Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Joseph Bakhach*, Elsa Bakhach, Bachar Chaya and Reem Karameh
Received: August 14, 2018; Published: August 23, 2018
*Corresponding author: Bakhach J, American University of Beirut Medical Center, Riad El Solh, Beirut 1107-2020, Lebanon
DOI: 10.26717/BJSTR.2018.08.001642
Aim: The ideal flexor tendon repair should be a simple procedure and should provide enough strength to the tendon in order to ensure a good anatomical stumps connection. The surgery must be performed without impairing either the tendon shape or the gliding process, particularly in zone II. Many experimental attempts have been made by using a barbed suture in the repair of the finger flexors focusing particularly on the mechanical properties of the suture. All the devices previously used had either a circular cross-sectional area or were designed to be used on the skin and subcutaneous tissues. The aim of our research is to define the anatomical properties of the digital flexor system in order to set the ideal shape and dimensions for a barb wire, that can be used for the digital flexor tendon repair.
Methods: Twenty-four hands from fresh cadavers were dissected exposing the different finger flexor systems. The length of the different annular pulleys and the distance from the distal insertion of each pulley to the distal insertion of the Flexor Digitorum Profondus (FDP) were both recorded. In addition, the width, heights and cross-sectional diameter of all the FDP tendons were documented.
Results: The cross-sectional shape of the FDP tendon in zone II is elliptical. We have postulated that the wire device should have an elliptical shape in order for it to better conform with the tendon. The different measurements of the cross-sectional diameters - radioulnar (a) and dorsovolar (b) - of the FDP tendon of the different fingers have demonstrated that the mean ratio a/b is usually 1.5. Thus, the mechanical investigations should address wires with a mean cross-sectional area ratio of 1.5, 2, 3 and 4.
Conclusion: These anatomical studies revealed that the best shape of an intra-tendinous barb wire device should be elliptical rather than the available circular ones. From an anatomical perspective, the optimal cross-sectional area of the wire should be 1.5 but the final cross-sectional area ratio should be adapted according to the results of the mechanical testing results.
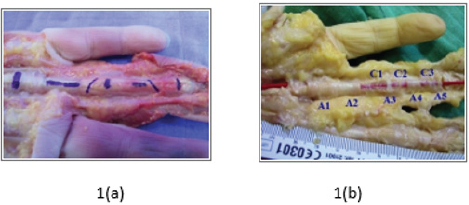
Finger flexor tendon repair is still one of the most challenging surgeries for a hand surgeon. This is particularly true when the rupture of the flexor tendon is localized to the zone II, also known as "The No Man's Land", that Bunnell described in 1918 [1,2]. This zone ranges from the insertion of the Flexor Digitorum Superficialis (FDS) distally to the palmar crease proximally. These difficulties are related to the unique anatomy of the flexor system in this particular zone. It is mainly composed of the flexor digital tube and the tendons of both the FDS and the FDP The flexor digital tube is formed by the succession of five annular pulleys 'A1 through A5" separated by three cruciform pulleys "C1 through C3". The name of these pulleys can be traced back to their anatomical structure and particularly to the orientation of the collagen bundles [3,4]. A ring shape for the annular pulley and a cross shape for the cruciform ones (Figure 1a & 1b).
Figure 1: 1(a) The flexor digital tube with the two tendons, the flexor digitorum superficialis and profondus and 1(b) The five annular pulleys separated by three cruciform pulleys.
All these structures are tightly arranged and work in a perfect dynamic coordination. This is due to its intrinsic gliding structures and endogenous fluids, that will lead to the optimal finger mechanics (Figure 2). Any alterations to the tendons or to the flexor digital tube (structure, volume or disposition) will impair the hand function drastically. In case of sharp injury to the fingers, the relatively superficial position of the FDP tendon, lying just behind the finger's volar skin, makes it prone to rupture[4]. The primary repair of the ruptured FDP tendon usually gives the best outcome. However, the following conditions should be respected for an optimal repair:
Figure 2: The flexor digitorum superficialis and profondus and the pulleys are tightly connected and work in perfect harmony.
a) One must take good care while manipulating the tendon's stumps; in order to avoid any additional iatrogenic trauma [5].
b) A strong tendon anastomosis should be performed; in order to prevent any gap formation during early mobilization.
c) The surgeon should make sure not to impair the tendon vasculature.
d) The surgeon should preserve the natural anatomy of the tendon.
A great number of surgical techniques for tendon anastomosis were described in the literature. In previous practice, a core suture with two strands, using non-absorbable material, was performed. A circumferential running suture (around the zone of anastomosis) was placed on top of the core suture, in order to reshape the tendon circumference [6]. Recent studies have shown that the number of strands in the core suture can be increased up to eight, with the aim to strengthen the solidity of the tendon anastomosis [7]. However, the more sutures we use, the more we cause trauma to the tendon. Further, trauma to the tendon will lead to a higher risk of secondary tendon rupture and to the formation of adhesions.
Failure of the flexor tendon repair can occur relatively early post-op, with the rupture of the tendon anastomosis occurring at the site of the connection. This rupture usually occurs between the seventh and the fifteenth day post-repair. It is triggered by the inflammatory process that weakens the tendons connection. This rupture is facilitated by one or a combination of the following:
a) The improper handling of the tendon stumps during repair.
b) The use of constrictive knot sutures that impair the blood flow to the stumps and jeopardizes the tendon healing.
c) The application of an early aggressive rehabilitation protocol [8].
Not only can flexor tendon repair failure occur early post-op, but also failure can occur relatively late post-op. This is largely related to adhesion formation. These adhesions are a normal component of the healing process (intrinsic healing). Yet, they can extend beyond the tendon structure (extrinsic adhesion) [9], gluing the tendon and the flexor digital tube together. This process will impair the normal gliding action and will limit the finger’s range of motion. In order to avoid the previously stated problems, many authors have thought of using a circular barb suture that will insert into the two stumps of the repaired tendon [10-14]. However, the main wire should have a more unique shape in order for it to be in perfect contact with the tendon. In order for the barbs to anchor efficiently into the tendon structure, they must be distributed along the surface of the wire, have an ideal shape and orientation, and enough mechanical properties. This will maintain the stumps connected while performing the physical therapy later on.
In collaboration with the Department of Mechanical Engineering of the Faculty of Engineering and Architecture at the American University of Beirut, numerous studies and experimentations have been made in order to compare the mechanical properties of the circular and elliptical cross-sectional shapes of the wire. These studies also aim at defining the ideal configuration "depth & cut angle" for the barbs in order for them to better anchor into the flexor tendon structure [15-17]. In parallel to these fundamental studies concerning the shape and the configuration of the barb wire, anatomical studies and investigations of the finger flexor digital tubes have been made. Further, we measured the dimensions of the FDP tendons of the different fingers in order to set the basis for the mechanical engineering team. This helped them define the specifications of the barb wire device that they opted to used. The results of our different anatomical investigations are reported in this article.
An anatomical dissection was carried on 24 hands of 12 fresh cadavers. The different flexor systems of the index, middle, ring and small fingers were all exposed and the following measurements were noted:
a) Length "L", of the different annular pulleys "A1, A2, A3, A4 & A5" on each finger
b) Distance "d", extending from the distal insertion of each pulley to the distal insertion of the FDP tendon,
c) Transversal diameters
d) Width "w" of the FDP tendons on each finger
e) Height "h" of the FDP tendons on each finger
f) The cross-sectional area of the FDP tendons of each finger.
This anatomical dissection was performed initially for the purpose of comparing the anatomy of the flexor system of the foot to the anatomy of the fingers in order to validate the possibility of transferring the whole flexor system of the second toe to replace the flexor system of any finger [18,19]. The Flexor Pollicis Longus (FPL) tendon was excluded from this experiment as the anatomy of the flexor system of the thumb rely mainly on a major pulley 'A1" and on only one tendon. This is a relatively simple anatomy when compared to the anatomy of the flexor system of the remaining fingers. The FDS was also excluded since when it crosses through zone II, its shape becomes relatively flat and thin hindering its connection to the barb wire.
For each finger dissected, the mean length of the annular pulley was calculated. Our results were compared to those obtained by Doyle [20] (who also measured the length of the five annular pulleys) and to the results obtained by Katzman [21] (who limited his anatomical study only to the A5 pulley) (Table 1). In addition, the mean distance, between the distal insertion of each pulley to the distal insertion of the FDP tendon, on the 24 anatomical specimens was calculated. Our results were also compared to those obtained by Doyle [20] and Katzman [21] (Table 2). This distance allows us to calculate, when necessary, the total length of the flexor digital tube of each finger, the length of the different cruciform pulleys (C1, C2 and C3) and the size of the surgical space of the FDP tendon in zones IIB and IIC.
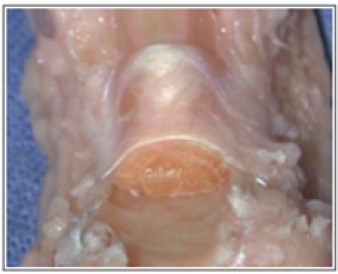
Finally, since the shape of the FDP tendon is elliptical, the cross-sectional diameters "radioulnar or width" and "dorsovolar or height" of the FDP tendons of the different fingers were recorded.These measurements were taken at the level of the mid second phalanx which corresponds to the zone IIB.
The cross-sectional area of each tendon was calculated according to the following formula:
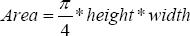
Our results were compared to the results obtained by Boyer [22] who also discussed the variation in the cross-sectional size of the different flexor tendons in the hand (Tables 3 & 4).
The finger flexor system is one of the most complex systems in the human body. In zone II, it is composed of a flexor tube that contains five annular and three cruciform pulleys. These pulleys hold the FDP and FDS tendons in multiple strategical places that are critical in the flexion process. Any minor disturbance to the components of this system, whether it was a trauma or an imperfect repair of a traumatic laceration, may lead to a major limitation in the fingers function. The difficulty in this reconstructive surgery lies not only in the anatomical restitution of the different parts but also on the functional recovery that aims at restoring a natural finger triple flexion.
Decades ago, great attention was given to the repair of lacerated flexor tendons. Many techniques have been reported that rely on the use of non-absorbable threads, oriented in a rectangular scheme, to hold the two stumps during healing. The most commonly used procedure was the "Kessler" suturing technique that required the use of two strands [23]. It was followed by the "Modified- Kessler" technique, a combination of the modifications proposed by Kirchmayr, Urbaniak and Pennington [24-26], that required the use of two or four strands. Finally, Savage et al. proposed to increase the number of strands up to eight in order to increase the strength of the repair [27]. All these suturing techniques require the implementation of one or two knots on the external surface of the tendon or inside the zone of connection.
The presence of knots was very controversial and considered to create a zone of weakness. When placed inside the zone of repair, it can disturb the tendon healing and generate an inflammatory response. Similarly, when located on the outside of the tendon, it can impair the gliding process and promote adhesion formation [28-31]. This pushed many authors to experiment with the fully barbed sutures. The unidirectional (V-LocTM 180, Covidien Inc, Mansfield, MA) or the bidirectional (Stratafix™ Spiral PDO Device, Angiothech, Ethicon). We can insert these sutures into the tendon specimens the same way we insert the normal braided polyester threads [32-37]. These barbed sutures have the main advantage in that they don't require the use of knots. Furthermore, they display a higher tensile strength with a better resistance to loading. This is mainly due to the presence of multiple anchors which prevent the threads from slipping. However, barbed sutures:
a) Do not exhibit better result in preventing the 2-mm gap formation at the zone of repair
b) If not well inserted it can create bulging and shape deformation of the zone of anastomosis
c) They can impair the stumps vascularity in case of high traction and when the number of strands exceeds two [38].
The use of intra-tendinous barbed device in flexor tendon repair is not new but none of the experimented devices were widely adopted [39,40]. All the experimented devices had a circular crosssectional shape with the barbs distributed in a circular way. Since the cross-sectional shape of the flexor tendons is elliptical, we have considered that the shape of the wire device should also be elliptical in order for it to better conform with the tendon architecture. Moreover, we have concluded that the barbs should be distributed on both sides of the ellipse major axis in order to recruit and anchor the maximum number of tendons. Prior to any mechanical studies, our anatomical investigations had demonstrated that FDS cannot benefit from the use of an intra-tendinous barb wire insertion, as previously mentioned. The FDP tendon however, has an elliptical shape and fits the requirements of this innovative device perfectly. The site of insertion of the barb device should ideally be in the centre of the ellipse (Figure 3). If two barb wires are planned to be inserted, they should be introduced on the transversal axis at the junction points between the first, second and third of this axis (Figure 4).
Figure 4: In red, the two points of entry when two barb wires are planned to be inserted into the FDP tendon.
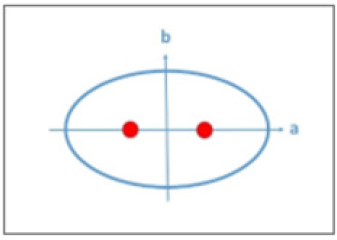
Evaluation of the length of the different parts of the flexor digital tube and the distance between the different annular pulleys have revealed that the FDP tendon can be better accessed when the rupture occurs in zones IIB and IIC. The cruciform C1 and C2 pulleys can be opened giving enough space to the FDP stumps without harming the A3 and A4 pulleys. Different studies have showed that part of A2 and A4, the most important functional pulleys, can be vented without impairing the function of the finger [41,42]. However, it is preferable not to vent any one of these annular pulleys (Figure 5). The different measurements of the cross-sectional diameters - radioulnar (a) and dorsovolar (b) - of the FDP tendon have demonstrated that the mean ratio a/b is usually 1.5. Thus, the mechanical investigations should address wires with a mean cross-sectional area of 1.5, 2, 3 and 4. The best ratio will be selected after the mechanical investigations.
These anatomical investigations have set the requirements for the design of an intra-tendinous barb wire device for FDP tendon repair. Further mechanical investigations should be performed in order to determine the best cross-sectional ratio of the wire ellipse in addition to the depth, cut angle, and orientation of the different barbs. Additional investigations are required in order to determine the numbers of barbs and the length of the wires that should be introduced into each stump (taking into consideration whether one, two or three wire devices are used). Finally, the biological interaction between the barbs and the tissues should be evaluated in order to better understand the mechanism of repair failure.
Medical and surgical part of this work: Bakhach J, Chaya B, Karameh R, Literature review, photos design and tables: Bakhach E
Data in this study were derived from searches of the PubMed


