Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Yang Yuan Chen*1, Cheng Che Chen1 and Yung-Fang Chen2
Received: April 04, 2018; Published: April 13, 2018
*Corresponding author: Yang Yuan Chen, China Medical University, China Medical University Hospital 3 Lane 138 Tai-An 2nd Street Changhua, 500 Taiwan
DOI: 10.26717/BJSTR.2018.03.000961
Abbreviations: RFA: Radiofrequency Ablation; HCC: Hepatocellular Carcinoma; CT: Computed Tomography
Radiofrequency ablation (RFA) is a novel technique that is being used to treat hepatic lesions with an increasing frequency. Complications with this rapidly spreading technique will be increase and shall be more careful after RFA. We report a case of hepatic pseudoaneurysm after RFA for hepatocellular carcinoma treatment.
A 75-year-old man presented to the emergency room with acute right upper quadrant pain and without orthopnea or peripheral edema. The patient received regular follow-up, and his medical history revealed postoperative hepatocellular carcinoma (HCC) at 3 years. An abdominal echo revealed a hyperechoic nodule of 1.1 cm over segment 8 of the right side of the liver (Figure 1). Multilphase contrast-enhancement Computed tomography (CT) showed a typical HCC pattern. On admission, his laboratory values were as follows: alanine aminotransferase, 21U/L; alkaline phosphatase, 120U/L; and a-fetoprotein, 3.61ng/ dL. The patient was negative for serum hepatitis B surface antigen and hepatitis C antibody, and a hepatic nodule biopsy revealed HCC [1]. He received radiofrequency ablation (RFA) for recurrent HCC; however, he suddenly experienced acute right upper quadrant pain 1 week later. A B-mode ultrasound revealed a cystic lesion with arterial waveform (Figure 2), and color Doppler ultrasound findings showed arterial flow (Figure 3). Arterial phase CT revealed a hepatic arterial pseudoaneurysm (Figure 4) arrow and mild contrast medium extravasation, which was confirmed by emergent angiography (Figure 5) arrow. Transhepatic arterial embolization was performed using a coil to achieve complete embolization, arrow [2]. Recovery was uneventful, and the patient was discharged 2 days after embolization.
Figure 1: An Abdominal Echo Revealed a Hyperechoic Nodule of 1.1cm Over Segment 8 of the Right Side of the Liver.
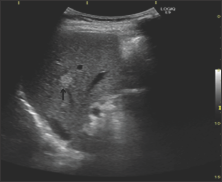
Figure 2: A B Mode Ultrasound Revealed a Cystic Lesion with Arterial Waveform.
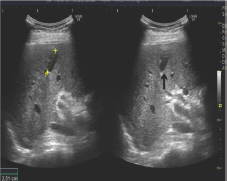
Figure 3: Color Doppler Ultrasound Findings showed Arterial Flow.
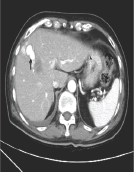
Figure 4: Arterial Phase CT Revealed a Hepatic Arterial Pseudoaneurysm.
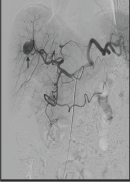
Figure 5: Mild Contrast Medium Extravasation, which was confirmed by Emergent Angiography.

RFA has been confirmed as an effective and safe therapeutic option for treatment in primary and secondary hepatic neoplasms. The major and minor complication rates ranged from 2.2% to 3.1% and 5% to 8.9%, respectively. RFA-induced hepatic vascular damage, including portal vein thrombosis, hepatic artery rupture, and pseudoaneurysm, is very rare. A pseudoaneurysm caused by RFA may arise from the hepatic artery or the portal vein. Pseudoaneurysms after RFA mainly arise because of thermal or mechanical injury. Thermal injuries seldom cause vessel damage because of the cooling effect of the blood flow [3]. The most likely cause of pseudoaneurysms after RFA is mechanical injury during needle insertion. In our case, the pseudoaneurysm and HCC were detected in different segments of the liver; the pseudoaneurysm was identified at the RFA needle track.
Therefore, we believe that the pseudoaneurysm is secondary to vessel damage during needle insertion. Hepatic pseudoaneurysm can be easily identified using multiphase contrast-enhancement CT, color Doppler ultrasound imaging, or angiography. Typically, CT images provide accurate assessments of the therapeutic response and any complications after RFA. Many cases have been diagnosed by CT during follow-up. In our case, color Doppler and B-mode ultrasound imaging procedures were used for initial diagnosis, which easily identified that the pseudoaneurysm originated from the hepatic artery and not from the portal vein. In addition, multiphase contrast-enhancement CT confirmed the diagnosis. Hepatic artery pseudoaneurysms have high rupture and mortality rates (44% and 82%, respectively) and can be treated surgically or by transhepatic arterial embolization. In our case, transhepatic arterial embolization was performed using a coil because it is a minimally invasive procedure and yields optimal results.


