Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Nina Mahne*1, Natalia Lipskaia2, Andreas Lunacek1, Badereddin Mohamad Al-Ali1 and Eugen Plas1
Received: May 04, 2018; Published: May 14, 2018
*Corresponding author: Nina Mahne, Department of Urology, Hanusch Krankenhaus, Heinrich-Collin-Strasse 30, A-1140 Vienna, Austria
DOI: 10.26717/BJSTR.2018.04.001067
Cystic lymphangiomas of the adrenal gland are rare, benign lesions of vascular origin with lymphatic differentiation. Most of these lesions are discovered incidentally during radiological imaging studies, surgery or autopsy. As radiologic techniques have improved, adrenal cysts are discovered more often. We present a 49-year-old woman who was referred to our hospital with a growing cystic mass located in the left suprarenal space causing left flank pain. The lesion had previously been described as a simple left renal cyst observed by ultrasound follow-up studies. Further characterization by magnetic resonance tomography (MRT) displayed a 7.0 x 4.0 x 4.6 cm left adrenal septated cyst. A hormonesecreting tumor was excluded. An organ-sparing left laparoscopic adrenalectomy was performed. Histopathological examination revealed a benign cystic lymphangioma of the left adrenal gland. The lining cells showed strong immunoreactivity for CD31 and D2-40 (podoplanin). Diagnostic features and surgical treatment of an uncommon lesion are discussed.
Keywords: Adrenal Gland, Adrenal Cyst, Lymphangioma, Laparoscopy, Adrenalectomy
Cystic lymphangiomas of the adrenal gland are very rare, benign vascular malformations originating from the lymphatic system [1]. The majority of these cystic masses are clinically asymptomatic and therefore mostly discovered incidentally during radiologic imaging, abdominal surgery or at autopsy [2,3]. Preoperative diagnosis is challenging. Although radiological imaging has improved and is able to characterize the cystic nature of the lesion, it fails to prove a specific diagnosis. Definitive diagnosis can only be performed histologically with additional immunohistological evaluation. Further investigations are recommended for all adrenal incidentalomas including accurate clinical, radiological and endocrinological examinations [4]. Hormonal evaluation can be helpful in identifying functional cysts but cannot distinguish non-functional cysts from lymphangiomas. Small asymptomatic non-functioning and unsuspicious adrenal cysts can be observed by follow-up studies. Indications for surgical removal involve large cysts (≥5cm), functional cysts, symptomatic cysts and cysts at risk for rupture, hemorrhage and infection and certain radiological findings. The letter includes high density (>10 HU) on unenhanced computed tomography (CT), delayed was-out of the contrast medium, significant growth of the cyst in follow-up images [5]. Cystic lymphangiomas of the adrenal gland are in rare cases subject of investigation, therefore only few cases are reported in literature. Here we describe a case of a female patient diagnosed with a cystic mass first discovered by ultrasound and incorrectly diagnosed as a renal cyst. Due to a constant increase in size revealed by followup studies, MRT was performed, demonstrating a large left adrenal cyst.
A 49-year-old woman with a history of follow-up examinations due to a growing cystic mass in the left suprarenal fossa was referred to our hospital for treatment of a complex cyst of the left adrenal gland. The lesion was first discovered by abdominal ultrasound in 1998 with a size of 3.5 cm and had grown to a diameter of 3.8 cm in a follow-up examination in 2000. Both findings were reported as simple cysts in the upper pole of the left kidney. In 2013 the lesion was showing further growth on ultrasound measuring 4.2cm and had been characterized as complex cystic mass due to the presence of septations and partially thickened walls. Additional radiological investigations were initiated. MRT demonstrated a 7 x 4 x 4.6 cm left adrenal cystic mass showing thin septations (Figures 1 & 2). At that time the patient presented with left flank pain, physical examination was normal. Laboratory evaluation of adrenal function revealed unremarkable values.
Figure 1: Coronal T2-weighted MRT image revealing a large well-defined cystic mass in the left suprarenal fossa showing high signal intensity.
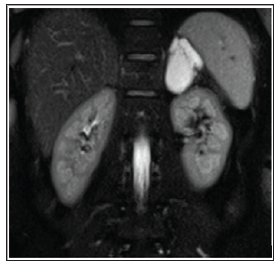
Figure 4: Histopathologic specimen showing characteristic architecture with multiple irregular shaped cystic spaces lined by flattened epithelium lacking cytologic atypia. Immunohistochemically these cells stained positive for (A) CD31 and (B) D2-40 (podoplanin).
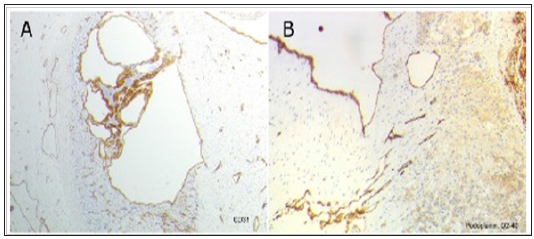
As the cyst demonstrated septations and had been growing constantly to a large size (> 5 cm) and was causing symptoms, the decision for excision was made. In May 2014 an organ-sparing left laparoscopic adrenalectomy was performed (Figure 3). Pathologic examination demonstrated partial multiple cystic formations among normal tissue. Cystic walls were intact, smooth and had two chambers, each 2 cm in diameter. Microscopically the walls of the multi-chambered cysts were laid with thin-walled endothelial cells. Immunohistologically these cells stained positively for CD31 and D2-40, podoplanin (Figure 4). Therefore a benign cystic lymphangioma of the left adrenal gland was diagnosed histologically. Postoperatively the patient recovered without complications. No further follow-up studies are necessary.
Adrenal cysts are rare lesions with an incidence of approximately 0.06% in autopsy studies [6]. The majority of these lesions are discovered incidentally during imaging examinations, surgery for unrelated reasons or at autopsy [2,3]. Lymphangiomas can occur at all ages, but are most frequently revealed between the third and sixth decade of life with a female, right-sided predominance. Approximately 95% of all lymphangiomas are located in the neck and head or axillary region, as well as the mediastinum. The remaining 5% occur in the abdominal cavity including the mesentery of small intestine, omentum, mesocolon and retroperitoneum [7]. Although cystic lymphangiomas may grow to a remarkable size, they remain asymptomatic in the majority of the reported cases. Symptoms may be gastrointestinal disturbance, fever, abdominal, back or flank pain or a palpable mass related to size and location of the tumor [3,7].
The majority of adrenal cysts are benign and nonfunctional [8]. Further investigations are recommended for all adrenal incidentalomas including accurate clinical, radiological and endocrinological examinations [4]. Hormonal evaluation is helpful in identifying functional cysts but cannot distinguish nonfunctional cysts from lymphangiomas. Preoperative diagnosis is challenging. Although radiological imaging has improved and is able to characterize the cystic nature of the lesion, it fails to prove a specific diagnosis. Definitive diagnosis can only be performed histologically with additional immunohistological evaluation. Differential diagnosis includes cystic benign and malignant adrenocortical neoplasms, adrenal solid tumors with cystic change, cystic metastasis, pheochromocytoma with cystic change, pseudocysts, hemorrhage and infection including echinococcal cysts [1,7]. The suspicion on ultrasound is based on the presence of a well-marginated, anechoic cystic lesion, typically located in the suprarenal area. The lesions appear anechoic. Septations between the loculi are usually thin [1,2].
CT visualizes a non-enhancing mass with smooth borders and thin walls. It may show enhancement of the cyst wall or septa. The fluid component typically appears homogenous with low attenuation values similar to water density, or occasionally higher if hemorrhagic or protein component is present. On MRT unsuspicious adrenal cysts present homogenous with low signal intensity on T1-weighted imaging and high intensity on T2- weighted imaging without substantial internal enhancement. Complicated cysts demonstrate high signal intensity on T1- and T2- weighted images [2]. Cystic lymphangiomas of the adrenal gland are benign vascular malformations originating from the lymphatic system [1]. So far, the pathogenesis is not completely understood. It is hypothesized that these lesions origin from continued growth of ectopic or malformed lymphatic tissue or arise from a hyperplastic reaction to inflammation or a lymphatic hamartoma.
Furthermore it has also been discussed, that impairment of lymphatic drainage, proximal dilatation of the lymphatic system and traumas cause these lesions [7,9]. The characteristic histological pattern is an intra-adrenal, well-defined multilcystic mass composed of irregular dilated, thin-walled channels lined by bland, flattened, attenuated endothelial cells that contain significant amounts of connective tissue, lacking cellular atypia. These cystic spaces are empty or may contain acellular, homogenous protein-aveous material with occasional calcification and lack blood, cholesterol clefts, blood cell content, mucus or necrotic debris. The endothelium is surrounded by normal appearing adrenal parenchyma [7,10]. Immunohistochemistry can be helpful confirming the diagnosis. The endothelial lining reacts with CD 31, CD34 and furthermore with D2-40 (podoplanin) which is a specific marker of lymphatic endothelium [7]. Surgical excision by adreanlectomy is recommended in literature with excellent prognosis and no evidence of recurrence [10].
Small asymptomatic non-functioning and unsuspicious adrenal cysts can be managed conservatively by follow-up imaging series [5]. Benign imaging features of adrenal cystic lesions include thin wall, small size, well demarked border and homogenous hypodensity [2]. Indications for surgical removal involve large cysts (≥ 5 cm), functional cysts, symptomatic cysts and cysts at risk for rupture, hemorrhage and infection and certain radiological findings. The letter include high density on unenhanced CT (>10 HU), delayed was-out of the contrast medium, significant growth of the cyst in follow-up images [5]. Adrenalectomy can be performed by an open surgical approach, however most authors as well as our department prefer laparoscopic excision. In the case of our patient we were able to remove the cystic lesion in toto by an organ-sparing laparoscopic surgery. Laparoscopy is a safe and effective minimally invasive approach and provides clear advantages over open surgery regarding analgesia, hospitalization, blood loss, cosmetics and complication rate


