on the primary healing of the wound than the flap design. In the study by Sandhu et al.7 they found that there is no difference in the degree of inflammation between the different flaps mentioned above. These authors, along with Kirk et al. [17] did not find any type of relation between the type of flap and postoperative pain and they did not refer any difference in the presence of dehiscence. Both Koyuncu et al. [15], did not show differences in the maximum incisal opening. Regarding the presence of alveolar osteitis, it was insignificant for Sandhu et al. [7]. In the study by Koyuncu et al. [15] they described that there were no demographic differences. Even for Monaco et al. [8] the flap election didn’t seem to be important in the appearance of complications, nor in the amount of medication needed (this wasn’t important for Erdogan et al. either 14).
For both of them Erdogan et al. [8,13], the level of periodontal healing did not have any importance in the flap selection. When they compared the triangular flap and the bayonet flap, Kirtiloglu et al. [9,18] found that there weren’t significant differences in the plaque index, gingival index and probing depth , (this last one was also not important for Arta et al. [12], when compared to the free gingival margin, the clinical level of insertion and the bone level (these two last factors for Rosa et al. [18] didn’t influence the flap design). Desai et al. [11] did not find any significant differences between the envelope and the triangular flap regarding visibility, accessibility, bleeding and sensibility of the adjacent teeth. In the study by Baqain et al. [1] work, they concluded that the flap to be used in young patients should be in accordance with surgeon’s preferences, taking the patient’s needs and his oral hygiene into account. Karaca et al. [3] argued that if there is a problem related to the soft tissues around the mandibular second molars, it is not a result of surgery or technique, but of some other process and that more comparatives studies are needed to determine the best technique to be used.
Therefore, it can be inferred that even though there are a variety of flap designs to approach impacted third molars, the conclusions in the articles that we have studied are not very clear. Most of them have small sample size and do not take other possibly important variables into account. Even though we have summarized the differences in favor or against the different types of flaps with reference to pain, inflammation, dehiscense, maximum interincisal opening, periodontal health, etc. in Table 2, the truth is that most of the results are not statistically significant. Moreover, in a few weeks or at most in a few months, the results are equivalent. Many authors consider factors such as the degree of impaction of the third molar, duration of the surgery, or patient’s toxic habits more important among others. However, small variations exist within these three types of flaps, so we have tried to unify criteria
Modified partial Newmann flap seems to be the most appropriate flap for the exodontia of the third molars considering that its benefits outweigh the risks. However we have a great diversity of flaps and we must personalize each case depending on the characteristics of each patient and on the skill and preference of the surgeon. More detailed studies are needed with bigger and well-designed samples.


