Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Melinda Fernyhough Culve1, James Bowman2, Vijaya Juturu*1
Received: June 11, 2018; Published: June 19, 2018
*Corresponding author: Vijaya Juturu, Ph.D, FACN, FAND. OmniActive Health Technologies Inc. 67 Park Place Suite 500 Morristown, NJ 07960
DOI: 10.26717/BJSTR.2018.05.001250
Purpose: Excessive exposure to short-wavelength visible (“blue”) light may damage retinal cells and lead to macular degeneration. This study is to assess the effects of macular carotenoids [L/Zi, lutein, zeaxanthin, and meso-zeaxanthin] on visual performance, function, computer use exposure causing symptoms and sleep quality in healthy subjects.
Methods: We carried out a double-blind, placebo-controlled randomized (DBPCR) study in 48 healthy young adults (mean age = 21.2 years, males and females, non- smokers, and Body mass index (BMI) <27 kg/m2). Subjects included in the study was based on minimum at least 4 hours / day (outer side activity & screen time exposure of electronic devices). Subjects were randomly assigned to ingest daily either a placebo (PLA, Safflower oil capsule/day, n = 13), or 20 mg L/Zi (20 mg L/4 mg Zi/day, n = 35). Macular pigment optical density (MPOD), contrast sensitivity (CS), critical flicker fusion (CFF), serum lutein (L) and zeaxanthin (Z) were assessed. Sleep quality assessed and a questionnaire was used to assess the daily use (in hours) of computers/tablet/laptops/smart phones (CDU) and physical symptoms. Statistical significance set at p<0.05.
Results and Conclusion: L/Zi supplementation significantly improved MPOD, CFF and CS [p < 0.05], serum L, Z and ratio of L/Z (p<0.0001) increased over placebo. Sleep quality improved (p<0.05), reduced eye fatigue, eyestrain and headache episodes were observed. Eye fatigue was significantly correlated with CFF and CS at baseline. No adverse events were observed among participants. Visual performance, function, sleep quality and symptoms associated with CDU improved with L/Zi supplementation in healthy subjects.
Keywords: Digital Devices; Blue Light; Photoreceptor Damage; Lutein; Zeaxanthin Isomers; Antioxidants; Oxidative Stress; Sleep Quality; Vision Health Status
Abbrevations: ISRCTN Clinical Trial Registration: ISRCTN16156382; DBPCR: Double-Blind; Placebo-Controlled Randomized; BMI: Body Mass Index; CFF: Critical Flicker Fusion; MPOD: Macular pigment optical density; CS: Contrast Sensitivity; AMD: Age-Related Macular Degeneration; RPE: Retinal Pigment Epithelium; OSDI: Ocular Surface Disease Index; ROS: Reactive Oxygen Species; LED: Light-Emitting Diode; PSQI: Pittsburgh Sleep Quality Index; HPLC: High-Performance Liquid Chromatography; ONL: Outer Nuclear Layer; GRAS: Generally Recognized As Safe
Millions of children and adults use computers at school, work, and home. Extensive viewing of computer screens and an increasing preference for smaller-screen devices that necessitate nearfield viewing (e.g., computers, laptops, tablets and smartphones) can cause eye discomfort, fatigue, blurred vision, and headaches and lead to photo-oxidative damage [1,2]. Based on recent Pew Re search Center surveys, 45% of U.S. adults own a tablet and 73% of U.S. adults own a desktop or laptop computer [3]. Computer use is universal and may lead to significant impact not only on visual comfort and strain but also on occupational productivity [2]. In [3] reported significant differences in median symptom scores with regard to blurred vision during a task (p = 0.03) and the mean symptom score (p = 0.04) was higher for computer use in young, visually-normal subjects [4]. Symptoms such as eyestrain, dry eyes, blurry vision, and eye fatigue are very common from extended computer monitor use [5].
Visible light, such as sunlight, contains all color wavelengths - red, orange, yellow, green and blue – and is colored depending on the energy and wavelength of the spectral bands. According to a study by The Schepens Eye Institute, low macular pigment density may represent a risk factor for Age-related macular degeneration (AMD). Low amounts of macular pigment can result in Inc reased photochemical damage to the photoreceptors and the retinal pigment epithelium (RPE) [6]. In vitro and in vivo studies have shown that too much exposure to blue light damages retinal cells and increases oxidative stress thereby demonstrating that blue light penetrates to the retina [7,8]. Macular carotenoids can be considered for preventing photoreceptor cell degeneration and neutralizing free radicals produced by oxidative stress [7-9]. reported that the retina was most sensitive to short-wavelength light and result to photoxidative damage in the retinal pigment epithelium [10-12]. Computer use and associated symptoms may vary significantly with gender, and a positive correlation was observed between computer-related visual symptoms and the Ocular Surface Disease Index (OSDI), a measure of dry eye [13].
Studies suggest that 60% of people spend more than 6 hours a day in front of a digital device. Blue light is capable of inducing photo-oxidative damage through generation of reactive oxygen species (ROS), and it requires 100 times less energy to cause damage to tissues compared to yellow-orange coloured light (e.g., near 570 - 590 nm) [14]. In the case of light-emitting diode (LED) - based devices [15] long-term, cumulative effects, including cellular damage observed from increased oxidative stress [16]. In 2006 National Sleep Foundation reported insufficient sleep and irregular sleepwake patterns in younger adolescents and in the college student population [17]. Sleep quality was associated with academic progress, leisure activity, and living conditions [18]. The main objective of the study is to determine effects of macular carotenoid levels and 6 months’ supplementation of 20 mg lutein/ 4 mg zeaxanthin isomers on relationships between vision health and overall blue light exposure including sleep, eye strain, blurry vision, neck strain, eye fatigue, and headache episodes in healthy young adults.
This study is a randomized, double-blind, placebo-controlled trial with a 6 month supplementation period. Forty-eight (48) subjects were recruited to visit the Behavioral Neuroscience Laboratory for screening, at baseline, 3 months, and 6 months. Adult male and female college student volunteers enrolled in this study. Subjects requested to avoid carotenoids rich diets including lutein/zeaxanthin isomers rich foods and instructed to follow the dietary restriction list provided during the study period. Subjects requested to fill the diaries/records. After screening, subjects were randomized to placebo or actives [L/Zi] supplementation. Participants were randomly assigned to either macular carotenoid supplement containing 20 mg lutein + 4 mg zeaxanthin isomers (L/Zi), or the placebo group (PLA, safflower oil). This study was reviewed and approved by the University of Georgia Institutional Review Board. Informed consent was obtained for each subject, and the study adhered to the tenets of the Declaration of Helsinki [ISRCTN #16156382].
Potential participants completed a short questionnaire to determine eligibility for the study. Subjects exposed to blue-light exposure / screen time at least 4 hours / day. Also, 2-3 hours of outside activity / day will be recruited with preference, due to blue light exposure. At least one or more of the following computer vision symptoms including digital eyestrain, eye fatigue, blurry vision, difficulty focusing, dry and irritated eyes, headaches and neck and or back pain Participants were in good general health, had corrected visual acuity of 20/20 or better, not taking medication that may interfere with sleep patterns, subjects were also screened to ensure viewing screens at a distance of 3 feet or less, and had no current or previous history of ocular pathology. Subjects wearing spectacles for vision correction were not considered for the study, due primarily to potential reflection and coating-mediated light absorption issues with glare testing. Subjects were instructed to maintain their current diet; those that were planning on changing their diet (for whatever reason) were excluded from consideration for the trial.
Those with a Body Mass Index of 28 or greater were excluded, because the supplemental lutein may be deposited preferentially in adipose tissue, and not in the retina. Due to the potential for saturation, those with a macular pigment optical density (MPOD) of 0.70 or higher were excluded. Subjects were excluded if they had a history of ocular disease or insufficient visual acuity. Visual acuity of 20/30 best corrected was cutoff for exclusion. Subjects with systemic disease or any disease state (e.g. diabetes), and current smokers were excluded. Individuals taking psychiatric medication and any medication to treat a psychiatric condition (e.g. obsessive-compulsive disorder, depression, bipolar disease and schizophrenia) were excluded. Measures of all visual and physical parameters (detailed below) were taken at baseline, 3 months and 6 months.
Subjects were randomly assigned to either placebo (n = 13) or MC supplement (n = 35) groups. Pills for each group were identical, brown-colored, soft gelatin capsules. Placebos (PLA) contained no lutein (L), zeaxanthin (Z), or meso-zeaxanthin (MZ), but only safflower oil. Independent analysis indicated that the active supplement pills (Lutemax 2020®) contained 20 mg of L, and 4 mg Zi (RR and RS-zeaxanthin), obtained from the extract of dried flowers of Marigold (Tagetes Species)] supplied by OmniActive Health Technologies Ltd., India. Subjects were instructed to ingest one pill with a meal (preferably lunch or dinner) every day. Compliance was ensured with weekly phone calls and pill counts.
a) Measurement of Macular Pigment Optical Density (MPOD)
A macular densitometer (Macular Metrics, Inc., Rehoboth, MA, USA) was employed. The apparatus and procedure used to measure macular pigment optical density (MPOD) have also been described in detail previously described by Stringham et al. [19].
b) Temporal vision (Critical flicker fusion frequency, CFF)
CFF was assessed as per the method described by Renzi and Hammond [20]. The overall threshold for the CFF task was calculated as the average of two ascending and two descending thresholds.
c) Contrast sensitivity testing
The procedure used to measure macular pigment optical density (MPOD) have also been described in detail previously described by Stringham et al. [21]. The subjects typically produced five or more reversals; actual thresholds were determined by computing the average of the last three reversals. Two thresholds were determined at each visit; the average of the two thresholds was taken as the true threshold,and used for statistical analysis.
d) Sleep
The sleep quality of participants was assessed by Pittsburgh Sleep Quality Index (PSQI) [22]. The PSQI is a self-rated questionnaire which measures subjective sleep quality and disturbances over the past month, and differentiates between normal and poor sleepers. In this questionnaire, 19 questions are grouped into 7 components, each having score range from 0 (no difficulty in sleep) to 3 (severe difficulty). The global PSQI score was calculated and score >5 was considered as disturbed or poor sleep [22].
e) Computer devices use questionnaire
A short questionnaire, containing questions about weekly occurrence of headache, eye strain, neck strain, eye fatigue, and blurry vision was administered at each visit. If a specific item occurred less often than once / week, but still occurred on a monthly basis (e.g. twice / month), participants were instructed to write down the monthly frequency next to the item. For calculation purposes, a month was considered four weeks; monthly frequency was simply divided by four to yield a weekly value. During each visit, participants completed a short questionnaire about the weekly frequency of occurrence of five outcome variables typically associated with excessive near-field device use: headache, blurry vision, neck strain, eye strain, and eye fatigue.
f) Serum Lutein and Zeaxanthin Assay
Serum samples analyzed for lutein and zeaxanthin levels using High-Performance Liquid Chromatography (HPLC).
g) Statistical analysis
The primary analyses were conducted according to intent-totreat principles. The statistical power rate 1−β was set at 0.80; a 20% change in visual performance or physical indicator status in treatment groups, a standard deviation of 20%, and α = 0.05 were parameters used for calculation. With the placebo group set at n = 12, the power calculation determined that the treatment group required 30 subjects to detect effects (if present). Randomization was computer generated in a 3:1 ratio. For each attribute (vision markers such as MPOD, CS and CFF, PSQUI, headache, strain, fatigue, blurry and irritated), the pre/ post differences were compared within the treatment groups using a two-sided, two-sample Student’s t-test. The pre/post differences were compared between the treatment groups using analysis of variance. The attributes were correlated utilizing Pearson Correlation Coefficients. All statistical tests of hypothesis employed a level of significance of 0.05 and no adjustments were made for the number of tests performed. Analysis was performed using SAS (SAS Institute, Cary, NC).
Subject characteristics and use of electronic devices such as computers, smart phones and television were reported in Table 1. There were no significant differences between treatments for mean computer use time, or any other baseline characteristics. This study was conducted in U.S Population. Study includes males and females.
L/Zi supplementation increased MPOD, improved CFF and CS at 3 months and 6 months (p<0.001). No significant changes were observed in placebo (PLA) group. Significant difference in vision performance/function markers were observed between the treatments (p<0.001), (Table 2). No significant difference was observed between the treatments at baseline for MPOD (p value: <0.96250), CFF (p value: <0.82960) and CS (p value: <0.1036).
Serum lutein (p<0.0001), serum zeaxanthin (p<0.0001), ratio of L/Z (, p<0.0001) significantly increased over placebo at 6 months. Significant decrease in lutein levels were observed in placebo (Table 2).
*Asterisks denote statistically significant difference from baseline (p ≤ 0.05)
**Asterisks denote statistically significant difference from Placebo (p ≤ 0.05)
vSerum lutein (p<0.0001), serum zeaxanthin (p<0.0001), ratio of L/Z (, p<0.0001) significantly increased over placebo at 6 months. Significant decrease in lutein levels were observed in placebo (Table 2).
Sleep quality (PSQI) was improved at 3 months (18.1%) and 6 months (19.9%) in treatment group subjects, versus placebo (p<0.05) (Tables 3 & 4) provides the results of the PSQI and its respective domains before and after supplementation. Sleep disturbance significantly decreased in L/Zi group relative to baseline at 6 months (p<0.0435). In this study, sleep latency (time needed to fall asleep) was decreased in L/Zi group (p<0.0389) at 3 months. Daytime dysfunction decreased in L/Zi (p<0.0090 at 3 months and p<0.0381 at 6 months). Sleep efficiency increased significantly in the L/Zi supplementation group (p<0.0508). The need of medications to sleep decreased in L/Zi (p<0.0316) supplementation. No significant changes were observed in placebo.
Table 3: Averages and standard deviations of the Pittsburgh Sleep Quality Index and its respective domains.
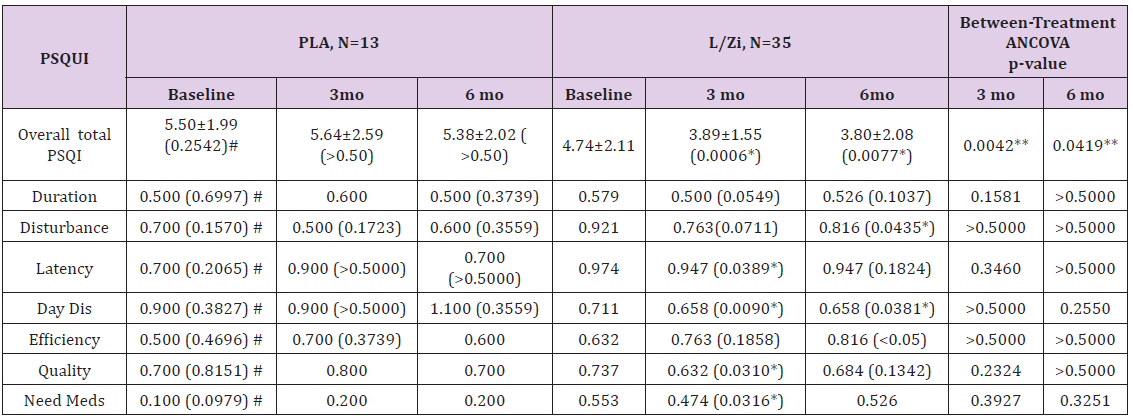
A total score of “5” or greater is indicative of poor sleep quality
# No significance between the treatments at baseline (PLA and L/Zi)
*Asterisks denote statistically significant difference from baseline (p ≤ 0.05)
**Asterisks denote statistically significant difference from Placebo (p ≤ 0.05)
*Asterisks denote statistically significant difference from baseline (p ≤ 0.05)
**Asterisks denote statistically significant difference from placebo (p ≤ 0.05)
# No significance between the treatments at baseline (PLA and L/Zi)
Compared with baseline, eye fatigue was reduced significantly after supplementation at 3 months (p<0.0007) and 6 months (p<0.0001) compared with baseline. Eyestrain significantly decreased after L/Zi supplementation at 3 months (p<0.0475) and 6 months (p<0.0319) in L/Zi group. No significant changes were observed in PLA group. Headache episodes significantly reduced in L/Zi treated group after supplementation (p<0.0001 over baseline; p<0.0032 at 6 months over placebo). Eye fatigue was significantly correlated with CFF (r=0.2791, p<0.054) and CS (r=0.34941, p<0.05).
Long-term exposure to blue light has the potential to induce damage to the retina and photoreceptor damage and many physiologic functions [11-13,16,17]. The results of our study suggest primarily to visual performance and parameters of physical comfort that are impacted by extended use of CDU. Geiger et al (2015) reported wild type mice and R91W; Nrl (-/-) model exposed to toxic levels of blue light and analyzed their retinas at different time points post illumination (up to 10 days). Massive pyknosis in a focal region of the outer nuclear layer (ONL) was observed in wild type mice and cell death detected within the inner nuclear layer. Microglia/ macrophage infiltration at the site of injury was more pronounced in the all-cone retina was observed in R91W; Nrl (-/-). In addition, vascular leakage was abundant in the inner and outer retina, retinal swelling and the appearance of cystoid spaces in both inner and ONLs was also observed in R91W; Nrl (-/-) mice [23]. Blue light has been known to be phototoxic for the retina. Macular edema in humans is a result of diffuse capillary leakage and micro-aneurysms in the macular region.
Macular carotenoids may thus potentially help to develop treatment strategies for complications in macular degenerations. In this study, at the monthly visits, compliance was monitored with specific questions on the subject’s daily intake of the intervention foods and a review of compliance calendars. Subjects requested to fill the diaries/records to observe if there are any changes in their dietary habits. Our study showed that by increasing MPOD an improvement in visual performance and symptoms such as eye strain and eye fatigue was reduced. Perhaps more importantly, increasing MPOD leads to improved visual performance [24]. In the current study, L/ Zi supplementation [all p < 0.05] improved visual performance at 3 months and 6 months, respectively. In this study, subjects significantly improved contrast sensitivity in L/Zi treated group. These results suggest a significant improvement in visual performance was observed at 3 months and continued at 6 months. In consideration of vision testing (inclusion criteria), all subjects had uncorrected or contact lens-corrected visual acuity of 20/20 or better in the test (right) eye, and had no current or previous history of ocular pathology.
Subjects wearing spectacles for vision correction were not considered for the study, due primarily to potential reflection and coating- mediated light absorption issues with glare testing. Current limitations of the study include the facts that light has a cumulative effect and many different characteristics such as wavelength, intensity, duration of the exposure, distance from the electronic device, and time of day are important to consider the spectral output of the light source to minimize the danger that may be associated with blue light exposure. In this study the observation, together with the limited data in terms of length of treatment, may help to predict the association between blue light exposure as a source from electronic device and its effect on visual performance. Further longterm studies are required to explore light exposure level, wave lengths and light protection for computer devices to protect vision. Exposure to near-field screens, although not often not acutely or superficially noticeable, creates glare, reduces visual contrast, can affect visual acuity, and causes general eye strain, headaches and fatigue [25,26]. In our present study, we observed L/Zi supplementation reduced eye fatigue and eyestrain over baseline, and reduced headache episodes. Eye strain, headache and eye fatigue are common symptoms experienced in relation to the use of computers.
We did not measured skin color during the period of the study. In our previous study, we reported improved overall skin tone, luminance (L*) values and individual typological angle increased in the L/Zi group. Mean minimal erythemal dose was increased with L/Zi supplementation after 12 weeks of supplementation [27]. In addition L/Zi (Lutemax 2020 ) supplement has obtained Generally Recognized as Safe (GRAS) status and in 2011 notified to food and drug administration (FDA). This is based on standard set of toxicity studies recommended by FDA including published and unpublished human clinical trials [28]. In terms of sleep quality, Galambos and colleagues [29] showed that less sleep predicted greater negative mood while better quality sleep increased positive mood and decreased stress. Poor sleep and daytime sleepiness was negatively affect academic performance [30,31] and driving skill [32] and shorter sleep was associated with increased incidence of common illness in adolescents [33] and adults [34]. Sleep disturbances may reduce performance, increased morbidity, fluctuation in mood, risk of accidents, and reduced life expectancy [35,36]. Sleep apnea was associated with cardiovascular, inflammatory and metabolic consequences [37].
In the current study, we observed a sleep quality total score (PSQI) improvement at 3 months (18.1%) and 6 months (19.9%) in the L/Zi-treatment group, versus placebo (p<0.05). We did not observed correlations of sleep and visual performance. Further studies are required to study in people with low PSQUI and in relation to melatonin and vision performance. Our study results suggest that a benign, nutritional mode of therapy can have a significant impact on sleep quality-perhaps most notably in those with high exposure to near-field screens. Recent studies reported night time phone use and texting markedly decreased the quality, duration, and efficiency of sleep [38,39], poor sleeping pattern in medical students [40] and poor sleep quality among college students [41,42]. The results of our study, conducted on college students, are therefore encouraging. In terms of benefits to the retina, lutein and zeaxanthin have been shown to promote the differentiation of photoreceptors, increase expression of opsin, and increase in development of outer-segment like apical processes, and modulate development of new cellular structures [42].
L/Zi treatment effect is probably related to the decrease in oxidative stress and endoplasmic reticulum stress by the L/Zi treatment [7,8]. The limitations of the study include subjects were not recruited based on poor sleep quality and not measured hours of computer use before bed time. The longer-term health impacts of poor sleep quality was of increase interest, as evidence suggests that there are rising levels of sleep disturbance due to digital devices. The number of domains of sleep quality measured in sleep research was influenced by the type and scope of the study being conducted. The results of these studies were constrained by limitations in measurement of sleep quality. These findings were of interest to researchers on how macular carotenoids can alter changes vision performance and in their sleep quality and changes in computer use symptoms with supplementation.
We are grateful to all participants in the study for the consent and co- operation in the study. We thank all our staff for helping blood analysis and collection. The authors would like to thank OmniActive Health Technologies Ltd. for providing macular carotenoid capsules and matched placebos including study support and funding.


