Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Ahmad Oryan1,2, Somayeh Monazzah2 and Amin Bigham-Sadegh*3
Received: April 04, 2018; Published: June 14, 2018
*Corresponding author: Amin Bigham-Sadegh, DVM, DVSc, Department of Clinical Sciences, School of Veterinary Medicine, Shahrekord University, Shahrekord, Iran
DOI: 10.26717/BJSTR.2018.05.001228
The main reason of postmenopausal osteoporosis is high bone turnover due to increased osteoclastic action. Strontium Ranelate is a new drug that is used for the treatment of postmenopausal osteoporosis. We searched PubMed in May 2016 using the terms ‘Strontium ranelate’ for experimental study and review articles. The result from the studies that we have conciliated show: Strontium ranelate enhances bone resistance and increases the bone formation. Strontium ranelate has been shown to increase bone apposition rates and bone mineral density while maintaining the quality of bone mineral; but it has no effect on mineralization. Evidence from in vitro and in vitro studies present the evidence that strontium ranelate is able to inhibit the osteoclasts resorbing activity, decreased osteoclastic differentiation (Prevention of differentiation of blood monocyte and pre-osteoclasts into osteoclasts) and increase apoptosis of osteoclasts. The studies show that strontium ranelate increased pre-osteoblastic replication and osteoblastic proliferation and differentiation as evaluated by the measurement of DNA synthesis in osteoblasts.
Strontium ranelate stimulated the synthesis of PG by human chondrocytes. Strontium ranelate promotes the synthesis of PG capable of integrating the ECM. It has been show that post fracture use of strontium ranelate on the ovariectomized rats is associated with better fracture healing as assessed by radiography, histological analysis and biomechanical testing. The exact mechanism by which strontium ranelate exerts these effects is not definitely understood, but may include inhibition of osteoclast formation and stimulation of osteoblast proliferation. In most cases use of strontium ranelate did not seem to be associated with series adverse events and most adverse events were mild and transient. It seems that Strontium ranelate is aeffective and winsome treatment for osteoporosis and in the most cases the side effect of this drug is negligible.
Abbrevations: SOTI: Spinal Osteoporosis Therapeutic Intervention, TROPOS: Treatment of Peripheral Osteoporosis, STRATOS: Strontium Ranelate for Treatment of Osteoporosis, PREVOS: Prevention of Osteoporosis
The main reason of postmenopausal osteoporosis is high bone turnover due to increased osteoclastic action) [1]. Strontium Ranelate is a new drug that is used for the treatment of postmenopausal osteoporosis [2]. It is used for decreasing the risk of fracture in vertebral and non-vertebral (especially hip) bones [3]. Strontium ranelate is a combination of strontium chloride (SrCl2, 6H2O) and sodium ranelate [4]. Strontium ranelate contains two stable atoms, strontium and one organic carrier, ranelic acid [5]. The molecular action mechanism of strontium ranelate is not understood [4]. But its action mechanism on bone is complex and time-dependent and dose- dependent [6]. It has been seen that the low doses of strontium ranelate persuaded the bone tissue quality [7]. It enhances bone tissue quality, and is effective on bone resistance and reduces the fracture risk in postmenopausal osteoporotic patients which treated with strontium ranelate [8].
Strontium ranelate also prevents bone loss that is induced by estrogen deficiency in postmenopausal women by restraint of bone resorption and stimulation of bone formation [9]. In ovariectomized rats, Strontium ranelate prevented bone resorption, whereas bone formation remained elevated [10]. This drug is well tolerated because it has no effect on food intake or body weight [11]. Strontium ranelate has some similarities with Ca+2 in its absorption in the digestive system, incorporation into bone, and reabsorption in the kidneys [12]. Because strontium, a divalent cation like Ca+2, it’s possible that the ralenate salt plays a role in the incident of this reaction [13]. Administration of 2 g/day of strontium ranelate to postmenopausal women for a 2-year resulted in uncoupling between bone resorption and bone formation that led to a significant increase in the lumbar spine bone density and a 44% reduction in vertebral fracture during the 2end year of treatment [14]. The strontium ranelate effects on bone can be studied by histomorphometry, DXA, and biomechanics in preclinical studies [15]. Originally strontium was detected in the 1700, in Scotland, a place near Strontian [16]. This earth element is present in food and water and throughout the bones [17]. Strontium ranelate was used widely in the 1950 for the treatment of malignant bone diseases, osteoporosis, painful, etc. [18].
We searched PubMed in May 2016 using the terms ‘Strontium ranelate’ for experimental study and review articles. Of the 61 articles retrieved, there were 5 review articles. Evidence of the safety and efficacy of strontium ranelate comes from two large multinational clinical trials, the Spinal Osteoporosis Therapeutic Intervention (SOTI), [5] and Treatment of Peripheral Osteoporosis (TROPOS), [19] studies, which were designed to study vertebral and non vertebral fractures respectively; and clinical data is available from 2 earlier Phase 2 trials, the Strontium Ranelate for Treatment of Osteoporosis (STRATOS), Meunier et al. and Prevention of Osteoporosis (PREVOS), [18] studies.
Strontium ranelate cause a positive bone balance in experimental models [13]. It has a unique effect on bone remodeling by increasing bone formation and decreasing bone resorption, which leads to prevention of bone loss and increase in bone mass and strength [20]. It increases markers of bone formation and also has anabolic effects on bone [21]. The analysis of bone markers showed that strontium ranelate reduced the excretion of the bone resorption marker from kidney and increased the levels of osteoblast differentiation serum marker, bone-specific alkaline phosphatase [22]. Strontium ranelate enhances bone resistance and increases the bone formation, as evaluated by increased ALP activity, and it is confirmed by the increased trabecular and cortical bone tissue amount [23].
Strontium ranelate has been shown to increase bone apposition rates and bone mineral density while maintaining the quality of bone mineral [24]; but it has no effect on mineralization [25]. Actually some studies on intact animals confirm that strontium ranelate preserves the structure of bone matrix crystals without affecting the mineralization process [26]. It has been shown that treatment with strontium ranelate results in the formation of lamellar bone with no evidence of mineralization defect or other deleterious effects [27].
a) It has shown strontium ranelate increase the diameter of the bone shaft suggesting an effect on periosteal bone formation [28]. It also increases trabecular bone volume, trabecular number, trabecular thickness, and cortical thickness Arlot et al. Modification of bone diameters with periosteal apposition may effects bone strength of long bones [29]. This effect on bone size is very important and can play a role in the improvementof mechanical properties of bone, because the diameter of long bones predicts to 55% of the variance of the bone strength (Arlot et al 2008). Strontium ranelate treatment seems to stimulate both trabecular and cortical bone formation in 3D analyses but without increase of cortical porosity [30]. The change in 3D trabecular and cortical micro architecture improve bone biomechanical properties Arlot et al.
b) Evidence from in vitro and in vitro studies present the evidence that strontium ranelate is able to inhibit the osteoclasts resorbing activity [31], decreased osteoclastic differentiation (Prevention of differentiation of blood monocyte and pre-osteoclasts into osteoclasts) and increase apoptosis of osteoclasts [5]. Strontium ranelate inhibited the expression of two osteoclast markers: the αv subunit of the vitronectin receptor and carbonic anhydrase-II in bone marrow culture [32].
c) The studies show that strontium ranelate increased pre-osteoblastic replication and osteoblastic proliferation and differentiation as evaluated by the measurement of DNA synthesis in osteoblasts [9]. It stimulates osteoblastic differentiation markers activity such as ALP, bone sialoprotein and osteocalcin in osteoblasts [16]. Strontium ranelate promote osteoblasts survival [33] and its positive effects on osteoblast survival, is because of the seven-transmembrane-spanning extracellular calcium-sensing receptor which is expressed by osteoblasts and that responds to strontium [34]. However, recently it has been showed which Strontium ranelate increases osteoblasts survival independently of the calcium-sensing receptor, indicate that other signaling mechanisms may involve in the positive effects of Strontium ranelate on osteoblastogenesis [35].
d) Some in vitro Studies in human osteoblasts suggest that strontium ranelate have the ability to promote the differentiation and survival of osteocytes, which is an additional mechanism of its anti-fracture efficacy [10].
e) Strontium ranelate has beneficial effects on both cartilage and bone remodeling Henrotin et al. It has shown evidence of beneficial effects of strontium ranelate on interference in cartilage metabolism [36]. It stimulates cartilage matrix formation by ionic stimulation of chondrocyte anabolism without affecting resorption of cartilage; it enhanced collagen synthesis and has a direct effect on proteoglycan synthesis [37]. It could restore the imbalance between chondroresorption and chondroformation observed.
f) Strontium ranelate stimulated the synthesis of PG by human chondrocytes [38]. Strontiumranelate promotes the synthesis of PG capable of integrating the ECM [39]. It also promoted the synthesis of high-molecular weight PG complexes [40]. The mechanism that strontium ranelate influenced the synthesis of PG is not known until now Henrotin et al. Strontium is effective in reversing the IGF-Istimulating effect, because factors which lead to increase the synthesis of PG were reported as causing an initial decrease in cytosolic free Ca concentration [41]. IGF-I stimulation of PG synthesis maybe increased by strontium ranelate treatment [42]. This effect may be consequent to the proliferation of chondrocyte because IGF-I is required for cell proliferation [43]. This fact that IGF-I regulates the metabolism of chondrocyte (by IGF-I produced in response to a high of strontium) can be responsible for the PG increase [44]. Furthermore high extra cellular Ca concentration increases the secretion of IGF-I as well as the expression of IGF-I mRNA by osteoblastic MC3T3-E1 cells [45]. This finding can explain why strontium ranelate increased the IGF-I effect when it was added to a low concentration [36].
Fracture Healing: Although antifracture efficacy of strontium ranelate has been demonstrated, there is paucity of data on the effect of strontium ranelate on fracture healing [4] and there are limited data about the effect of strontium ranelate on fracture healing Seeman et al. It has been show that post fracture use of strontium ranelate on the ovariectomized rats is associated with better fracture healing as assessed by radiography, histological analysis and biomechanical testing Seeman et al. Some of scientists evaluated the efficacy of strontium ranelate on fracture healing in healthy bone Roux et al. In these studies employing traumatically induced fracture, no effect on fracture healing were reported Arlot et al. & but Li et al. reported that 625 mg/kg/day strontium ranelate revealed beneficial effect on the fracture healing on the ovariectomized rats [24]. The weaker antiresorptive activity of strontium ranelatecan not disrupts the osteoclast resorption in the remodeling phase [19]. Anabolic activity of strontium ranelate can provide beneficial effect on the regenerative and reparative processes of the remodeling phase in the fracture healing (Roux et al 2016). Further studies are needed to discover the precise mechanism of action of strontium ranelate on fracture healing [19] (Table 1).
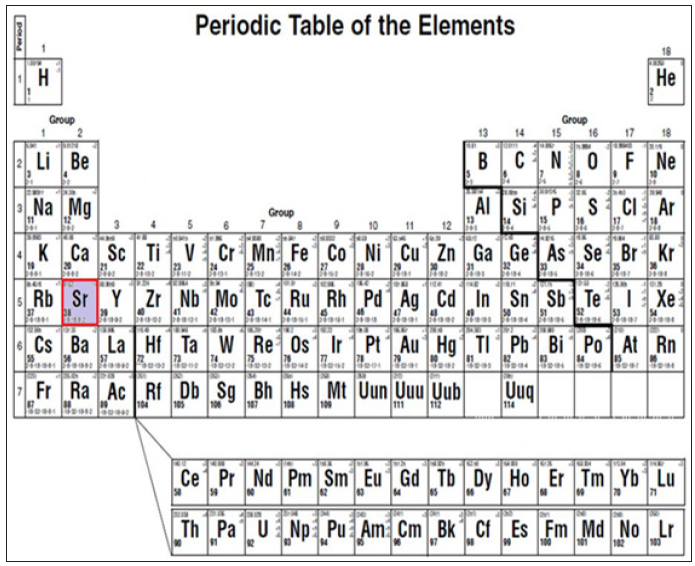
The exact mechanism by which strontium ranelate exerts these effects is not definitely understood, but may include inhibition of osteoclast formation and stimulation of osteoblast proliferation [46]. Strontium ranelate has the atomic number 38 and the atomic symbol Sr, belongs to the group II in the periodic table of the elements, just beneath Ca+2 (Figures 1 & 2). As its nucleus is similar to that of Ca+2, the body takes up strontium into tooth enamel and bones in the place of Ca+2. In addition Strontium ranelate stimulates the Ca+2 sensing receptors [47]. Strontium ranelate regulates protein and mRNA levels of the osteoblast which induced signals for osteoclastogenesis [48]. These findings provide new insights to the action mechanism of strontium ranelate in the bone microenvironment [49].
Figure 2: Strontium ranelate has the atomic number 38 and the atomic symbol Sr, belongs to the group II in the periodic table of the elements.
The cellular mechanism which strontium ranelate may act is unknown, although the inductions of activation of the Ca+2-sensing receptor and cellular differentiation have been suggested as contributing factors [50]. Previously was shown strontium suppressing the release of parathyroid hormone [51]; but recently, it has been shown to activate the Ca+2-sensing receptor in other cell systems. Whether the Ca+2-sensing receptor also mediates some of the effects of strontium ranelate on bone, as it reportedly does for Ca+2, remains to be determined [52]. The fact that strontium ranelate contained in bone is eliminated in the end of treatment; it is strongly suggests which strontium ranelate was not trapped in hydroxyapatite [53]. So, in the bone mineral phase, strontium ranelate is located in the hydrated layer and can structurally modify the bone matrix in relation to the hydration state of the bony tissue (Figures 1 & 2).
We collected information about the risks of adverse events with the use of strontium ranelate for the treatment of postmenopausal osteoporosis [54]. In most cases of strontium ranelate did not seem to be associated with series adverse events and most adverse events were mild and transient [55]. Also the most of subsequent publications generated from the strontium clinical trials programme failed to report data on these adverse events [22]. However, it has been reported which there is a higher rate of cardiac events (myocardial infarction) in men with to strontium ranelate therapy. The 2013 Periodic Safety Update Report showed that strontium increased the risk of myocardial infarction in pooled analyses in postmenopausal women [56]. The risk of two serious adverse event, venous thromboembolism and pulmonary embolism was found to be significantly higher in patients with strontium ranelate therapy [5].
Some nervous system disorders, including disturbed consciousness, seizures, mental impairment, and memory loss and were reported with the use of strontium ranelate [57]. Strontium ranelateis associated with a number of other risks, such as serious disturbances in consciousness, liver inflammation, seizures, gastrointestinal disturbance, reduced number of blood cells, severe skin reactions such as Stevens–Johnson syndrome, toxic-epidermal necrosis, and drug rash with eosinophilia and systemic symptoms [58]. In the cases that we should not use strontium ranelate like stroke and ischemic cardiac events we can use efficacious drugs such as alendronate, risedronate, zoledronate, or denosumab [18]. Strontium ranelate acts through an innovative mode of action by inhibiting bone resorption and stimulating bone formation [59]. Strontium ranelate is a new drug for the treatment of postmenopausal osteoporosis and its safety profile is not fully established [60]. Strontium ranelate has been associated with adverse events and idiosyncratic reactions [61]. Strontiumranelate has been studied in many studies for a longer duration. So, it’s pre-marketing safety data are relatively robust [49].
It seems that Strontium ranelate is aeffective and winsome treatment for osteoporosis and in the most cases the side effect of this drug is negligible.


