Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Nasir A M AL Jurayyan*
Received: June 10, 2018; Published: June 19, 2018
*Corresponding author: Nasir A M Al Jurayyan, Professor and Consultant Pediatric, Endocrinologist, Division of Endocrinology, Department of Pediatrics (39), College of Medicine, P.O Box 2925, Riyadh 11461, Saudi Arabia
DOI: 10.26717/BJSTR.2018.05.001245
Pituitary apoplexy in children is extremely rare clinical syndrome, and potentially lethal due to adrenocorticotrophic hormone (ACTH) deficiency. It is characterized by acute haemorrhagic or infraction of the pituitary gland. We report a 13 year-old-boy who presented with acute headache, vomiting, and visual loss. He was diagnosed to have macroprolactinoma, with acute haemorrhage into the mass by magnetic resorance image (MRI), and raised serum prolactin. Serum ACTH, cortisol, thyroid stimulating hormone (TSH), and free thyroxine (FT4) were low. This report aims to remind the general practitioners and the emergency practitioners of the initial assessment and management of pituitary apoplexy.
Keywords: Macroprolactinoma, Pituitary, Apoplexy, Management, Diagnosis
Abbrevations: ACTH: Adrenocorticotrophic hormone, MRI: Magnetic Resorance Image, TSH : Thyroid Stimulating Hormone, FT4: Free thyroxine, PRL: High prolactin, LH: luteinizing hormone, FSH: Follicular Stimulation Hormone
Pituitary apoplexy is children is extremely rare clinical syndrome secondary to abrupt hemorrhage or infarction, complicates ≃2% of pituitary adenomas, especially nonfunctioning tumors [1-4]. Headache of sudden and severe onset is the main symptom, sometimes associated with visual disturbances or ocular palsy. Signs of meningeal irritation or altered consciousness may complicate the diagnosis [5]. Precipitating factors (increase in intracranial pressure, arterial hypertension, major surgery, anticoagulant therapy or dynamic testing, etc) may be identified [6-9]. Corticotropic deficiency with adrenal insufficiency may be life threatening if left untreated [5]. Magnetic resonance imaging confirms the diagnosis by revealing a pituitary tumor with hemorrhagic and/or necrotic components [10,11]. Here in we report a case of pituitary apoplexy who present with acute headache, visual loss and vomiting. Short literature review is also included.
A 13-year-old male patient presented with acute history of headache, visual loss, and vomiting following a one-year history of intermittent frontal headache and blurred vision. Past medical and family history were unremarkable, and he was not on any medication. Vital signs showed blood pressure 118/65 mmHg, heart rate 74/min, temperature 36.8C, anthropometric measurements were height: 164.5 cm (above 50 centile) weight 85.4kg (above 95 cen tile). Pubic hair at tanner stage 4, testicular volume was 12 ml bilaterally. Funduscopy showed normal examination of the right eye while there was a pale optic disc of the left eye. Visual field examination revealed total loss of left eye vision, while there was temporal hemianopia of the right. Laboratory investigations revealed high prolactin (PRL) level of 17532ng/ml, thyroid stimulation hormone (TSH) 0.9 mu/L and free thyroxin (FT4) 10.9 pmol/L (indicating secondary hypothyroidism). Adrenocorticotrophic hormone (ACTH) 0.3 pmol/L, cortisol 9.9 nmol/L (indicating central adrenal insufficiency), luteinizing hormone (LH) 1.1IU/L, follicular stimulation hormone (FSH) 2.5 IU/l, and testosterone 6.3 nmol/L.
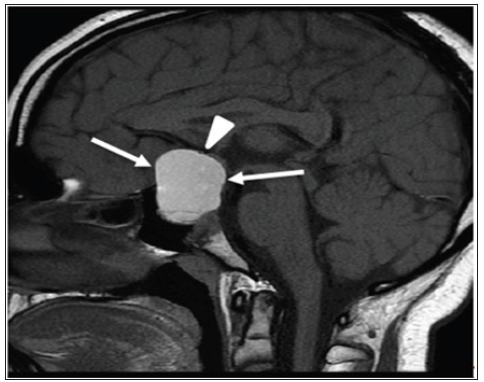
Liver and renal function were normal with serum glucose 4.4mmol/l. Serum sodium 137mmol/l with normal serum osmolality. There was no evidence of diabetes insipidus or SIADH before or after surgery. A magnetic resonance imaging (MRI) revealed a large interstellar mass with suprasellar extension with evidence of recent hemorrhage within the mass (Figure 1), measuring 4 x 2.5 x 3cm. Due to visual symptoms and under steroid coverage, transsphenoidal hypophysectomy was performed and revealed pituitary adenoma – prolactinoma type. The patient was started on dopamine agonist (Cabergoline). Hydrocortisone and Levothyroxine were continued.
Figure 1: Mid-sagittal brain MRI (T1 weighted image without intravenous contrast: shows a largeintrasellar/suprasellar mass (arrows) with homogenous high signal intensity indicatinghemorrhage.
The diagnosis of macroprolactinoma in this patient was established on the bases of high serum prolactin, the MRI findings, histopathology, white, pituitary apoplexy was explained on the bases of acute symptoms, MRI findings of blood within the gland, and hormonal deficiency [12,14]. Pituitary apoplexy in children is extremely rare, but could be life threatening due to ACTH deficiency [15-17]. Symptoms typically associated with pituitary apoplexy include sudden severe headache, visual field defects, decrease visual acuity, and ophthalamoaplegia. Other symptoms are nausea, vomiting, vertigo, and meningeal irritation [5,18,19]. All tumors have a similar risk of apoplexy, and the incidence has been established at ≃2%. Approximately 50-80% of cases of apoplexy occur in patients who were unaware of the presence of tumor. Various precipitating factors have been described in the literature including, hypertension, diabetic ketoacidosis, and coagulation agents [1-4,6-9,20,21].
Diagnosis of pituitary apoplexy must not be over looked. The most reliable method to diagnosis pituitary apoplexy in MRI [10,11,22]. Management should be made by multidisciplinary team of experts in neurosurgery, endocrinology, and ophthalmology. Optimal management of acute apoplexy remains controversial. Some authors advocate early transphenoidal surgical decompression for all patients, whereas others adopt a conservative approach for selected patients, namely those without visual acuity or field defects and with normal consciousness. The size of the tumor on MRI is also an important part of the clinical decision-making process. If conservative treatment is chosen, then careful monitoring of visual signs and symptoms is necessary, and surgical decompression is recommended if visual disorders do not improve or if they deteriorate. However, clinical deterioration can be rapid, and patients may not be able to be hospitalized for observation which may limit this approach. Reevaluation of pituitary function and the tumor mass in the months after the acute apoplectic episode is mandatory to determine whether the pituitary defect is permanent, to determine the possible hypersecretory nature of the adenoma, and to initiate follow-up of a possible tumor remnant [23-28].
The author would like to thank Ms. HADEEL N ALJURAYYAN for his help in preparing the manuscript.


