Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Alimov I*, Khujanazarov I and Abdusattarov K
Received: June 18, 2018; Published: July 18, 2018
*Corresponding author: Alimov Ijod, Department of Traumatology, Orthopedics, Military field Surgery and Neurosurgery, Tashkent Medical Academy 100109, Tashkent, Uzbekistan
DOI: 10.26717/BJSTR.2018.07.001437
Osteoporosis is the global burden public health issue due to the high prevalence and substantial impact on morbidity and mortality; the incidence rates of osteoporotic fracturesare rise exponentially with an aging population [1]. Untreated osteoporosis can increase the risk of osteoporosis-related fractures. To date, the standard image modality for diagnosis of osteoporosis is a dual-energy x-ray absorptiometry (DXA) scan, the diagnosis for osteoporosis can be done if 2.5 SD below the normal adult mean, also it is scored as a T score [2]. Ballane et al 2017 evaluated the prevalence and incidence of vertebral fractures worldwide using published Medline data. The of this study revealed that the prevalence of vertebral fractures in European women is highest in Scandinavia (26%) and lowest in Eastern Europe (18%), the prevalence rates in North America for White women ≥50 are 20–24%, with a White/Black ratio of 1.6. The rates in women ≥50 years in Latin America are overall lower than Europe and NA (11–19%). In Asia, rates in women above ≥65 are highest in Japan (24%), lowest in Indonesia (9%). Incidence data is less abundant and more heterogeneous. Age-standardized rates in studies combining hospitalized and ambulatory vertebral fractures are highest in South Korea, USA, and Hong Kong and lowest in the UK [3] (Figure 1).
Osteoporotic vertebral compression fractures (OVCFs) are the most common type of osteoporotic fracture; they often occur at the midthoracic (T7-T8) spine and the thoracolumbar junction (T12-L1) [4]. Despite the significant issue of OVCFs to the healthcare system and economy, the issue of treatment of OVCFs is remained challenging throughout the years to date. The conservative management of OVCFs has included the pain relieve medications; limiting activities, back braces, and physical therapy or combination of these procedures [5]. In cases of limited mobility of the patient due to the severity of back pain or ineffective conservative treatment of OVCFs, the alternative can be done to the minimally invasive surgical procedures such as percutaneous vertebroplasty or kyphoplasty, these procedures involve the injection of bone cement polymethylmethacrylate (PMMA) under image guidance into the spinal fractures [6]. In the USA, the total number 81,690 of patients underwent vertebroplasty and 169, 413 patients underwent kyphoplasty between 2006 to 2014 years [7]. The vertebral augmentation treatment modalities such as PVP and KVP may help reduce pain, improve mobility, prevent further collapse of the bone, and also improve the kyphotic deformity.
In our experiences, a total 74 PVP procedures were performed in 41 patients with of OVCFs of the I and II degrees, of them 5 (12%) were male and 36 (88 %) were female; the mean age of the patients was 66 years (range, 55-78 years). The mean duration of the procedure was 51.2 ± 4.2 (range, 34-55) min; the mean cement volume injected into vertebra was 4.5 ± 0.54 (range, 3.4-6.0) ml. The mean follow-up was 16.0 ± 4.2 (range, 12-24) months. All patients achieved substantial pain relief after surgery; the Visual Analogue Scale (VAS) score decreased significantly from a pre-operative value of 8.4 ± 1.2 (95% CI 8.13-8.67), to a post-operative value of 2.0 ± 0.2 (95% CI 2.15- 2.24) and was maintained at 2.2 ± 0.4 (95% CI 2.11- 2.29) at the final follow-up 16.0 ± 4.2 months (p < 0.01).
The intraoperative complication such as a leakage of the cement into the venous plexuses was observed in 2.34 % (1/41) patients, which was the cause of occlusion of small branches of the pulmonary arteries, but the clinical manifestation of this case was asymptomatic. Our previous reported study demonstrated that PVP offers statistically significant short and longterm benefits in decreasing pain and increasing mobility for the patients with OVCFs, there were not any subsequent vertebral fractures in longterm follow-up [5] (Figures 2-4).
Figure 2: Comparison of preoperative and postoperative VAS score in patients with osteoporotic vertebral body fractures of the thoracic and lumbar spine.
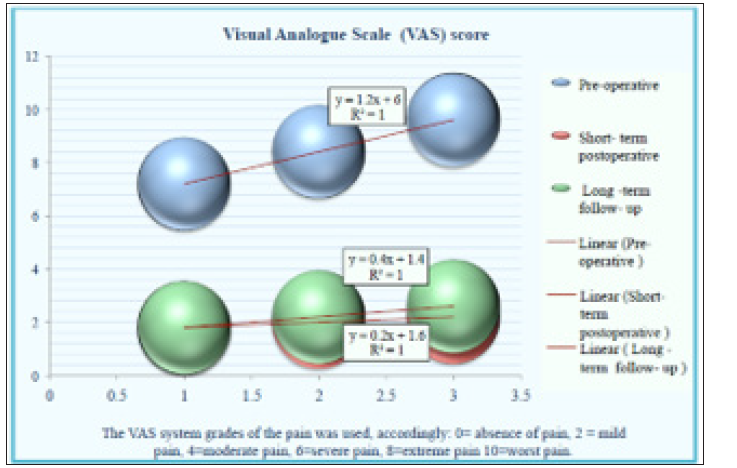
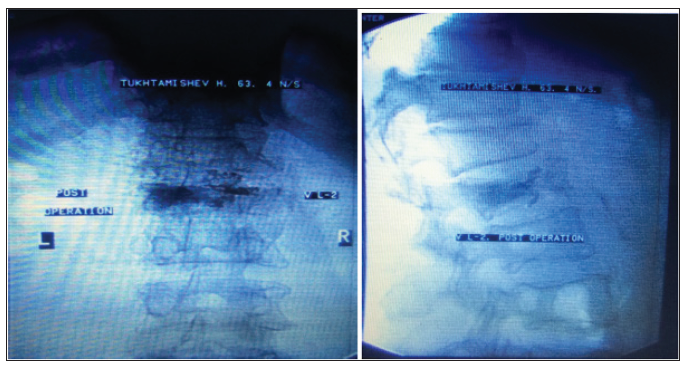
Figure 3: MRI, the T1-weighted sagittal image before surgery. The patient T. was 62 years old. There are signs of low-traumatic compression fracture of the body VL-2, the I degree.

Figure 4: MRI, the T1-weighted frontal and sagittal images after PVP. The patient T. was 62 syears old. The augmentation of the bone cement into the vertebral body of VL-2.
Multiple retrospective and prospective trials demonstrating the efficacy of vertebroplasty or kyphoplasty compared to placebo and standard medical therapy. Pourtaheri et al. 2018 conducted systematic review and meta-analysis to evaluate the clinical outcomes of the treatment of OVCFs with and without vertebral augmentation. The result of analysis 1467 patients demonstrated that the pain reduction was greater with vertebral augmentation modalities over conservative therapy for OVCFs (P<0.000001) in minimum 6-month follow-up [8]. Martikos et al. [9] study compared the long -term clinical and radiographic outcomes in OVCFs of the thoracolumbar spine treated with conservative treatment and percutaneous vertebroplasty. The results demonstrated that PVP provided better vertebral body height restoration, but was associated with a higher incidence of adjacent fractures (20%) than conservative treatment (3.5%). Chandra et al 2018 reported results of analysis of multiple national claim datasets, the results revealed that elderly patients hospitalized for painful VCFs had positive clinical effect following PVP, earlier hospital discharge, lower readmission rates, and reduced mortality [10]. In consummation, the percutaneous vertebral augmentation techniques such as PVP or KVP are safe and effective treatment modality for the patients with OVCFs in combination with the long -term conservative treatment of osteoporosis.


