Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Tarabeih Mahdi*1, Riad Abu Rakia1 and Victoria Gonta2
Received: May 14, 2018; Published: May 30, 2018
*Corresponding author: Tarabeih, Mahdi, Senior lecturer in Nursing Science, Tel Aviv-Jaffa Academic College, Tel Aviv-Jaffa 6818211, Israel
DOI: 10.26717/BJSTR.2018.05.001140
Introduction: Dual Diagnosis is undoubtedly one of the most important and particular problems that mental health services are facing. The common problem of all patients is that is entering in Psychiatric Services due to complications from the use or abuse of legal and illegal substances and at the same time the presence of another psychiatric disorder. The Literature supports the hypothesis that psychiatric disorder and substance abuse disorder coexist more frequently than luck can predict.
Aim: The aim of this study was to examine, assess and compare the characteristics and the psychopathology between patients with dual diagnosis receiving treatment for mental disorders and those receiving treatment for substance use disorders in Substance Use treatment programs in Mental Health Services of Moldova. Furthermore, this study examines the differences in psychopathology in correlation with the alcohol dependence, the duration of treatment and the number of hospital isations in relation with dual diagnosis.
Methods: Three hundred patients (150 of them were dually diagnosed that were, admitted to drug addiction therapeutic and rehabilitation centers for legal and illegal substances and 150 were dually diagnosed were admitted to Psychiatric units in Mental Health Center in Moldova). The Europe ASI the AUDIT, and the PDQ4 were administered individually to each one of the participants. The Statistical Package for Social Sciences (SPSS) version 20.0 was used for data analysis.
Results: Results revealed that the dually diagnosed patients that were admitted in psychiatric units had higher number of diagnosis (mhuM=3.03, duM=2.55, pvalue) higher number of hospitalization in Mental Health Services (mhuM=12.25, duM=7.73) and much more psychological problems (mhuM=63.02, duM=18.78), as well as longer prison time (mhuM=5.55, duM=2.10), compared with those that are entered in Substance Use treatment programs. The mean age of first use for men was 17.88 for psychiatric patients and 17.52 for patients that are entering in Substance Use treatment programs (pvalue=0.001). For women, the mean starting age was 17.50 in psychiatric units and 17.60 in Substance Use treatment programs (pvalue=0.01). The main substance of dependence in most cases was cannabis, followed by cocaine, in both study groups (57.5% of cannabis, 20% of cocaine in psychiatric units and 30% of cannabis, 20% of cocaine in drug Substance Use treatment Programs. 53.4% of people in Substance Use treatment programs had a family history of alcoholism, while the corresponding figure for those in psychiatric units was 46.6%, 50% of both groups had a family history of drug addiction. The patients with anti-social disorder according to the PDQ-4 questionnaire had a higher incidence of alcohol dependence than patients without anti-social disorder. The use of alcohol the last 30 days was associated with an increase in the frequency of alcohol dependency.
Implications for Mental Health Nursing: Results shows that the lack of a specialized treatment centre creates a huge gap for treatment, which leads to Mental Health Services overuse and misuse, and to continuous hospitalisations and relapses, leading dual diagnosis patients to disorganisation and isolation. Mental health specialists should learn and educated in new therapeutic approaches in order to treat dually diagnosed patients holistically.
Keywords: Dual Diagnosis, Drug Addiction, Psychiatric unit, Drug addiction centre, Treatment, Therapy, Psychiatric disorder
The term dual diagnosis includes those individuals who experience drug addiction disorder and co-occurring psychiatric disorders. People with co-existing psychiatric disorders (Axis I or Axis II) and substance use disorder, as well as individuals who experienced both type of disorder during their lifetime is not necessarily simultaneously [1-3]. Dual diagnosis may include any class of mental dis-order that coexists with substance disorder such as post-traumatic stress disorder, anxiety disorder, bipolar disorder, schizophrenia, mania, depression, personality disorder. Usually clinical characteristics are related to the type of psychiatric disorder that is presented by the individual for example many studies have highlighted the relationship between the presence of acute psychotic syndrome and mania and the use of cannabis. The various studies carried out during these decades on population of people that are treated for substance abuse showed that around 50-75% of these individuals presented at the same time some sort of mental disorder (without necessarily being a sever psychiatric disorder) while investigations into populations of people treated for mental disorders recorded rates of 20-50% of these people with coexisting substance abuse [4] The various surveys recorded similar rates of dual disorder in individuals approaching drug treatment regimens [5-11].
Based on everything that has been mentioned above, the intense engagement of mental health specialists, researchers and clinics in recent years with the issue of dual diagnosis is reasonable. It is now common acceptance both on the part of the Mental Health Services and the staff members that there is a lack of evaluation and management of the issue, a lack of services for dually diagnosed patients, lead to a wastage of costs with ineffective provision and there are a lot that needed to be done to enable Mental Health Services to provide a rich therapeutic effect to problems of dual diagnosis and early treatment of consequent problems that affect both the individual as a unit and society as a whole. Within this framework, the need for research on this issue is important. The prospect of investigating dual diagnosis and the characteristics of people with dual diagnosis attempts to explain how this phenomenon affects the therapeutic effect, the course of the disease, the number of infections, and how is generally affects the use of mental health services [11-17].
The purpose of this research, is to explore the characteristics of dually diagnosed patients who approach the Public Mental Health Services in Moldova, examine the differences and similarities of the two group those that are entering in Substance Use Treatment Programs and those that are entering in Psychiatric Units in relation to demographic characteristics, the number of hospitalization, the number of relapses and the frequency of coexistence of these two disorders. Additionally other aims of this research is to explore the relation between the main substance use, the degree of alcohol dependence and the presence of specific mental disorder.
Three Hundred consecutive dually diagnosis patients took part in this study that are receiving treatment either for substance use disorders or for mental disorders in substance use treatment programs, emergency units, psychiatric hospitals and mental health rehabilitation units across Moldova. They were grouped into two categories: mental health service patients (n=150) and substance use treatment program patients (n=150). Dual diagnosis treatment was not provided to any of the participants. The questionnaires EuropASI, AUDIT, SCID and the PDQ-4 were administered individually to each one of the participants by the researcher. The researcher visited the units once a week in order to select and collect the sample for 12 months (from 01/01 / 2014-01 until 01/2015). In psychiatric units, those who had a positive effect on the urological substance detection test were evaluated and were present on the specific day of the visit. In Substance Use Treatment Programs, those who had a history of psychiatric disorder diagnosis based on the psychiatrist’s assessment of the center, after crossing the history with the SCID (Structured Clinical Interview for DSM-IV Axis I Disorder and PDQ-4 Diagnostic Questionaire- version 4) were included in the sample. The sample of the study consisted of those who came to these services for duration of 12 months measured once in the specific period regardless of the time of entry. The study was explained in detail and informed consent was requested in order to continue to the completion of the questionnaires.
a) Participant must be sober during the assessment.
b) Participant must be able to provide data which meet the quality standards necessary for data analysis processes.
c) Participant must not be in a psychological state that puts them or other people in danger
d) Participant must not suffer from any brain damage or any cognitive or mental disorder due to a general medical condition.
e) Participant must be over 18 and under 70 years old.
European Addiction Severity Index – EuropASI [18]. EuropASI is an adaption of the Addiction severity index - ASI 5th Edition [19] for the European population. The purpose of this instrument is to determine the severity of addiction to psychoactive substances. It is a semi-structured interview, containing 30 questions, mainly used for diagnostic purposes and assessment of treatment outcome. The instrument consists of eight domains: general information, medical status, chemical use, employment/support, family/social relationships, legal status, and psychiatric/psychological status [19,20].
EuropASI is considered as a valid and reliable tool for assessing the severity of substance use in psychiatric populations. Test-retest reliability has been reported at 0.89. It has been translated in Greek and used in Moldova as well by trained interviewers [21-25]. In this study, the first domain of EuropASI (General Information) is used for the collection of information regarding the medical and legal history of participants. AUDIT is considered as a valuable, easy-touse, fast, and reliable tool for investigating vulnerable populations and patients with severe co-morbidities of mental disorders and dependence. For these reasons, AUDIT is widely used in both primary prevention and inpatient patients for the early detection of alcohol use disorders [24-28].
The AUDIT questionnaire includes 10 questions, each rated from 0 to 4. Out of a total of 10 questions, three concern alcohol use, four for the addiction and three for the problems that the use of alcohol caused. Overall rating ≥8 is indicative of a problem of alcohol abuse, with scores higher than 15 suggesting dependence, according to the manufacturer’s instructions [28,29]. The translation of AUDIT done in Greek by the English original, by two bilingual psychiatrists and by reverse translation. Studies has showed high Internal affinity reliability (Cronbach a) was 0.78 for controls and 0.79 for patients. AUDIT has an increased internal affinity value and high validity with respect to clinical criteria, as well as high sensitivity and specialization
The study falls on bioethical and ethical issues and it was necessary to observe the code of confidentiality and the patient’s written consent for participation, as well as the appointment of a person to control the research process by the Committee for the Protection of Mental Patients. For these reasons, the Moldova Bioethics Committee and the Commissioner for Personal Data Protection for the protection and safeguarding of patients’ personal data, as well as the Research Committee of the Ministry of Health of Moldova, have been asked for permission to conduct the study. Subsequently, once the above procedures have been completed all the units under investigation were informed by the Director of the Mental Health Services about the authorization to conduct the study. Before participating in the study, participants signed a consent form. Anonymity and confidentiality were the basic principles of this study.
The Statistical Package for Social Sciences (SPSS) version 20.0 was used for data analysis. Descriptive statistics were used for demographic characteristics and t-test was used to determine the differences in psychopathology between patients in mental health services and patients in substance use treatment programs. Furthermore, logistic regression analysis was conducted in order to determine factors affecting psychopathology.
Results revealed (Tables 1 & 2) that the men that were entering in Substance Use Treatment Programs were more (51,5%) in comparison with the men that were entering in Psychiatric Units (48,5%). The women that were entering in Psychiatric Units were more (55,4%) than the women that were entering in Substance Use Treatment Programs (44,6%). In Psychiatric Units the patients were single (54,8% ) in correlation to the patients that were entering in Substance Use Treatment Programs that the majority of them were divorced (59,3%). The majority of the patients that were entering in Psychiatric Unit were living with their parents (54,1%) in comparison with those that were entering in Substance Use Treatment Programs that were less (45,9%) and the majority of them were living with sexual partner without children (76,20%).
According their education level the majority of the patients that they were entering in Psychiatric Units they stopped school (57,1%) in comparison with those that were entering the Substance Use Treatment Programs (42,9%). The age that they stopped school was 13.3 years old for those that they were entering in Psychiatric Units and 13.9 years old for those that were entering in Substance Use Treatment Programs. According their job status patients that were entering in Psychiatric Units (60,3%) were without job in comparison with those that were entering in Substance Use Treatment Programs That were only (39,7%) without job, with the majority of them to have full time job (81.0%) in comparison with those that were entering in Psychiatric Units that were only (19 %). The main source of money for the patient that were entering in psychiatric units were the social insurance allowance pension (66,7%) in comparison with the patient that were entering in Substance Use Treatment Programs that their main source of money seems to be firstly their personal job (80,4%) in comparison with those that were entering in psychiatric units (19,6%).
According the patients family history the 46.4% of drug addicts had a family history of an alcohol use/drug use /psychiatric problem, and 53.6% of those in psychiatric units. More specifically, those in psychiatric units had a greater family history of psychiatric problems (71.4%) than those in Substance Use Treatment Programs (28.6%), In addition, 53.4% of them had a family history of alcoholism, while the corresponding figure for those in psychiatric units was 46.6%. 50% of both groups had a family history of drug addiction. 72.7% of people with a family history of gambling addiction were in Substance Use Treatment Programs, while 27.3% of these individuals were in psychiatric units (Table 3).
The Table 4 below shows the patient’s score in the AUDIT questionnaire. For the majority of the sample, both groups (psychiatric unit and drug addicts) scores in the AUDIT questionnaire were slightly different. Specifically 49.6% of psychiatric patients had a score of 0-7 (physiological status), while the corresponding percentage for people in Substance Use Treatment Programs was 50.4%., 51.9% of people in psychiatric units had a score of 8-15 (a problem), while the proportion of those in Substance Use Treatment Programs was 48.1%, 49.6% of people in psychiatric units had a rating of 16-40 (dependence), while the corresponding percentage for people in Substance Use Treatment Programs was 50.4%. The association between Type of Unit and severity of psychiatric disorder, the severity of dependence and treatment rates, were investigated by using Logistic Regression analysis (Table 5,6). The results revealed that patients with severe psychiatric illness were more likely to enter in a psychiatric unit than patients without severe psychiatric illness. The increase in the severity of dependence was associated with an increase in the frequency of admission to Substance Use Treatment Programs. The increase in treatment rates in a psychiatric hospital / clinic was associated with an increase in the frequency of admission to a psychiatric unit. The patients that enrolled following a court or a police order were imported to a greater extent in a psychiatric unit than patients imported without a court or a police mandate. The variables account for 82% of the variability of admission to a Substance Use Treatment Program or psychiatric unit.
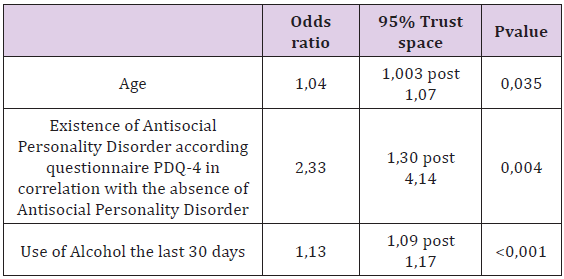
Table 6: Multivariate Logistic Regression Analysis according the degree of alcohol dependence by using the AUDIT questionnaire (score 0-7 = reporting category).
The research according the differences between the two groups revealed that the men had a higher representation in the sample (51.5%) in Substance Use Treatment Programs as opposed to the women with the highest number of those who were admitted to the Psychiatric Units (55.4%). In a survey conducted at US Psychiatric Hospitals, where patient records were investigated for alcohol or illicit drug use during 2003-2007, it was found that the dual diagnosis rate was higher in women (54.6%) than in men (38.4%). A research by Wu et al. [9], it was revealed that patient with a dual diagnosis were more likely to be men. The group of patients enrolled in psychiatric units was more often single (54.8%) with a large percentage living together with their parents (54.1%), as opposed to the group of patients in Substance Use Treatment Programs the largest proportion was divorced (59.3%).
Similar results were also found in other investigations as in the Picci et al. [12], where the participants were aged 18-44, free or divorced and widowed, the same research by Rady et al. [13] revealed that the majority of the sample (63%) was single, with low socio-economic and educational level. Also the national survey by Magidson et al. [22], typically indicate that people with double diagnosis were more likely to be divorced / deprived, in the absence of a supportive environment. The above finding may be related to the fact that in Moldova, individuals with dual diagnosis are usually marginalized in the absence of social life and cohabitation. At the same time, the beginning of substance abuse at a young age makes them trapped in a permanent state of lack of maturation and emotional development and assuming personal responsibility and establishing relationships. This correlation needs further research in the future. The majority of people in psychiatric units had primary education at elementary school (58.6%), and more often, they were interrupted by school (57.1%) with an average age of 13.3 years.
The low level of education in this research is supported by other European studies where the presence of dual diagnosis was higher in patients with low socio-economic and educational background, usually with chronic education of less than 9 years [13,30- 34]. The majority of the sample included in the psychiatric unit was in the group of inactive (60.3%), with the main source of income for the pension or sickness benefit (66.7%). In contrast to people who were in Substance Use Treatment Programs where the majority had the main source of income illegality (56.9%). The unemployment rates of the current survey are at the same level as unemployment rates in dual diagnosis population in Europe, where dual - diagnosis surveys often show instability in the place of residence and high levels of unemployment [31, 35-38].
For the majority of the sample, both for psychiatric patients and for those in Substance Use drug addiction treatment centers, the AUDIT questionnaire score showed slight differences in all sub-scales. The results showed the use of alcohol (from 0 to 7), a slightly higher percentage of use among patients in psychiatric units (50.4%), the same for alcohol abuse (from 8 to 15), the percentages (51.9%) and alcohol dependence (16 to 40) were slightly higher for the group of patients in Substance Use Treatment Programs (50,4%). Several surveys that carried out in the European area confirm the results of the association between abuse and alcohol dependence with the presence of dual diagnosis with a first example of Liang & Chikritzhs [39], which reported that patients with disorders mood and anxiety disorders faced an increased risk of developing alcohol abuse or alcohol dependency compared to people without mental disorders. The risk of alcohol dependence was even higher for newly diagnosed patients (over 5 years of research) with mental disorder, especially when they were patients with bipolar disorder. In addition, this study showed that generalized anxiety disorder had a greater correlation with the risk of developing alcohol dependence, while social phobia and posttraumatic stress disorder had a greater correlation with the risk for alcohol abuse disorder. From the existing literature, it also appears that the use of alcohol for self-medication in patients with anxiety disorders is an important risk factor for the development of alcohol dependence disorder.
The percentages of patients with dual diagnosis that were in psychiatric units and had a family history of an alcohol / drug / psychiatric problem (53.6%) were higher. More specifically, those in psychiatric units had a greater family history of psychiatric problems (71.4%), while the percentage of people in Substance Use Treatment Programs and family history of alcoholism (53.4%) was higher, 50% of both groups had a family history of drug addiction, and higher percentage of family history of gambling addiction for the patients that are entering in Substance Use Treatment Programs (72,7%). The same results shows the research of Gregg, Barrowclough, & Haddock (2007), saying that the family history of Substance Use Disorder can be considered as a predictor factor for the coexistence of Substance Use Disorder among the Schizophrenic patients. Other researcher support that the rate of parallel occurrence of alcoholism and dependence on psychoactive substances is particularly high. Percentages ranging from 30% to 51% of psychoactive substances add to alcohol dependence or are dependent on it, while relatives of alcoholics often have problems of abuse of other substances or vice versa [40,41].
Regarding the number of imports small differences were found between the two groups of patients with those that were in psychiatric units having an average number of imports equal to 2 and respectively the group of patients that were in Substance Use Treatment Programs having an average number of imports equal to 1, 7 during the year. Contrary to the number of imports during that year, people in Substance Use Treatment Programs had a higher average import (9,2) imports than those in psychiatric units (7,6). In addition, those in psychiatric units had a higher average number of hospitalizations for psychological / emotional problems (4.3) and a higher average (67.8 days) for treatment days for psychological problems as outpatients. Those results are supported from the findings of recent research shows that drug use affects the number of relapses, hospitalizations for hospitalization, treatment time, and the possibility of completing the treatment of patients with double diagnosis [3,9,11,12,17,42-44].
More specifically, Zammit et al. [42], through a systematic review of research, concluded that in people with psychotic disorders the use of cannabis increases the incidence of recurrences and admissions for hospitalization while reducing the chances of completing treatment. Similar results came from the research by Batalla et al. [11], which revealed that cannabis use and cocaine use increase the probability of re-admission for hospitalization to people experiencing psychotic episodes, especially during the first five years after the first psychotic episode.
The logistic regression analysis shows that the age was positively associated with the frequency of alcohol dependency. Older people had an increased frequency of alcohol dependence, possibly related to the fact that people start using alcohol at an early age, are then led to alcohol abuse, and with the passage of time the dependence on alcohol. At the same time people who show alcohol dependence are people who are using alcohol abuse for years that alcohol dependence can last for years and the individual is in a service for assistance at an advanced age for those people who are part of programs treatment of alcohol dependence are usually older. Moreover patients with antisocial personality disorder had a higher frequency of alcohol dependence. This finding that alcohol dependence is related to the presence of antisocial personality disorder is consistent with the findings of Torrens, Gilchrist, Domingo- Salvany, and the psyCoBarcelona Group [45] who report that the majority of participants met the criteria for more of dependence disorders during their lifetime and the most common dependency disorders observed were dependence on heroin, cocaine, alcohol and sedatives.
At the same time, 41.8% of participants experienced even a mental disturbance of Axis I during their lifetime, with mood disorders, anxiety disorders and antisocial or borderline / borderline personality disorder more frequent. Dual Diagnosis patients who have been drinking alcohol for the last thirty days before entering Mental Health Services have also had an increased incidence of alcohol dependence with pvalue <0.01. The research by Ding et al. [46] agrees with the above finding, arguing that the major drug use disorders in dual diagnosis patients who came to treatment in drug addiction treatment programs in US public hospitals were withdrawal syndrome, withdrawal syndrome from illicit psychoactive substances, other chronic undetermined alcohol dependence disorders and chronic opioid dependence disorders. Alcohol appears to be one of the main substances of dependence among individuals with dual diagnosis.
The problem of dual diagnosis is more common in Mental Health Services over the last few years, making it a top priority to provide appropriate treatment for both the clinical and the mental health policy makers. This phenomenon has also been strongly observed in Moldova during the last fifteen years, with a great deal of concern for the clinicians regarding the way of treatment and clinical evaluation. For dual diagnosis treatment in Moldova we have Public and Private Substance Use Treatment Programs and all cases that are entering in those programs are upon request of the patient and only in Public Psychiatric Units such as In Psychiatry Hospital the patients are admitted involuntary and under the pressure of the law. According to experts, at the clinical level, people with a dual diagnosis need treatment that is addressed in parallel to both coexisting disorders. The reality is that most of the under investigation services treat one disorder as a secondary one without setting therapeutic targets for the secondary disorder, resulting in frequent relapses due to lack of proper treatment and management. So this create the need for proper and extensive assessment of the dual diagnosis patients in the initial phase of treatment, while key types of treatment are psychosocial interventions, opioid substitution therapy, physical detoxification, treatment of psychopathology symptoms and co-treatment of both disorders in dual diagnosis treatment units [47-50].
This research is the first attempt to evaluate and investigate dual diagnosis in the Mental Health Services in Moldova, setting the basis for further research efforts as well. On a first level we were a identified the special characteristics of dual diagnosis patients that are approaching the investigated services as well as the usual mental disorders they present, the symptoms of psychopathology and in general, we made an attempt to outline the profile of dual diagnosis patients that are entering to the Mental Health Services of Moldova as well as its particular needs in terms of both personal, social, family, psychological, substance use history as well as dependence and web presence abuse. Subsequently, further investigation is needed on issues like how the family environment affects the development of those individuals and their disorder as well as the investigation if the treatment is related to the presence of dual diagnosis, whether the absence of supportive environment exacerbates disturbance and increases their imports into these services, or whether or not medication is helping to treat the symptoms of psychopathology that these people are facing.
The need to investigate the particular conditions of development of these individuals as well as the expression of their personal experiences in relation to the development of their disorder is something that will add to the clinical evaluation and treatment of these individuals. During this research the patients have the opportunity for an active participation through focused interviews that they expressed their own thoughts, opinions and feelings about the services provided and what they themselves consider as ancillary or not, are useful information for those that are involved in policy- making on the issue of addressing substance abuse and mental disorder in general, as it would be the trigger for creating treatment programs that respond on the specific needs of dual diagnosis patients.
Moreover this research revealed the need for the implementation of a strategy that will strengthen the continuous care as well as communication between Mental Health Services in order to support mentally and physically dually diagnosed patients, give the right treatment and phase the problem of readmissions and minimize the problem of relapses. Persons entering compulsory psychiatric hospitals need to be subsequently linked to drug addiction programs to continue their treatment. A clear assessment framework with specific assessment tools, weighted, valid and reliable, will help to a large extent measure both the size of the problem and the appropriate treatment. Applying a clear single treatment policy with clear treatment contracts and a study of a unitary setting that will specialize in addressing individuals with dual diagnosis with distinct goals for both the patients themselves, their supportive system and the staff themselves health and other stakeholders would greatly contribute to timely and immediate treatment as well as to reducing the cost of the Services provided.


