Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
S Dhoum1*, K Jabrane2, S Dhaimy3, N Talache4, K Lahlou5, A El Ouazzani6 and H El Merini7
Received: May 22, 2018; Published: May 31, 2018
*Corresponding author: S Dhoum, Specialist, department of conservative dentistry and endodontics, School of dentistry of Casablanca, North Africa
DOI: 10.26717/BJSTR.2018.05.001147
The use of composite for posterior teeth restoration competes with amalgams, metallic and ceramic inlays, in the important deterioration cases. Its use is increasing and it’s becoming possible because of the current progress of composite material technology and bonding evolution. Even though the dentists seem informed and able to achieve successfully the direct composite technique, the use of composite restoration with indirect or extra-oral method remains uncertain. In this article, we will explore composite systems used at the laboratory for indirect restoration and we will treat, step by step, the composite inlay realization.
Keywords: Posterior Restoration; Laboratory Composite; Composite Inlay; Indirect Technique
In restorative dentistry, metallic inlays, and especially gold were considered as filling the choice of posterior teeth. However, the growing demand for aesthetic fillings by patients, reproducing the natural appearance of healthy teeth has guided research towards material improvement and new perspectives. The advent of bonding systems and the use of the etching capabilities of enamel and dentine have considerably modified the therapeutic concept of posterior dental lesions. Touati in France 1983 and James in USA 1983, were the first to propose the first to offer moulded composite incrustations, made from an impression, and secondarily bonded in the mouth [1,2]. These incrustations are what everyone agrees to name: composite inlays. Composite Onlay/Inlays turn out to be an interesting restoration option among other possible choices in our therapeutic arsenal. Indeed, they combine with their natural aesthetic and ecological qualities, favourable mechanical and biological properties. However, their development has required years of work and their method of manufacturing remains sharp and requires a good knowledge of impression techniques, composite materials and bonding mechanisms [1-3].
The principle consists in creating a well-adapted, anatomical, functional and aesthetic composite restoration using a model manufactured extemporaneously. This model comes from the impression of cavity preparation [1-3].
a) Restoring substance losses by indirect method finds its indication in the following cases:
b) Dimension of the cavity does not allow the application of a direct technique: the large mass of restoration by the direct technique is not indicated due to the significant shrinkage of the polymerization and the stress at the cavity walls.
c) Multiple restorations by quadrant: easier technique because it requires a single impression avoiding multiple sessions.
d) Aesthetic patient’s request: the large palette of shades associated with layering techniques allows faithful reproductions of the original dental structures.
e) The patient must have good oral hygiene, to avoid any risk of percolation at the joint, knowing that it is a bonded inlay.
f) The tooth must be vital: it is uncertain to indicate this technique on a tooth with a pulpal disorder. In the case of endodontically treated teeth, other therapeutic methods must be used.
g) In bruxism cases, the composite remains the restoration material of choice. Its low hardness compared to the dental structures makes the wear caused by the bruxism takes place at the composite reconstitution and not at the antagonist tooth. Unlike what happens with other materials such as ceramics [4,5].
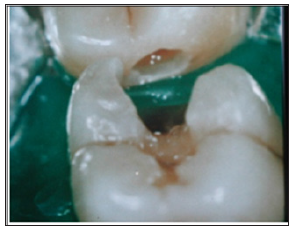
The realization of composite inlays using the indirect technique requires a reasoned dental preparation and a precise impression. The coordination with the laboratory must be worked and honed to facilitate the clinical steps of fitting, bonding under a dental dam, removal of excess bonding material, occlusion control and final polishing. These clinical sequences require great attention, application and some experience to be perfectly mastered. These clinical steps require great concentration, application and some experience to be perfectly mastered [6-8]. The clinical examination of the tooth is completed by vitality tests; the tooth must be vital and without any sign of pulpal involvement. We must proceed to a study of the carious extension on radiogram, to objectify the relation of the decay with the pulpal tissue and the periodontal structures, in case of a proximal lesion (Figure 1). After elaborating a diagnosis, we proceed to a complete elimination of the altered tissues with maximum preservation of healthy tissue (Figure 2). A pre-prosthetic study is then carried out in order to choose the optimal reconstitution material and the optimal technique.
Figure 2: After the setting of the rubberdam, we procede to the removal of the temporary obturation, and the cavity preparation to receive the indirect restoration.
It is important that the future restoration / tooth joint does not coincide with the occlusion impact points. These contacts could cause the deterioration of the joint with hiatus formation, percolation, marginal staining and recurrence of decay. A dental dam is put in place to isolate the operative field. Its utilization is imperative in order to work in a dry and aseptic operating environment. The preparation for the composite inlay is the same as the one in fixed prosthodontics that allow insertion and disinsertion of the inlay. For the sake of tissue economy, only the affected tissue is eliminated during the preparation. The undercuts are filled with dentinal substitute materials such as Glass-ionomer cements or flow composites, with no additional preparation for the healthy dental structures. The accurate impression is made using silicone materials. The impression is made in a single-step with dual-viscosity technique, then sent to the laboratory for casting and realization of the composite inlay. The impression of the antagonist was realized with alginate to allow the reproduction of the occlusion reports (Figure 3).
The preparation is protected with a temporary filling while waiting for the next appointment (Figure 4). The manufacturing of the composite inlay will be done at the laboratory. It will be built up as for ceramics. The stratification built up allows to accurately mimic the optical properties of the natural tooth (Figure 5). The underside of the inlay is treated following these steps:
a. Post lightcuring treatment with heat and light (80 to 140°) in specific containers, with or without nitrogen pressure. This final cooking phase improve the mechanical properties of the composite, its marginal integrity as well as its surface topography. Moreover, this post lightcuring phase increases the conversion rate of the composite. The sanding with 50 m alumina oxide is combined to etching with 5% hydrofluoric acid for one minute, followed by application of a layer of silane to promote the adhesion.
b. Once the inlay is received, we try it in the tooth under a dental dam isolation, any contact with the mouth fluids will cause a readmission of the inlay to the laboratory to resume sanding, etching and silanization treatments (Figure 6).
c. During this step, functional and margins adjustment are done if necessary.
d. The bounding of the inlay is made after treatment of the tooth surface, enamel and dentin etching during 20 seconds, 20 seconds rinsing, drying and application of the 4th or 5th generation bonding system (Figure 7).
e. The chemical treatment of the tooth surface allows an adhesion of the composite by micro-locking in the enamel and the hybrid layer in the dentin by tangling between the adhesive system and the dentin collagen matrix which allows the bonding (Figure 8).
f. For the proximal cavities (Class II- Black, Site 2- Mount & Hume); the use of a matrix system is recommended to avoid any cervical excess (Figure 9).
g. The bonding is assured with a dual flow composite, chemical and light cured composite (Figure 10). The composite is places in the cavity, then the inlay with a slight pressure.
We proceed to the elimination of all the excess of the composite material before the polymerization using a dental probe for the occlusal surfaces and dental floss for the proximal zones. Then we proceed to the polymerization of all the tooth walls, then polishing and finishing using fine diamond burs and disks.
Regular clinical and radiological controls of the inlay are recommended to follow the evolution of the dentin-pulp structures and to appreciate the behaviour of the material over time. Thus, it is possible to detect any marginal deterioration or lack of tightness of the filling (Figures 11 & 12).
The advantages procured by the use of indirect restorations:
a) Minimize the effects of polymerization shrinkage and reduce its stress effects on cavity walls.
b) Polymerizing the composite as a whole, eliminating the risk of remaining free monomers.
c) Better marginal adaptation, better sealing and reducing the risk of hiatus.
d) Better occlusion reports and proximal contacts.
e) Better aesthetic integration
f) And most important point, best mechanical properties during thermal and photonic treatment in the laboratory [9- 12].
Nevertheless, they show many limits such as:
a) The relatively high cost compared to amalgam and composites by direct method.
b) Multiple sessions are needed.
c) In addition, and like all bonding treatments, it is a technique that interesting patients with good oral hygiene and good motivation.
First generation of indirect composite: Touati, Pissis and Morman et al. were the first to develop a technique for aesthetic restorations using first generation composite resins (Kultzer’s Dentacolor ®, Ivoclar’s Isosit®, Visiogem® from Espe ...) [13,14].
These materials have showed good clinical results, but they quickly showed their clinical limitations, resulting in partial and total fractures, marginal joints opening, quick and excessive abrasion and significant colour changes [15,16]. The failure was related to their composition. These first generation laboratory composites were composed by only mineral microcharges with a diameter between 0.04 and 1um. These composite inlays and onlays showed wear fatigue explained by the mastication stress, there is appearance of cracks in the material. These cracks will spread until confluence to give a block out. They thus had a significant fracture rate limiting their use in clinical situations where the material undergoes few flexural stresses [17,18].
Second generation of indirect composite: The clinical failures of 1st generation composites led to the development of improved aesthetic materials for indirect restorations (Targis / vectris ®, Ivoclar, Columbus®, Solidex® from Shofu). The key element in this evolution the adaptation of a microhybrid structure with high charge density which gives the material a better resistance with a better aesthetic rendering and the use of a post-polymerization phase which can be photonic, thermal or a combination of both.
Composition and structure: The increase of the quantity of inorganic charges, associated with the incorporation of macrocharges, has a significant impact on the mechanical properties of the material. the reduced volume of the matrix decreases the shrinkage phenomena in the polymerization and the abrasion with mastication stress. Especially since the particles are silanized to improve their adhesion to the organic matrix and thus reduce the phenomena of wear [11,13,14,29].
Post-polymerization: This post-polymerization phase can be photonic, thermal or a combination of both, with or without nitrogen pressure. This phase has a dual purpose, on one hand, it allows to obtain a high conversion rate (percentage of polymerized composite), on the other hand, it improves the mechanical and optical properties of the material. This technique would allow to reach a degree of conversion close to 100%, which would reduce the internal stress generated by the polymerization shrinkage by appreciably improving the tightness of the restorations.
Fibers incorporation: Some of these second generation systems have known, in addition to the two aforementioned parameters, a fiber incorporation to extend their use to the realization of small bridges. Indeed, the incorporation of fibers increase the mechanical strength of the composite. Different fibers can be used such as glass fiber, carbon fiber, aramid or polyethylene. The Targis / Vectris system from IVOCLAR is one example. It combines Ceromer material (Targis) with glass fiber reinforced material (Vectris) [11,19,20].
The stratification build-up associated to the large choice of composites currently available, allow us to have the same aesthetic properties of the direct and indirect composites. The mechanical properties of indirect inlays are certainly more interesting compared to direct composites, thanks to heat treatments and post polymerization. In addition, the indirect composite inlay offers better control of cervical tightness and better restitution of the contact point in cases of proximal loss of substance. The cost is certainly lower when the restoration is carried out directly in the mouth [19- 24]. As for longevity, clinical studies have shown that there is no significant difference between direct and indirect method inlay.
The main causes of failure are secondary caries, fractures, marginal defects, wear and postoperative sensitivities. A study conducted by the Lasfargues et al. [23] shows that the failures are not related to the material, but a large part is due to the implementation and the respect of the operating stages.
The main causes of failure are secondary caries, fractures, marginal defects, wear and postoperative sensitivities. A study conducted by the Lasfargues et al. [23] shows that the failures are not related to the material, but a large part is due to the implementation and the respect of the operating stages.
The aesthetic integration is the same for the both materials, composite and ceramic. Indeed, the wide range of shades currently available can mimic the tooth in its finest details [24,25]. Thanks to the bonding, composite or ceramic inlay helps strengthen the structure of the decayed tooth, creating a homogeneous structure. The bonding also allows a good marginal adaptation, when the different steps are respected [20]. The stability of ceramics in time is well established, the composite stability depends on the respect of the cooking and polymerization steps, and especially a good final polishing. As for the hardness, the ceramic inlay largely exceeds the composite inlay. It could even cause long-term abrasion of the opposing teeth, reason why the use of the ceramic inlay is not indicated in the presence of parafunctions. The higher cost as well as the difficulty of manufacturing of the ceramic inlay; would tip the balance of the advantages of the composite inlay. Indirect composite inlay remains an excellent alternative, less expensive especially in cases of bruxomania [26,27].
In tribute to Professor Khadija LAHLOU, deceased on June 2016, and contribute in the achievement of this work.


