Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Adrian Kahn*1, Ronen Mogilner2, Lazar Kats2 and Dan Dayan2
Received: September 29, 2018; Published: October 09, 2018
*Corresponding author: Adrian Kahn, Department of Oral and Maxillofacial Surgery, School of Dental Medicine, Tel Aviv University, Tel Aviv 69978, Israel
DOI: 10.26717/BJSTR.2018.09.001844
Coronectomy, a surgical technique that has been developed for impacted mandibular third molars that their roots are in intimate vicinity to the inferior alveolar nerve, refers to the removal of the tooth crown while retaining the root/s within the jawbones. We report the first case in which coronectomy was successfully used to treat a case of a partially impacted mandibular third molar with recurrent pericoronitis in a patient diagnosed with florid osseous dysplasia. In this condition the involved bone features poor cellularity and vascularity, therefore increasing the risk of abnormal healing and secondary infection following surgical procedures. We suggest that coronectomy should be considered also in other conditions that affect the quality of the jawbones that result in contraindication for complete third molar extraction.
Coronectomy has been developed as a relatively new treatment modality for mandibular third molars, when surgery is necessary in case of an intimate anatomic proximity between the inferior alveolar nerve (IAN) and the roots of these teeth [1,2]. The procedure of coronectomy intentionally retains the roots and the rational is to decrease the prevalence of IAN injury compared with the conventional total removal of the lower third molar [3]. Osseous dysplasias are a group of idiopathic processes located in the tooth-bearing areas characterized by replacement of normal bone by fibrous tissue and metaplastic bone[4] When osseous dysplasias occur bilaterally in the mandible or even involving all jaw quadrants, the condition was termed as florid osseous dysplasia (FOD) and was first described by Melrose et al [5]. FOD is commonly seen in middle aged black females and is quite rare in Caucasians and Asians [4,6,7].
These lesions are clinically asymptomatic and may be found as incidental radiological findings presenting as multilocular radiopaque lesions within peripheral radiolucent lesions located in two or more quadrants usually in tooth-bearing areas [4,6]. Lesions are not always limited to the periapical alveolar bone and they also can involve the interradicular bone up to the level of the cemento- enamel junction. Rarely, the patient may complain of dull pain and alveolar sinus tract may be present, consequent to the progressive alveolar atrophy under ill-fitted denture or following extraction of teeth in the affected area [8]. Although biopsy is required for definitive diagnosis, clinicians generally try to avoid surgical procedures in FOD patients as these might lead to unsatisfactory healing and infection due to the poor cellularity and vascularity of the bone [9]. Therefore, in some FOD cases, the diagnosis is established based on characteristic radiological features without histopathologic confirmation [10]. It is the purpose of this study to report for the first time the use of coronectomy in a FOD patient with lower jaw third molar chronic pericoronitis aimed to avoid alveolar bone infection and atrophy due to the extraction procedure.
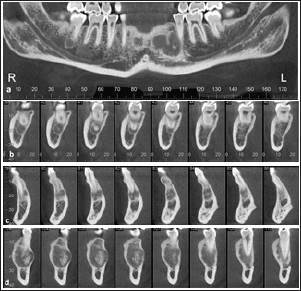
A 31-year-old female was referred to the Department of Oral and Maxillofacial Surgery, School of Dental Medicine, Tel Aviv University due to a complain of several episodes of swelling and pain in the lower right third molar. The patient was diagnosed five years ago with FOD based on the clinical and radiographic findings. Extraorally, the clinical examination revealed right submandibular lymphadenitis; no limitation on mouth opening was present. Intraorally, edema and tenderness on palpation of the operculum surrounding the right lower third molar consisted with a diagnosis of pericoronitis (Figure 1). The radiographic findings are shown in Figures 2 & 3. On the panoramic view, the involved third molar showed a slightly distoangular inclination, with the distal part of the crown being associated with a radiolucent, corticated area at the level of the cemento-enamel junction. Arrows point to multifocal mixed radiopaque-radiolucent lesions in the periapical regions throughout the mandible (Figure 2). The cone beam computed tomography (CBCT) reveals multifocal mixed hypodense- hyperdense lesions in several periapical regions (Figure 3).
Figure 2: Panoramic x-ray shows the slight distoangular position of the mandibular right third molar. Arrows point to multifocal mixed radiopaque-radiolucent lesions in the periapical regions throughout the mandible.
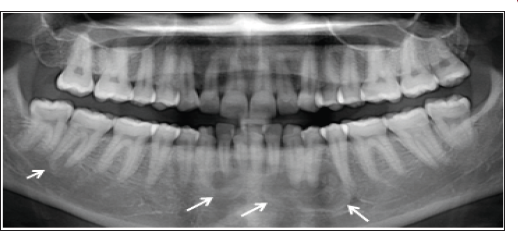
Figure 3: CBCT: A (a) panoramic and (b, c, d) cross-sectional reconstructions: (b) area of second right molar, (c) area of second right incisor, (d) area of left premolars of the CBCT bone windows images: multifocal mixed hypodense-hyperdense lesions seen in the periapical regions of #47, 42, and 33-35.
Due to a history of recurrent episodes of pericoronitis (the present one being of a mild-moderate severity but previous ones being considerably more intense and debilitating), it was decided to extract the mandibular right third molar. To avoid any possible post-extraction FOD-related complications, coronectomy was suggested as a practicable option to be applied in the present case. The patient signed on a form of informed consent for this procedure. Local infection control was achieved by oral Amoxicillin 500 mg tid, and 0.12% chlorhexidine mouth rinses twice a day, beginning two days prior to the surgical procedure. Under local anesthesia, a lower right full thickness distally released envelope flap was reflected. No lingual retraction was used. An initial horizontal cut with a highspeed was made. The cut included almost all the tooth diameter, avoiding the lingual aspect of the crown to avoid lingual nerve injury. The crown was gently broken off, without excessive apical pressure. The cut surface of the tooth was trimmed to 3 mm below the bony margin (Figure 4). The pulp was left untouched and the roots were checked for any mobility. The flap was advanced for full coverage primary closure and then sutured with 4-0Vicryl sutures. The post-operative course was uneventful. At follow up visit, 12 months after the procedure, the surgical site healed satisfactorily with no impact on the lesion of FOD in the second molar (Figure 5).
Figure 5: 12 months post-operative panoramic view of the "cor- onectomized" mandibular right third molar. No impact on the lesion of florid osseous dysplasia in the second molar.

Coronectomy is aimed to decrease the prevalence of IAN injury when there is a clear indication for third molar surgery and there is a close anatomic relationship between the IAN and the roots of the lower third molars [1,2]. The crown of the partially impacted lower third molar is often the cause for dental caries, food impaction, or pericoronitis that cause discomfort and pain to the patients. By removing only the crown and retaining the roots behind, the risk for damage to the IAN is minimalized or even avoided. Post-surgical pain within the first postoperative week is generally expected, however clinical trials have shown that following coronectomy it is less compared with the surgical removal of the entire third molar [11,12]. Root migration is another finding in studies on coronectomy of the lower third molars [13,14].
The presented case is the first to use coronectomy in a FOD patient for reasons other than the concern for damage to the IAN. In general, attempts are made to preserve teeth by conservative treatment approaches in patients diagnosed with FOD. This is because teeth extraction in FOD can lead to infection, bone sequestration and osteomyelitis due to the avascular nature of the involved bone [15,16]. This complication is more likely to occur and at higher severity in the context of extraction of impacted third molars that usually is associated with extensive removal of bone around these teeth and therefore requires a remarkable healing process. Coronectomy could be a feasible treatment option for lowering the risks associated with extraction of third molars in FOD. Furthermore, we suggest considering coronectomy for the treatment of impacted third molars planned to be extracted, also in other conditions that affect post-operative healing of the jawbones, such as use of bisphosphonates, post-irradiation, osteoporosis and osteopetrosis.


